Despite the nursing home industry’s ongoing insistence that location/zip code is the primary factor determining whether residents infected with coronavirus,[1] evidence mounts that higher nurse staffing levels are correlated with fewer COVID-19 cases in nursing facilities.[2]
Prompted by Bloomberg Law’s finding that the five nursing facilities within 25 miles of Nashville, Tennessee that were operated by the New Jersey-based CareRite Centers “suffered an infection rate more than three times that of the metro area’s 26 other homes,”[3] the Center for Medicare Advocacy took a closer look at the 31 nursing facilities in the Nashville area – five CareRite facilities and 26 facilities with other ownership.
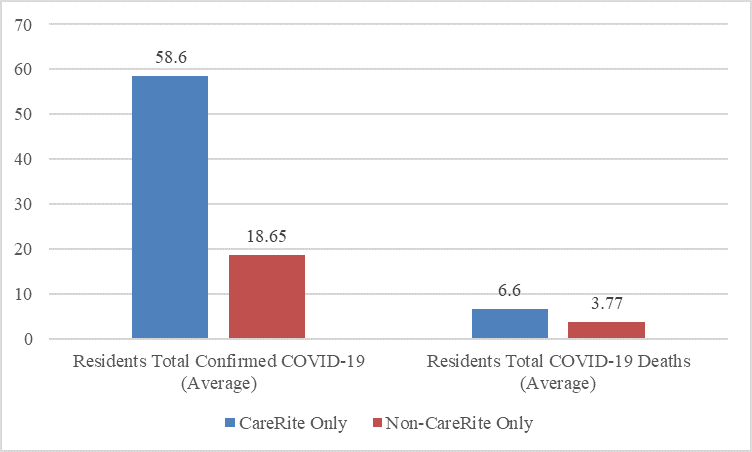
Coronavirus cases and deaths are considerably higher in the five CareRite facilities than the other 26 Nashville-area nursing facilities, according to cumulative information self-reported by facilities and reported through Nursing Home Compare, as of November 15, 2020.
5 CareRite and 26 Non-CareRite Facilities
Nashville, Tennessee Area
Self-Reported Data (Nov. 15, 2020)
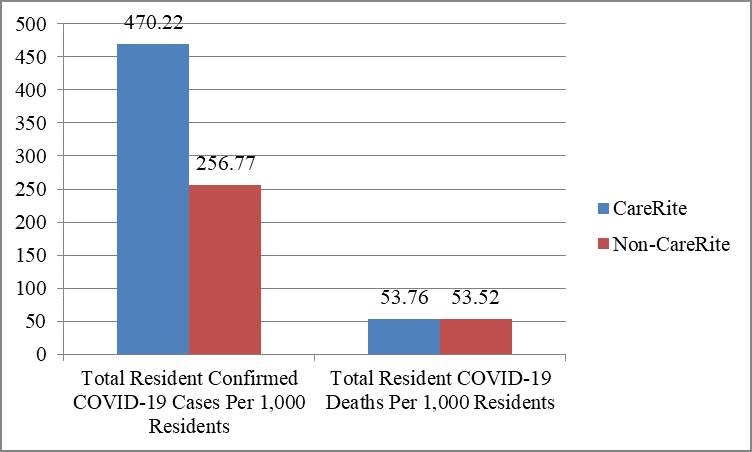
Recognizing that larger facilities may be more likely than smaller facilities to have COVID-19 infections and that CareRite’s facilities are generally larger than other facilities, the Center controls for facility size by showing below total coronavirus cases and deaths per 1000 residents for CareRite and non-CareRite facilities. As of November 15, 2020, CareRite’s Nashville facilities reported almost double the number of COVID-19 cases per 1000 residents, compared to non-CareRite facilities.
5 CareRite and 26 Non-CareRite Facilities
Nashville, Tennessee Area
Covid-19 Cases/1000 Residents
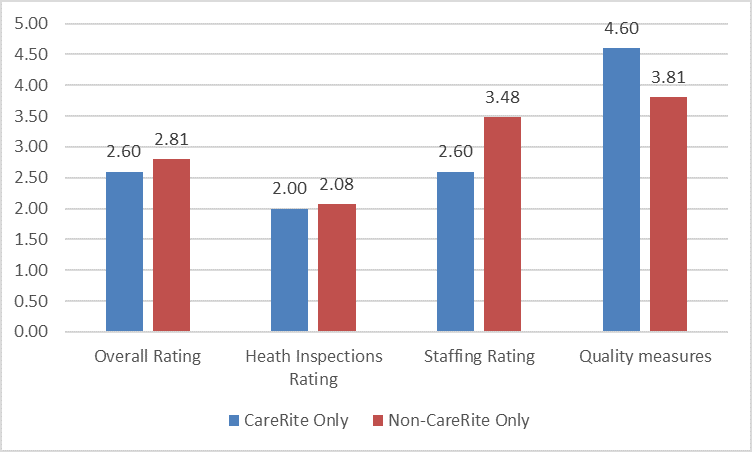
As shown in the below chart, as reported on Nursing Home Compare (data not updated since March 2020),the five CareRite facilities in the Nashville area have lower overall star ratings, lower health inspection ratings, and considerably lower staffing ratings than the 26 non-CareRite facilities. CareRite facilities reported higher ratings only in the quality measure domain than non-CareRite facilities. Quality measures are based largely on self-reported information and are the most inaccurate part of publicly-reported data.
5 CareRite and 26 Non-CareRite Facilities
Nashville, Tennessee Area
Nursing Home Compare
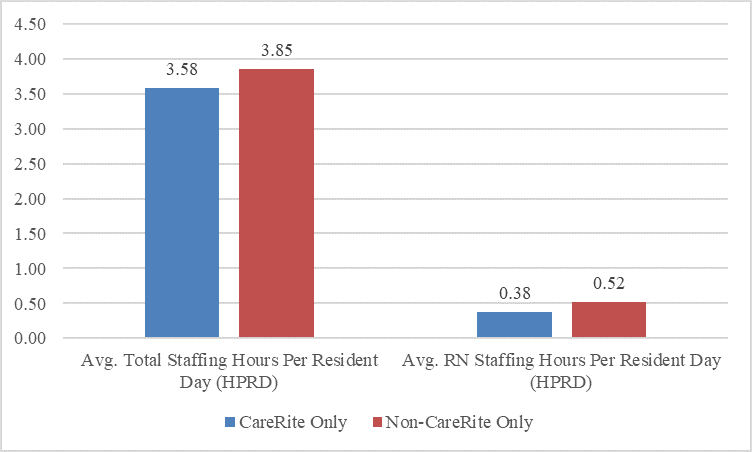
More recent staffing data continue to show that CareRite facilities in Nashville provide residents with much less care by registered nurses, compared to non-CareRite facilities.
In March 2020, as part of the Blanket Waivers for Health Care Providers, the Centers for Medicare & Medicaid Services (CMS) waived the requirement that nursing facilities report staffing data, using the Payroll-Based Journal (PBJ) system.[4] On June 25, 2020, CMS announced that it was ending that waiver, effective with the second calendar quarter 2020 (April –June 2020), although staffing information publicly reported on Nursing Home Compare (now Care Compare) would continue to be held constant and to report data for the fourth calendar quarter 2019 (October-December 2019).[5]
The New York-based Long Term Care Community Coalition published staffing data for the second quarter, 2020, as reported on data.cms.gov.[6] This information, based on PBJ data, shows that CareRite’s Nashville facilities provide less RN care than non-CareRite facilities – 0.38 hours per resident per day, compared to 0.52 hours per resident per day.
5 CareRite and 26 Non-CareRite Facilities
Nashville, Tennessee Area
Long Term Care Community Coalition
PBJ Data, data.cms.gov (2d quarter 2020)
CareRite’s low staffing levels and high rates of COVID-19 infections and deaths are not limited to the company’s Nashville facilities. CareRite’s nine Tennessee nursing facilities have 4% of the state’s nursing home beds, but 10% of the state’s COVID-19 cases and 11% of the deaths. Moreover, two of Tennessee’s three largest COVID-19 outbreaks are in CareRite facilities.
Bloomberg Law reports similar COVID-19 cases and deaths in CareRite facilities in other states. At least 499 resident and staff members have died from COVID in CareRite’s 29 facilities in four states. The company’s 15 facilities in New York, with 3000 beds, have had 336 COVID-related deaths, representing “a fatality rate that’s 75% higher than the average for nursing homes in the state.” CareRite’s four Florida facilities have seen 73 fatalities, “also above the average.”
December 3, 2020 – T. Edelman, M. Edelman
[1] American Health Care Association President and CEO Mark Parkinson, “We Won’t Back Down” (Jun. 2020), https://files.constantcontact.com/64f0b60b701/f86b03a3-a859-4098-b6d0-3866c56672d5.pdf. See Center for Medicare Advocacy, “Nursing Facilities and Covid-19 – it’s not Inevitable” (CMA Alert, Oct, 8, 2020), https://medicareadvocacy.org/nursing-facilities-and-covid-19-its-not-inevitable/.
[2] Center for Medicare Advocacy, “Nursing Facilities and COVID: Staffing Matters” (CMA Alert, Nov. 5, 2020) (discussing Bloomberg Law’s report about Nashville nursing facilities), https://medicareadvocacy.org/nursing-facilities-and-covid-staffing-matters/; Center for Medicare Advocacy, “Studies Find Higher Nurse Staffing Levels in Nursing Facilities Are Correlated With Better Containment Of Covid-19” (CMA Alert, Aug. 13, 2020) (discussing four studies finding facilities with more nurses are more successful in containing COVID-19 cases and death), https://medicareadvocacy.org/studies-find-higher-nurse-staffing-levels-in-nursing-facilities-are-correlated-with-better-containment-of-covid-19/.
[3] Ben Elgin, “Cost-Cutting at America’s Nursing Homes Made Covid-19 Even Worse,” Bloomberg Law (Oct. 31, 2020).
[4] CMS, “COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers” (issued Mar. 2020, updated Dec. 1, 2020), https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf.
[5] CMS, “Changes to Staffing Information and Quality Measures Posted on the Nursing Home Compare Website and Five Star Quality Rating System due to the COVID-19 Public Health Emergency,” QSO-20-34-NH (Jun. 25, 2020), https://www.cms.gov/files/document/qso-20-34-nh.pdf.
[6] https://nursinghome411.org/nursing-home-data-information/staffing/.
