The coronavirus pandemic has taken an enormous toll on nursing home residents and staff. Since the beginning of the pandemic and as of the end of February 2021, nursing facilities have reported that at least 640,271 residents and 552,660 staff members have had confirmed cases of COVID-19 and that at least 130,174 residents and 1,623 staff members have died of the virus.[1] These numbers are likely underreported, since the Centers for Medicare & Medicaid Services (CMS) did not require facilities to report COVID-19 cases and deaths until May 2020.[2] Nevertheless, the reported deaths account for more than one-third of coronavirus deaths in the United States and, in nine states, nursing facility residents and staff account for more than half of all deaths,[3] although residents account for less than .05% of the country’s population.[4]
During the pandemic, the federal government waived many longstanding resident protections and facility reporting requirements.[5] Accountability and oversight were severely limited, as CMS waived virtually all standard and complaint surveys[6] and barred long-term care ombudsmen and families from visiting.
What also changed during the pandemic was the large influx of public funds sent to facilities. During the coronavirus pandemic, nursing homes have received billions of additional dollars and non-monetary support from all levels of government in addition to reimbursement for care through the Medicare and Medicaid programs. The Federal Government has given, or in some cases, loaned facilities (with many loans forgiven) hundreds of millions of additional dollars through multiple programs. Most of these federal payments have been made without regard to facilities’ performance. Many states have also increased Medicaid rates across-the-board or paid higher rates for COVID-19-positive residents or established COVID-19-only facilities and paid them high rates. In addition, the Federal and State Governments have provided indirect financial support to nursing facilities, supplying personal protective equipment, tests and testing equipment, multiple training opportunities, the National Guard, and “strike teams” to help facilities in crisis situations during the pandemic. Despite these billions of dollars, the nursing home industry continues to ask for more financial support,[7] even as patients leaving the hospital are choosing home care over facility care for their post-hospital recovery[8] and nursing facilities’ occupancy rates decline to an unsustainable 70%.[9]
Concerns have been raised about nursing facilities that have received extensive COVID financial assistance, although sanctioned for fraud or poor care.
This Report highlights some of the key federal and state programs, both direct financial payments and indirect financial support, and describes some of the concerns raised about nursing home chains and individual facilities that have received extensive financial support.
Federal Money
Billions of federal dollars include at least the following:
Provider Relief Fund. The Coronavirus Aid, Relief, and Economic Security Act (CARES Act), enacted March 27, 2020,[10] created a $175 billion Provider Relief Fund. Approximately $21 billion of the $175 billion was earmarked for nursing facilities.[11] CMS described the distribution of Provider Relief Funds in three phases.[12] Only the third-phase distribution was based on so-called performance. Although the CARES Act requires facilities to spend money awarded under the Provider Relief Fund on “health care related expenses or lost revenues that are attributable to coronavirus,”[13] Seema Verma, then-CMS Administrator, said, as she announced the initial payout of $1.5 billion to skilled nursing facilities (SNFs) in April 2020, that the federal money comes with “‘no strings attached.’”[14]
- Phase One: On May 22, 2020, HHS announced that all certified skilled nursing facilities (SNFs) with six or more certified beds were eligible to receive $50,000 per facility plus $2,500 per bed.[15] More than 13,000 certified SNFs received a total of $4.9 billion. The Washington Post estimated in August that “the average distribution was $315,000, with some larger facilities receiving $3 million or more.”[16]
- Phase Two: On July 22, 2020, CMS announced $5 billion from the Provider Relief Fund “to build nursing home skills and enhance nursing homes’ response to COVID-19, including enhanced infection control.”[17] The money, available for Medicare-certified facilities and state veterans’ homes, could be used for “hiring additional staff, implementing infection control ‘mentorship’ programs with subject matter experts, increasing testing, and providing additional services, such as technology so residents can connect with their families.”[18] The $5 billion was distributed in two phases, $2.5 billion in August 2020[19] and $2 billion in Phase Three.
- Phase Three: On September 3, 2020, CMS announced that it would distribute $2 billion in “performance-based incentive payments” to nursing facilities.[20] To qualify, a facility was required to meet two criteria: (1) a COVID-19 infections rate that is below the rate of infection in the county in which it is located and (2) a COVID-19 death rate that falls below a nationally established performance threshold for mortality among nursing home residents infected with COVID-19. Performance-based payments were made on October 28 ($333 million to more than 10,000 facilities)[21] and on December 7 ($523 million to more than 9,000 facilities).[22]
Paycheck Protection Program. This program, created as part of the CARES Act and extended by the Consolidated Appropriation Act, 2021,[23] provides loans to businesses to keep workers employed during the pandemic.[24] The Small Business Administration (SBA) administers the program. Loans of up to $10 million may be forgiven if “employee and compensation levels are maintained,” “loan proceeds are spent on payroll costs and other eligible expenses;” and “at least 60 percent of the proceeds are spent on payroll costs.”[25] Businesses can receive multiple PPP loans.[26]
SBA data, reported by FederalPay, indicate that, as of March 1, 2021, 10,293 nursing facilities (as reported by December 1, 2020) received PPP loans totaling $5.7 billion.[27] The average PPP loan is $550,701.
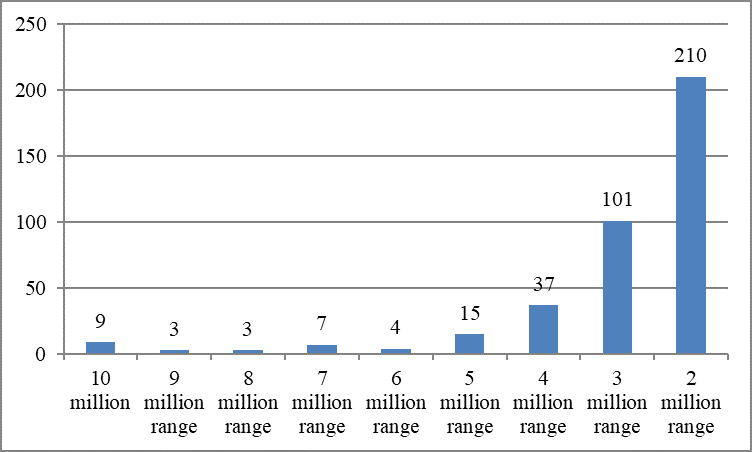
Using SBA data, ProPublica identified nursing facilities and organizations receiving PPP loans.[28] The Center for Medicare Advocacy calculated that 389 nursing facilities and organizations received at least two million dollars in PPP loans, totaling more than $1 billion, as of March 1, 2021.
Nursing Facilities Receiving $2 Million or More from the Paycheck Protection Program
Other Medicare Funding Issues
The reimbursement system that went into effect for Medicare coverage of SNF care on October 1, 2019 – the Patient Driven Payment Model – was intended to be budget-neutral but has in fact “provided $200 more per day than the system it replaced.”[29] The CARES Act suspended the 2 percent sequestration (automatic reduction) in Medicare reimbursement rates for providers for the period May 1, 2020 through December 31, 2020.[30] The Consolidated Appropriations Act, 2021 extended the sequestration relief for three additional months.[31]
Medicare Accelerated and Advance Payment Program[32]
CMS expanded its Medicare accelerated and advance payment program for all Medicare providers in order to expedite payments and provide emergency funding and address cash flow issues.[33]
Other Federal Programs (Not Limited to Nursing Facilities)
Nursing facilities are eligible for other loans, such as Economic Injury Disaster Loans.[34]
Other Programs
LeadingAge New York identified “COVID-19 Financial Assistance Opportunities for Not-for-Profit Providers (Version 10.6.20).”[35]
Medicaid
CMS described flexibilities that enable states to modify their Medicaid payment rates and methodologies, including increasing payments to facilities, targeting payment increases to COVID-19 residents, and amending state plans through the Medicaid Disaster Relief State Plan Amendment template (created in March 2020).[36] The National Governors Association (NGA) reported that 23 states provided additional payments to nursing facilities and 10 states increased staff payments and other employee incentives.[37] LeadingAge described 23 states’ and the District of Columbia’s use of Medicaid to increase reimbursement for facilities during the pandemic.[38]
- Some states increased Medicaid reimbursement across-the-board, by either specific percentages (such as 10%, in California and Oregon) or dollar increases (such as $20 per day, in Kansas, or $40 per day, in Montana).[39] Connecticut increased Medicaid payments by “another $31.2 million” in December 2020.[40] Washington submitted a State Plan Amendment in April 2020 to increase Medicaid rates by an average of $5.17 per day on May 1, 2020 and by $7.40 per day on July 1, 2020.[41]
- Some states focused Medicaid reimbursement on staff salaries. On April 15, 2020, Arkansas announced that CMS had approved its request to use Medicaid to fund the temporary increase of wages for direct care workers, including $125 per week for designated staff (including nursing staff) who worked 20-39 hours per week and $250 per week for designated staff working 40+ hours per week.[42] For staff working with COVID-19-positive residents, weekly wages increased more, $125 for staff working one-19 hours per week, $250 for staff working 20-39 hours per week, and $500 for staff working 40+ hours per week.[43]
- Some states paid higher reimbursement for residents who tested positive for COVID-19. Kentucky announced that it would pay a per diem add-on of $270 for each COVID-19- positive resident.[44] Politico reported that California, Massachusetts, Michigan, and New Mexico paid incentive payments to facilities accepting COVID-19-positive patients from hospitals.[45]
- Some states created coronavirus-only facilities and paid higher rates (“double or more”) for care of their residents.[46] Ohio, for example, pays as much as $984 per day for a resident in isolation centers who needs a ventilator.[47] Some coronavirus-only facilities had poor records for quality of care.[48] New Mexico named as its coronavirus-only facility Canyon Transitional Rehabilitation Center, a one-star facility owned by Genesis HealthCare that was cited for “a complete lack of infection control, massive staff shortages and staff incompetence.”[49] The facility was eligible for payments of $600 per patient per day, in addition to Medicare payments for the residents.[50]
Federal and States Non-Monetary Support
Nursing homes also received large amounts of non-monetary support during the pandemic. This support includes personal protective equipment (PPE), tests and testing equipment,[51] training, assistance from the National Guard, and strike teams.
- PPE: In May 2020, the Federal Emergency Management Agency (FEMA) sent a 14-day supply of PPE to 15,000 nursing homes nationwide. The supplies included more than 7.1 million surgical masks; almost 32.3 million gloves; more than 922,000 goggles/eye protection, and almost 9.7 million gowns.[52] States also provided PPE to facilities. For example, Georgia provided facilities with “industrial foggers, disinfectant solution” as well as “hundreds of thousands of face shields, masks, gloves and gowns.”[53]
- Tests: In July 2020, the federal government announced that it would send point-of-care antigen tests to all nursing facilities that were certified to perform the tests.[54] States also sent tests and testing equipment to facilities. In May, Delaware’s Governor announced a plan for universal testing of all residents and staff in long-term care facilities and said that the state would provide all facilities with “tests, testing supplies, training, and support.”[55]
- Training: The Federal Government has provided a considerable amount of training to nursing facilities, focusing on infection control.
On August 25, 2020, CMS provided “CMS Targeted COVID-19 Training for Frontline Nursing Home Staff and Management” in order “to equip both frontline caregivers and their management with the knowledge they need to stop the spread of coronavirus disease 2019 (COVID-19) in their nursing homes.”[56] A new National Nursing Home COVID Action Network was created under an Agency for Healthcare Research and Quality contract to provide “free training and mentorship to nursing homes across the country to increase the implementation of evidence-based infection prevention and safety practices to protect residents and staff.”[57] - The American Rescue Plan includes $200 million to Quality Improvement Organizations to provide support for infection control and vaccination uptake.[58]
- National Guard: The CMS “Toolkit on State Actions to Mitigate COVID-19 Prevalence in Nursing Homes” (Feb. 2021 edition[59] and earlier monthly editions) described activities of the National Guard in at least 18 states.[60] Tasks performed by the National Guard included disinfecting nursing facilities, conducting COVID-19 testing, staffing facilities, training and assisting in infection control, assisting with data collection, and providing ancillary services.
- Strike Teams: Maryland was the first state to use strike teams. The teams were “made up of National Guard, state and local health departments and hospital systems” and their purpose was to “provide emergency care, supplies and equipment to assist overburdened nursing homes and extended care facilities” that experienced a coronavirus outbreak.[61] The CMS Toolkits describe infection control “strike teams” used by states to test residents and staff for COVID-19, provide nurses and aides to achieve staffing stability, assist staff with implementation of infection control protocols, provide “initial triage, site assessment” and other functions for facilities on request, and go into facilities with outbreaks, among other functions.[62] The National Governors Association reported that 28 states had dedicated support teams for nursing facilities.[63]
CMS also deployed federal Task Force Strike Teams “to provide onsite technical assistance and education to nursing homes experiencing outbreaks.”[64]
The American Rescue Plan includes $250 million for Strike Teams.[65]
COVID-19 Money for Poor Performing Facilities
Concerns have been raised about multi-state nursing home chains that have received federal and state money during the pandemic, despite the poor care they provide and the legal actions brought against them for defrauding the Government. Concerns have also been raised about COVID-19 payments and loans made to individual facilities, despite their poor records for care and their high rates of COVID-19 cases and deaths.
The Washington Post reported in August, “More than a dozen companies that received federal funding have settled civil lawsuits in recent years with the Justice Department, which alleged improper Medicare billing, forged documents, substandard care and other abuses.”[66] A dozen companies, nearly all operating under corporate integrity agreements with the HHS Office of Inspector General, repaid the Government more than $260 million. Nevertheless, companies that have been sued for Medicare fraud in recent years “received more than $300 million in relief payments.”[67]
The Washington Post described large payments to a sample of such chains:
- In April 2020, Saber Healthcare and related entities agreed to pay $10 million to resolve allegations under the False Claims Act that nine of Saber’s facilities in North Carolina, Ohio, Pennsylvania, and Virginia, submitted false and inflated claims to Medicare.[68] The Washington Post reports that Saber Healthcare received more than $45 million in pandemic funding.[69]
- Brius Healthcare Services, California’s largest operator with 81 nursing facilities and a record of “police scrutiny, lawsuits, stiff regulatory fines and state and federal investigations that have uncovered numerous alleged violations,”[70] received more than $35 million in federal relief funds.[71]
- Life Care Centers of America, a privately-held company with more than 200 nursing facilities, is currently under a five-year Corporate Integrity Agreement (signed 2016) with the HHS Inspector General for overbilling Medicare.[72] The company’s nursing facility in Kirkland, Washington was the site of the first COVID-19 outbreak in February 2020. Life Care Centers of America received $19,269,489 from the Provider Relief Fund on October 27, 2020,[73] and, according to The Washington Post in August 2020, $48 million in relief payments.[74]
The Miami Herald reports that 24 Florida facilities under common ownership – more than one-third of which are on the state’s Watch List of troubled facilities – received funding totaling between $48 million and $78 million from CARES Act funds, a combination of “competitive federal coronavirus relief funds” and increased federal reimbursement.[75]
The New York Times reported that Genesis Healthcare, the country’s largest operator of nursing homes, “received more than $300 million in government grants and loans” during the pandemic, as of May 2020.[76] These funds included at least a $180 million CARES Act grants, $27 million in state money, and $158 million in advance Medicare payments from the Federal Government.[77] In a February 10, 2021 letter to Senator Elizabeth Warren, Genesis identified additional COVID funding that the company has received: $416.9 million in state and federal grants as well as $247.8 million in loans or advances subject to recoupment or repayment ($199.1 million in CARES Act Provider Relief Funds, $54.5 million in federal grants for infection control, $28.5 under the Quality Incentive Payment Program, $153.2 million in advance payments under the Medicare Accelerated and Advanced Payment Program, $92.2 million in payroll tax deferrals, $11.1 million in temporary suspension of Medicare sequestration, state relief totaling $123.7 million, and a state loan total totaling $2.3 million).[78]
Business Insider reported that 200 “of the US’s worst-performing nursing homes received millions of dollars from the Paycheck Protection Program.”[79] It cited individual facilities that were fined for poor care, but that nevertheless received PPP payments that dwarfed their fines.
For example, Kingston Healthcare Center, a California nursing facility, has a poor record for care. Following a coronavirus outbreak in April and May, the state sent a strike team to the facility so that it could continue operating. In October 2020, the California Occupational Safety and Health Administration fined the facility $92,500, later reduced to $17,315, for failing to protect workers from coronavirus.[80] Kingston Healthcare Center, one of six California facilities designated a Special Focus Facility,[81] was cited with 17 deficiencies as of November 2020, [82] including one immediate jeopardy.[83] As of November 2020, 71 staff and 112 residents, 19 of whom died, had tested posted for coronavirus. Despite this record, the California nursing facility received $1,628,800 in PPP loans,[84] almost triple the $550,701 average that nursing facilities nationwide received in PPP loans.[85]
Andbe Home, a Kansas nursing facility, was in the news when all 63 of its residents, and 55 of its 70 staff members, tested positive for COVID-19 and at least 10 residents died.[86] In October, CMS cited immediate jeopardy, imposed federal fines of $14,860, and moved to terminate the facility’s participation in the Medicare program. Nevertheless, AARP reported in November that the facility had received more than $300,000 in funding from the Provider Relief Fund.[87]
Conclusion
During the coronavirus pandemic, nursing homes have received billions of dollars in direct and indirect financial support, although, as the discussion of payments to Genesis Healthcare shows, the actual dollar amounts received by individual corporations (and facilities) change and are difficult to track. Nevertheless, the nursing home industry continues to ask for more assistance.[88] The American Health Care Association claims that at least 1,600 nursing homes could close in 2021 without more aid.[89] As AARP asked, “Nursing Homes Are Getting Billions in COVID Aid – Where Is It Going?”[90] That question needs to be answered before the nursing home industry is given more public dollars.
March 22, 2021 – T. Edelman, M. Edelman
[1] CMS, “COVID-19 Nursing Home Data” (Submitted Data as of Week Ending Feb. 28, 2021), https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/
[2] CMS, “Interim Final Rules Updating Requirements for Notification of Confirmed and Suspected COVID-19 Cases Among Residents and Staff in Nursing Homes,” QSO-20-29-NH (May 6, 2020), https://www.cms.gov/files/document/qso-20-29-nh.pdf. The interim final rule was published at 85 Fed. Reg. 27,550, CMS-5531-IFC (May 8, 2020), https://www.govinfo.gov/content/pkg/FR-2020-05-08/pdf/2020-09608.pdf
[3] “More than One-Third of U.S. Coronavirus Deaths Are Linked to Nursing Homes,” The New York Times (updated Feb. 26, 2021), https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html
[4] The Centers for Disease Control and Prevention reports that 1.3 million people lived in nursing facilities in 2015. CDC, National Center for Health Statistics, Nursing Home Care, https://www.cdc.gov/nchs/fastats/nursing-home-care.htm. The U.S. Census Bureau projected that the country’s population on January 1, 2016 would be 322,762,018. U.S. Census Bureau, “Census Bureau Projects U.S. and World Populations on New Year’s Day” (Dec. 30, 2015), https://www.census.gov/newsroom/press-releases/2015/cb15-tps113.html
[5] CMS, “COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers” (as of Feb. 19, 2021), https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf (Skilled nursing facility waivers are at pp. 16-21
[6] CMS, “Prioritization of Survey Activities,” QSO020-20-ALL (updated 9/28/2020), https://www.cms.gov/files/document/qso-20-20-all.pdf
[7] AHCA, “COVID-19 Exacerbates Financial Challenges Of Long Term Care Facilities” (Press Release, Feb. 17, 2021), https://www.ahcancal.org/News-and-Communications/Press-Releases/Pages/COVID-19-Exacerbates-Financial-Challenges-Of-Long-Term-Care-Facilities.aspx
[8] Alex Spanko, “As Nursing Homes Lose Patients to Home Health During COVID, Past Shifts Show Path Forward,” Skilled Nursing News (Feb. 22, 2021), https://skillednursingnews.com/2021/02/as-nursing-homes-lose-patients-to-home-health-during-covid-past-shifts-show-path-forward/?itm_source=parsely-api; Alex Spanko, “LTC Properties Upbeat on Genesis Leases, Predicts Decline in Home Health Diversions from SNFs,” Skilled Nursing News (Feb. 19, 2021), https://skillednursingnews.com/2021/02/ltc-properties-upbeat-on-genesis-leases-predicts-decline-in-home-health-diversions-from-snfs/
[9] CliftonLarsonAllen, CLA Occupancy Insights (Through Reporting Period January 3, 2021), https://www.mcknights.com/wp-content/uploads/sites/5/2021/01/CLA-Occupancy-Insight-1.22.2021-McKnights.pdf (reporting national occupancy rate of 69%).
[10] Public Law 116-136 (Mar. 27, 2020), https://www.congress.gov/116/plaws/publ136/PLAW-116publ136.pdf
[11] Andrew Soergel, “Nursing Homes Are Getting Billions in COVID Aid – Where Is it Going?” AARP (Nov. 24, 2020), https://www.aarp.org/caregiving/health/info-2020/nursing-home-covid-federal-aid-transparency.html
[12] CMS, “CARES Act Provider Relief Fund: General Information,” https://www.hhs.gov/coronavirus/cares-act-provider-relief-fund/general-information/index.html#phase1
[13] CMS, Acceptance of Terms and Conditions, https://www.hhs.gov/sites/default/files/terms-and-conditions-skilled-nursing-facility-relief-fund.pdf
[14] Verma said, “There are no strings attached, so the health care providers that are receiving these dollars can essentially spend that in any way that they see fit.” Alex Spanko, “$1.5B Medicare Cash Influx to Skilled Nursing Facilities Has Strings Attached -–and Some May Not Keep It,” Skilled Nursing News (Apr. 13, 2020), https://skillednursingnews.com/2020/04/1-5b-medicare-cash-influx-to-skilled-nursing-facilities-has-strings-attached-and-some-may-not-keep-it/
[15] HHS, “HHS Announces Nearly $4.9 billion Distribution to Nursing Facilities Impacted by COVID-19” (News Release, May 22, 2020), https://www.hhs.gov/about/news/2020/05/22/hhs-announces-nearly-4.9-billion-distribution-to-nursing-facilities-impacted-by-covid19.html
[16] Debbie Cenziper, Joel Jacobs and Shawn Mulcahy, “Nursing home companies accused of misusing federal money received hundreds of millions of dollars in pandemic relief,” The Washington Post (Aug. 4, 2020), https://www.washingtonpost.com/business/2020/08/04/nursing-home-companies-accused-misusing-federal-money-received-hundreds-millions-dollars-pandemic-relief/
[17] CMS, “Trump Administration Announces New Resources to Protect Nursing Home Residents Against COVID-19” (Press Release, Jul. 22, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
[18] Id.
[19] CMS, “HHS Announces Allocations of CARES Act Provider Relief Fund for Nursing Homes” (Press Release, Aug. 7, 2020), https://www.hhs.gov/about/news/2020/08/07/hhs-announces-allocations-of-cares-act-provider-relief-fund-for-nursing-homes.html
[20] CMS, “Nursing Home Quality Incentive Program Methodology” (Dec. 7, 2020), https://www.hhs.gov/sites/default/files/nursing-home-qip-methodology.pdf
[21] CMS, “Trump Administration Distributes Incentive Payments to Nursing Homes Curbing COVID-19 Deaths and Infections” (Press Release, Oct. 28, 2020), https://www.hhs.gov/about/news/2020/10/28/trump-administration-distributes-incentive-payments-to-nursing-homes-curbing-covid-19-deaths-and-infections.html
[22] CMS, “Trump Administration Announces New Half Billion Incentive Payment Distribution to Nursing Homes” (Press Release, Dec. 7, 2020), https://www.hhs.gov/about/news/2020/12/07/trump-administration-announces-new-half-
billion-incentive-payment-distribution-to-nursing-homes.html#:~:text=In%20August%2C%20HHS%20announced%20plans,safe
%20environments%20for%20their%20residents. HHS identified, by state, how many nursing facilities received incentive payments in October 2020 and total payments to each state. HHS, “Provider Relief Fund; Nursing Home Quality Incentive Payment Allocations, October 2020,” https://www.hhs.gov/sites/default/files/provider-relief-fund-nursing-home-quality-incentive-payment-allocations-october-2020.pdf
[23] Jim Probasco, “Third-Round Paycheck Protection Program (PPP) Funding: What Is It and How to Apply,” Investopedia, https://www.investopedia.com/your-guide-to-the-paycheck-protection-program-ppp-and-how-to-apply-4802195
[24] Small Business Administration, “Paycheck Protection Program,” https://www.sba.gov/funding-programs/loans/coronavirus-relief-options/paycheck-protection-program
[25] Small Business Administration, “PPP Loan Forgiveness,” https://www.sba.gov/funding-programs/loans/coronavirus-relief-options/paycheck-protection-program/ppp-loan-forgiveness
[26] Small Business Administration, “Paycheck Protection Program,” https://www.sba.gov/funding-programs/loans/coronavirus-relief-options/paycheck-protection-program
[27] “SBA Paycheck Protection Program – Nursing Care Facilities (Skilled Nursing Facilities) – Federal Pay,” https://www.federalpay.org/paycheck-protection-program/industries/nursing-care-facilities-skilled-nursing-facilities
[28] ProPublica, “Approved Loans for Nursing Care Facilities (Skilled Nursing Facilities) Organizations,” https://projects.propublica.org/coronavirus/bailouts/industries/nursing-care-facilities-skilled-nursing-facilities
[29] Alex Spanko, “PDPM Provides $200/Day Medicare Boost to Nursing Homes During COVID: ‘It Arrived Just in Time,’” Skilled Nursing News (Dec. 3, 2020), https://skillednursingnews.com/2020/12/pdpm-provides-200-day-medicare-boost-to-nursing-homes-during-covid-it-arrived-just-in-time/
[30] CARES Act, §3709.
[31] Consolidated Appropriations Act, 2021, §102.
[32] https://www.cms.gov/files/document/accelerated-and-advanced-payments-fact-sheet.pdf
[33] HHS, “Trump Administration Provides Financial Relief for Medicare Providers” (Press Release, Mar. 28, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-provide https://www.sba.gov/funding-programs/loans/coronavirus-relief-options/covid-19-economic-injury-disaster-loans-financial-relief-medicare-providers
[34] Small business Administration, “COVID-19 Economic Injury Disaster Loans,” https://www.sba.gov/funding-programs/loans/coronavirus-relief-options/covid-19-economic-injury-disaster-loans
[35] LeadingAge New York, “COVID-19 Financial Assistance Opportunities for Not-for-Profit Providers” (Version 10.6.20), https://www.leadingageny.org/linkservid/C1D9B1BC-D35A-D25E-DC5636F1906ACF13/showMeta/0/
[36] Anne Marie Costello, Acting Center Director, Center for Medicaid and CHIP Services, “Nursing Home Strategies for COVID-19 Only Isolation of COVID-19 Residents” (Aug. 24, 2020), https://www.medicaid.gov/federal-policy-guidance/downloads/cib082420.pdf
[37] National Governors Association, “State Actions Addressing COVID-19 in Long-Term Care Facilities” (Oct. 15, 2020), https://www.nga.org/memos/state-actions-long-term-care-facilities/
[38] LeadingAge, “States Leverage Medicaid to Provide Nursing Homes a Lifeline through COVID-19” (Jun. 12, 2020), https://www.leadingage.org/regulation/states-leverage-medicaid-provide-nursing-homes-lifeline-through-covid-19#
[39] Id.
[40] Jenna Carlesso and Keith M. Phaneuf, “Lamont directs another $31.2 million to CT nursing homes,” The CT Mirror (Dec. 30, 2020), https://ctmirror.org/2020/12/30/lamont-directs-another-31-2-million-to-ct-nursing-homes/
[41] State of Washington Health Care Authority, “Medicaid State Plan Amendment (SPA) 20-0019 Nursing Home Daily Rates” (Apr. 27, 2020), https://www.hca.wa.gov/assets/20-0019-NF-Rates-Public-Notice-WSR-20-10-026.pdf
[42] Arkansas Governor Asa Hutchison, “Governor Hutchinson Announces CMS Approval of Additional Pay For Eligible LTSS Direct Care Workers Due to COVID-19 Emergency” (Press Release) (Apr. 15, 2020), https://governor.arkansas.gov/news-media/press-releases/governor-hutchinson-announces-cms-approval-of-additional-pay-for-eligible-ltss-direct-care-workers-due-to-covid-19-emergency
[43] Id.
[44] LeadingAge, “States Leverage Medicaid to Provide Nursing Homes a Lifeline through COVID-19” (Jun. 12, 2020), https://www.leadingage.org/regulation/states-leverage-medicaid-provide-nursing-homes-lifeline-through-covid-19
[45] Maggie Severns and Rachel Roubein, “States prod nursing homes to take more Covid-19 patients,” Politico (Jun. 4, 2020), https://www.politico.com/news/2020/06/04/states-nursing-homes-coronavirus-302134
[46] Maggie Severns and Rachel Roubein, “States prod nursing homes to take more Covid-19 patients,” Politico (Jun. 4, 2020), https://www.politico.com/news/2020/06/04/states-nursing-homes-coronavirus-302134
[47] LeadingAge, “States Leverage Medicaid to Provide Nursing Homes a Lifeline through COVID-19” (Jun. 12, 2020), https://www.leadingage.org/regulation/states-leverage-medicaid-provide-nursing-homes-lifeline-through-covid-19
[48] Maggie Severns and Rachel Roubein, “States prod nursing homes to take more Covid-19 patients,” Politico (Jun. 4, 2020), https://www.politico.com/news/2020/06/04/states-nursing-homes-coronavirus-302134. See also Toby Edelman and Miriam Edelman, “COVID-Only Nursing Facilities: What Happened To A Good Idea?,” Center for Medicare Advocacy (Oct. 15, 2020), https://medicareadvocacy.org/covid-only-nursing-facilities-what-happened-to-a-good-idea/ (discussing the lack of federal standards and states’ largely accepting volunteers to be COVID-19-only facilities)
[49] Ed Williams and Rachel Mabe, “Designated hot spot,” Las Cruces Sun News (Apr. 26, 2020), https://www.lcsun-news.com/story/news/2020/04/26/searchlight-new-mexico-designated-hot-spot/3028883001/
[50] Id.
[51] National Governors Association, “State Actions Addressing COVID-19 in Long-Term Care Facilities” (Oct. 15, 2020), https://www.nga.org/memos/state-actions-long-term-care-facilities/
[52] FEMA, “Coronavirus Pandemic Response: PPE Packages for Nursing Homes” (May 2, 2020), https://www.fema.gov/news-release/2020/05/02/coronavirus-pandemic-response-ppe-packages-nursing-homes
[53] Carrie Teegardin, “$128 million in federal funds targeted to Georgia nursing homes,” Atlanta Journal Constitution (May 22, 2020), https://www.ajc.com/news/state–regional/128-million-federal-funds-targeted-georgia-nursing-homes/onnpjt4jCO0P838KpPxKbK/
[54] CMS, “Trump Administration Announces New Resources to Protect Nursing Home Residents Against COVID-19” (Press Release, Jul. 22, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19; Alex Spanko, “HHS to Provide 400 Tests as Part of Initial Nursing Home Round, with $25/Test Cost Afterwards,” Skilled Nursing News (Jul. 15, 2020), HHS to Provide 400 Tests as Part of Initial Nursing Home Round, with $25/Test Cost Afterwards – Skilled Nursing News ; Andrew Jacobs, “‘Testing Hell’: Gift of Devices to Nursing Homes Brings New Problems,” The New York Times (Sep. 30, 2020), https://www.nytimes.com/2020/09/29/health/covid-nursing-homes-testing.html
[55] Governor John Carney, “Governor Carney Announces Interim Steps Allowing Small Businesses; Universal Testing in Nursing Homes ” (May 5, 2020), https://news.delaware.gov/2020/05/05/governor-carney-announces-interim-steps-allowing-small-businesses-universal-testing-in-nursing-homes/
[56] CMS, “Trump Administration Launches National Training Program to Strengthen Nursing Home Infection Control Practices” (Press Release, Aug. 25, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-launches-national-training-program-strengthen-nursing-home-infection-control
[57] Agency for Healthcare Research and Quality, “AHRQ ECHO National Nursing Home COVID-19 Action Network,” https://www.ahrq.gov/nursing-home/index.html
[58] Public Law No. 117-2, §9401, amending 42 U.S.C. §1395y(g)
[59] CMS, “Toolkit on State Actions to Mitigate COVID-19 Prevalence in Nursing Homes” (Feb. 2021 edition), https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-nursing-homes.pdf
[60] National Governors Association, “State Actions Addressing COVID-19 in Long-Term Care Facilities” (Oct. 15, 2020), https://www.nga.org/memos/state-actions-long-term-care-facilities/
[61] Gregory S. Schneider, Erin Cox and Ovetta Wiggins, “Maryland forms ‘strike teams’ to combat nursing home coronavirus outbreaks,” The Washington Post (Apr. 7, 2020), https://www.washingtonpost.com/local/virginia-politics/maryland-forms-strike-teams-to-combat-nursing-home-coronavirus-outbreaks-in/2020/04/07/0792b312-78f5-11ea-a130-df573469f094_story.html
[62] CMS, “Toolkit on State Actions to Mitigate COVID-19 Prevalence in Nursing Homes” (Feb. 2021 edition), https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-nursing-homes.pdf
[63] National Governors Association, “State Actions Addressing COVID-19 in Long-Term Care Facilities” (updated Oct. 20, 2020), https://www.nga.org/wp-content/uploads/2020/06/State-Actions-Addressing-COVID-19-in-Long-Term-Care-Facilities.pdf
[64] CMS, “Trump Administration Announces New Resources to Protect Nursing Home Residents Against COVID-19” (Press Release, Jul. 22, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
[65] Public Law No. 117-2, §9402, amending 42 U.S.C. §1395i-3(k)
[66] Debbie Cenziper, Joel Jacobs and Shawn Mulcahy, “Nursing home companies accused of misusing federal money received hundreds of millions of dollars in pandemic relief,” The Washington Post (Aug. 4, 2020), https://www.washingtonpost.com/business/2020/08/04/nursing-home-companies-accused-misusing-federal-money-received-hundreds-millions-dollars-pandemic-relief/
[67] Id.
[68] U.S. Department of Justice, “Nursing Home Chain Saber Healthcare Agrees to Pay $10 Million to Settle False Claims Act Allegations” (News Release, Apr. 14, 2020), https://www.justice.gov/opa/pr/nursing-home-chain-saber-healthcare-agrees-pay-10-million-settle-false-claims-act-allegations.
[69] Debbie Cenziper, Joel Jacobs and Shawn Mulcahy, “Nursing home companies accused of misusing federal money received hundreds of millions of dollars in pandemic relief,” The Washington Post (Aug. 4, 2020), https://www.washingtonpost.com/business/2020/08/04/nursing-home-companies-accused-misusing-federal-money-received-hundreds-millions-dollars-pandemic-relief/
[70] Marjie Lundstrom and Phillip Reese, “California’s largest nursing home owner under fire from government regulators,” Sacramento Bee (Jun. 15, 2015), https://www.sacbee.com/news/investigations/nursing-homes/article24015475.html.
[71] Debbie Cenziper, Joel Jacobs and Shawn Mulcahy, “Nursing home companies accused of misusing federal money received hundreds of millions of dollars in pandemic relief,” The Washington Post (Aug. 4, 2020), https://www.washingtonpost.com/business/2020/08/04/nursing-home-companies-accused-misusing-federal-money-received-hundreds-millions-dollars-pandemic-relief/
[72] Corporate Integrity Agreement (Oct. 2016), https://oig.hhs.gov/fraud/cia/agreements/Forrest_Preston_and_Life_Care_Centers_of_America
_Inc_10212016.pdf. U.S. Department of Justice, “Life Care Centers of America Inc. Agrees to Pay $145 Million to Resolve False Claims Act Allegations Relating to the Provision of Medically Unnecessary Rehabilitation Therapy Services” (News Release, Oct. 24, 2016), https://www.justice.gov/opa/pr/life-care-centers-america-inc-agrees-pay-145-million-resolve-
false-claims-act-allegations.
[73] COVID Stimulus Watch, Life Care Centers of America, https://data.covidstimuluswatch.org/individual-record/life-care-centers-of-america-inc
[74] Debbie Cenziper, Joel Jacobs, and Shawn Mulcahy, “Nursing home companies accused of misusing federal money received hundreds of millions of dollars in pandemic relief,” The Washington Post (August 4, 2020), https://www.washingtonpost.com/business/2020/08/04/nursing-home-companies-accused-misusing-federal-money-received-hundreds-millions-dollars-pandemic-relief/
[75] Ben Wieder, “As Florida nursing home residents died, operators raked in federal handouts,” Miami Herald (Aug. 6, 2020), https://www.miamiherald.com/news/coronavirus/article244516407.html
[76] Matthew Goldstein, “Nursing Home Operator Genesis Details Coronavirus Aid,” The New York Times (May 27, 2020), https://www.nytimes.com/2020/05/27/business/genesis-earnings-nursing-homes-coronavirus.html
[77] Matthew Goldstein, “Nursing Home Operator Genesis Details Coronavirus Aid,” The New York Times (May 27, 2020), https://www.nytimes.com/2020/05/27/business/genesis-earnings-nursing-homes-coronavirus.html
[78] Letter to Senator Elizabeth Warren from Robert K. Kelner (Covington & Burling) (Feb. 10, 2021), https://www.warren.senate.gov/imo/media/doc/Genesis%20Heathcare%20Letter%202021-02-10%20(1).pdf. On January 27, 2021, Senator Warren had written Genesis CEO Robert Fish, https://www.warren.senate.gov/imo/media/doc/2020.01.27%20Letter%20to%20Genesis
%20Healthcare%20CEO%20re%20Bonuses%20for%20Top%20Executives.pdf, after The Washington Post reported that Genesis had paid its former CEO, George Hager, Jr., a retention bonus of $5.2 million, months before he retired. Will Englund, “Departing CEO paid $5.2 million ‘retention’ bonus by nursing home chain that lost 2,800 residents to covid,” The Washington Post (Jan. 20, 2021), https://www.washingtonpost.com/business/2021/01/20/genesis-nursing-homes-ceo-bonus/
[79] Rhea Mahbubani, “More than 200 of the US’s worst-performing nursing homes received millions of dollars from the Paycheck Protection Program,” Business Insider (Aug. 17, 2020), https://www.businessinsider.com/nursing-homes-poor-quality-ratings-millions-ppp-loans-coronavirus-2020-8
[80] Rhea Mahbubani, “More than 200 of the US’s worst-performing nursing homes received millions of dollars from the Paycheck Protection Program,” Business Insider (Aug. 17, 2020), https://www.businessinsider.com/nursing-homes-poor-quality-ratings-millions-ppp-loans-coronavirus-2020-8
[81] Special Focus Facility (“SFF”) Program, https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/SFFList.pdf
[82] Stacey Shepard, “Bakersfield nursing home issued major fine for COVID-19 workplace violations,” Bakersfield.com (November 18, 2020), https://www.bakersfield.com/news/bakersfield-nursing-home-issued-major-fine-for-covid-19-workplace-violations/article_1b1aed54-29db-11eb-a244-5fc4248295d6.html
[83] MatchtoOct30Doc12-10-20
[84] ProPublica , “Coronavirus Bailouts: Kingston Healthcare Center, LLC,” https://projects.propublica.org/coronavirus/bailouts/loans/kingston-healthcare-center-llc-4768417201
[85] “SBA Paycheck Protection Program – Nursing Care Facilities (Skilled Nursing Facilities) – Federal Pay,” https://www.federalpay.org/paycheck-protection-program/industries/nursing-care-facilities-skilled-nursing-facilities
[86] Brittany Shammas, “Kansas nursing home faces severe penalties after deadly coronavirus outbreak,” Washington Post (Oct. 27, 2020), https://www.washingtonpost.com/health/2020/10/27/kansas-nursing-home-covid-deaths/
[87] Andrew Soergel, “Nursing Homes Are getting Billions in COVID Aid – Where Is it Going?” (Nov. 24, 2020), https://www.aarp.org/caregiving/health/info-2020/nursing-home-covid-federal-aid-transparency.html
[88] American Health Care Association, “Long Term Care Faces Worst Financial Crisis In Years; Closures Loom Without Additional Funding” (Press Release, Feb. 11, 2021), https://www.ahcancal.org/News-and-Communications/Press-Releases/Pages/Long-Term-Care-Faces-Worst-Financial-Crisis-In-Years;-Closures-Loom-Without-Additional-Funding.aspx
[89] American Health Care Association, “COVID-19 Exacerbates Financial Challenges Of Long Term Care Facilities” (Press Release, Feb. 17, 2021), https://www.ahcancal.org/News-and-Communications/Press-Releases/Pages/COVID-19-Exacerbates-Financial-Challenges-Of-Long-Term-Care-Facilities.aspx
[90] Andrew Soergel, “Nursing Homes Are getting Billions in COVID Aid – Where Is it Going?” (Nov. 24, 2020), https://www.aarp.org/caregiving/health/info-2020/nursing-home-covid-federal-aid-transparency.html
