- President Biden Signs Inflation Reduction Act into Law – Includes Critical Medicare Prescription Drug Provisions
- Additional New Coverage News – Hearing Aids and Oral Health
- Nursing Home Trade Group Asks for New Waiver of Nurse Aide Training Requirements
- Report: Nursing Home MA Issues Survey
- Free Webinar | Medicare Enrollment Matters
- Discover How We Can Protect & Improve Medicare Together
President Biden Signs Inflation Reduction Act into Law – Includes Critical Medicare Prescription Drug Provisions
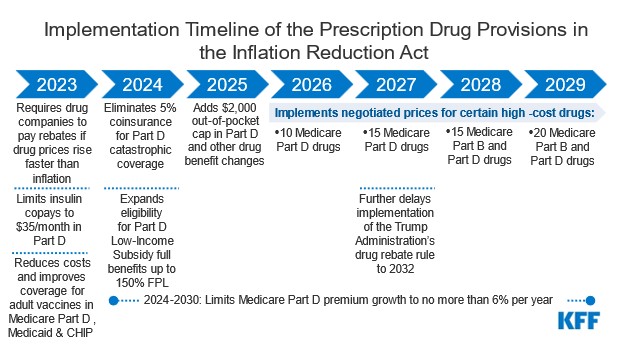
On Tuesday, August 16, 2022, President Biden signed into law the Inflation Reduction Act (IRA) of 2022, which includes expansive health and climate provisions. This bill is the culmination of over a year of debate about a wide range of proposals, including an extensive expansion of Medicare benefits. While the final bill includes only prescription drug provisions relating to Medicare, these provisions by themselves are a historic step forward concerning the price of prescription drugs and will be of significant benefit to Medicare beneficiaries.
Among other things, the IRA will:
- Allow Medicare to negotiate with drug manufacturers for the price of some Part D and Part B drugs (starting in 2026);
- Cap beneficiary out-of-pocket Part D drugs costs at $2,000 per year (starting in 2025; in 2024, the 5% coinsurance for Part D catastrophic coverage will be eliminated);
- Impose checks on the annual rise in costs of drugs and Part D premiums (limitations on drug prices start in 2023, and limitations on Part D premiums start in 2024);
- Limit monthly out-of-pocket copays for insulin to $35 (starting in 2023); and
- Expand access to the Part D low-income subsidy (“Extra Help”) (starting in 2024).
For a more detailed analysis, see this Kaiser Family Foundation report titled “What Are the Prescription Drug Provisions in the Inflation Reduction Act?” (Aug. 11, 2022) and this article in Health Affairs Forefront titled “Understanding The Democrats’ Drug Pricing Package” by Rachel Sachs (Aug. 10, 2022).
The Center for Medicare Advocacy applauds Congress and President Biden for taking these considerable steps in improving prescription drug coverage for Medicare beneficiaries.
The following implementation timeline of the prescription drug related provisions of the IRA is reproduced from materials from the Kaiser Family Foundation (found at the above link):
Additional New Coverage News – Hearing Aids and Oral Health
The Inflation Reduction Act of 2022 (IRA), just signed into law (as discussed in this CMA Alert will provide important new prescription drug savings for beneficiaries. In addition, the Administration has taken other steps to fill some other coverage gaps.
Over-the-Counter Hearing Aids
Although Medicare coverage was not expanded to include coverage of hearing aids, there has been positive movement on hearing coverage, many years in the making. Following legislation passed in 2017, and an Executive Order issued last year instructing the Food and Drug Administration (FDA) to issue long-delayed regulations, on August 16, 2022, the FDA announced a final a rule that will soon lead to the availability of over the counter hearing aids.
The rule will, as described by the Washington Post (8/16/22), “create a new category of hearing aids that supersede state-level regulations requiring patients to visit physicians or audiologists to get prescriptions and fittings. The devices will be available for individuals 18 and older with mild to moderate hearing loss at pharmacies, stores and online.” As noted by Inside Health Policy (8/16/22), “[h]earing aids that do not meet the requirements for the OTC category, for example because they are intended for severe hearing impairment or users younger than 18, are still considered prescription devices.”
Further, notes the Post, “[t]he change is expected to significantly benefit older adults — individuals who are most likely to experience hearing loss and to be on a fixed income — as well as those in poor and rural communities that have fewer audiologists.” According to a statement released by the White House, this action “deliver[s] nearly $3,000 in savings to American families for a pair of hearing aids and giv[es] people more choices to improve their health and wellbeing.”
The final rule was published in the Federal Register on August 17, 2022 “Regulatory Requirements for Hearing Aid Devices and Personal Sound Amplification Products; Guidance for Industry and Food and Drug Administration Staff; Availability” 87 Fed Reg 50568 (Aug. 17, 2022).
Oral Health Services
While broad coverage for dental services has not been expanded to all Medicare beneficiaries, the Centers for Medicare & Medicaid Services (CMS) recently issued a proposed rule, currently open for comment (until Sept. 6, 2022), that includes a proposal to broaden reimbursement for medically necessary dental services.
Nursing Home Trade Group Asks for New Waiver of Nurse Aide Training Requirements
In an August 9, 2022 letter, the American Health Care Association asked HHS Secretary Xavier Becerra to reinstate the 1135 waiver on nursing aide training requirements for nursing homes that expired more than two months ago.[1] The Center for Medicare Advocacy strongly opposes this request and urges the Centers for Medicare & Medicaid Services (CMS) to firmly and quickly say no.
In March 2020, at the beginning of the COVID-19 pandemic, CMS waived the federal statutory requirement that facilities not use individuals as nurse aides for more than four months unless they had completed a nurse aide training program.[2] However, CMS did not waive the statutory requirement that aides pass their state’s competency evaluation program.
AHCA immediately created a free eight-hour on-line training program for a new staff position, which it called temporary nurse aides (TNAs).[3] Many states accepted TNAs, with limited training, as workers during the pandemic.[4]
In April 2021, CMS advised that when it lifted the waiver of nurse aide training requirements, aides would have four months to complete their states’ required training. However, CMS simultaneously suggested that “states evaluate their NATCEP [nurse aide training and competency evaluation program] and consider allowing some of the time worked by the nurse aides during the PHE to count toward the 75-hour training requirement.”[5] The Center expressed concern at the time that CMS was signaling that states were free to undermine longstanding statutory nurse aide training requirements, in anticipation of the end of the public health emergency.[6] This gratuitous offer to states and nursing homes was especially troubling when CMS did not know how many people were working as TNAs and what proportion of the aide workforce they actually represent, what kind of training and how much training they received, who provided the training, where they work, and which specific CNA tasks they perform and how well (or inadequately) they perform those assignments.
CMS finally lifted the nurse aide training waiver on April 7, 2022, effective in 60 days.[7] The waiver is no longer in effect. The Center for Medicare Advocacy urges CMS not to reinstate it.
___________________
[1] Letter from AHCA President and CEO Mark Parkinson to HHS Secretary Xavier Becerra, https://www.ahcancal.org/News-and-Communications/Fact-Sheets/Letters/AHCA-NCAL-Letter-HHS-Aug2022.pdf
[2] 42 U.S.C. §§1395i-3(f)(2), 1396r(f)(2), Medicare and Medicaid, respectively (federal rules). States’ programs must comply with these federal standards, 42 U.S.C. §§1395i-3(e)(1), 1396r(e)(1)
[3] AHCA, Temporary Nurse Aide Training & Competency Checklist (website no longer available to the public)
[4] See “Who’s Providing Care for Nursing Home Residents? Nurse Aide Training Requirements during the Coronavirus Pandemic” (CMA Report, Jul. 23, 2020), https://medicareadvocacy.org/wp-content/uploads/2020/07/Report-Nurse-Aide-Training.pdf
[5] CMS, “Updates to Long-Term Care (LTC) Emergency Regulatory Waivers issued in response to COVID-19,” QSO-21-17-NH (Apr. 8, 2021), https://www.cms.gov/files/document/qso-21-17-nh.pdf
[6] See “Who Provides Care for Nursing Home Residents? An Update on Temporary Nurse Aides” (CMA Alert, Sep. 15, 2021), https://medicareadvocacy.org/special-report-update-on-tnas, and (CMA Report, Sep. 15, 2021), https://medicareadvocacy.org/wp-content/uploads/2021/09/SNF-TNA-Report-09-2021.pdf
[7] CMS, “Update to COVID-19 Emergency Declaration Blanket Waivers for Specific Providers,” QSO-22-15-NH & NLTC & LSC (Apr. 7, 2022), effective in 60 days from Apr. 7, https://www.cms.gov/files/document/qso-22-15-nh-nltc-lsc.pdf
Report: Nursing Home MA Issues Survey
The Center for Medicare Advocacy conducted a short survey of skilled nursing facilities (SNFs) in April 2022 after hearing an increasing number of alarming experiences with Medicare Advantage (MA) from CT beneficiaries and SNFs. The goal of the survey was to determine the nature and scope of issues, if any, SNFs were facing with MA plans. The survey was disseminated by Connecticut Association of Healthcare Facilities/Connecticut Center for Assisted Living and LeadingAge Connecticut. Of the state’s 211 SNFs, 31 facilities responded (27 for-profit and 4 non-profit), amounting to approximately 15% of the state’s SNFs.
1. Overall: Almost two-thirds (65%) of respondents indicated “Yes” their facility had “consistent” issues with a Medicare Advantage plan (e.g., denials of coverage and prior authorization delays).
Of those respondents who replied “Yes”:
- 60% contended that the MA issues impacted the ability of staff to provide quality care to nursing home residents.
- 75% answered that the issues with MA plans have increased in the past twelve months.
2. Issues brought up independently in the survey by the SNFs
Prior Authorization (45% of respondents), issues such as:
- Prospective patients sitting in the hospital
- Delays in authorization
- Denials
- No availability on weekends to provide prior authorizations
- “We are seeing consistent delays in hospital authorizations with Wellcare, Aetna, and UnitedHealthcare. It has taken upwards of 3 or more days to obtain authorization.” (SNF A)
- “Prior authorization delays for admissions from hospitals. Sometimes up to 48-72 hours.” (SNF B)
Denials of Coverage (75% of respondents), issues such as:
- Not complying with the 48-hour requirement for a NOMNC
- Cut from skilled care, even though staff is documenting skilled needs. Potentially leading to unsafe discharge.
- “Constant NOMNC. If a member appeals and wins the appeal, the MA just issues another NOMNC to start the process over again.” (SNF C)
- “Aetna has an in-house policy of retro denials. They authorize and then they will recoup payments … and the facility is held liable.” (SNF D)
- “Patients are having their benefit cut before they are ready to return home, and are left to privately pay for room and board or have an unsafe discharge.” (SNF C)
- “These plans either do not comply with the 48 hours of notice – or – and more importantly issue denials in situations when we know Medicare would have allowed more time.” (SNF E)
Not Following Medicare Coverage Criteria (25% of respondents), issues such as:
- “Staff are educated on Medicare skilled criteria, and Medicare Advantage plans do not follow this. Residents present as needing skilled care and staff is forced to discharge them home, perhaps unsafely, because there is no payor.” (SNF F)
Free Webinar | Medicare Enrollment Matters
Thursday October 13, 2022 | 2;30 PM – 4:00 PM EDT
This webinar will discuss the 2023 Annual Coordinated Election Period (ACEP), including outreach and education materials issued by the Medicare program, common enrollment pitfalls, options when you miss your Initial Enrollment Period, and other considerations for Medicare beneficiaries and those who assist them. Policy changes and other updates for 2023 will also be discussed.
Register now at https://medicareadvocacy.org/webinars/
Discover How We Can Protect & Improve Medicare Together
As a nonprofit organization, the Center for Medicare Advocacy relies on the generosity of our community to sustain a wide range of advocacy and educational initiatives such as providing these CMA Alerts and our popular free webinars. We give voice to people struggling to be heard; their stories guide our mission and our work.
You can help us reach our Summer fundraising goal with a $10 donation today – or any amount you are comfortable giving.
Let’s join together to support the Center’s mission to advance access to comprehensive Medicare coverage, health equity, and quality care for over 64 million current Medicare beneficiaries.
Your support will immediately make an impact today and help build a bridge to a brighter future for generations of Medicare beneficiaries and their families.
Click here to donate today and help us reach our goal!
If you prefer to donate offline, you can mail your check, payable to the Center for Medicare Advocacy, to: Center for Medicare Advocacy, P.O. Box 350, Willimantic, CT 06226.
THANK YOU FOR BEING PART OF OUR COMMUNITY
