Examining Inappropriate Use of Antipsychotic Drugs, a Report in three Parts, looks at antipsychotic drug use in skilled nursing facilities (SNFs) and nursing facilities (NFs) from two perspectives. First, it analyzes the antipsychotic drug deficiencies that were cited in seven states in calendar years 2010 and 2011 (Part One). Second, in this Part, it reports the perspectives of state Surveyors on the survey process, in general, and the citing of antipsychotic drug deficiencies, in particular (Part Two). Third, it presents recommendations for specific and important ways to improve the citing of antipsychotic drug deficiencies, and consequently, to improve the health, safety, welfare, and rights of nursing home residents throughout the United States (Part Three).
Methodology
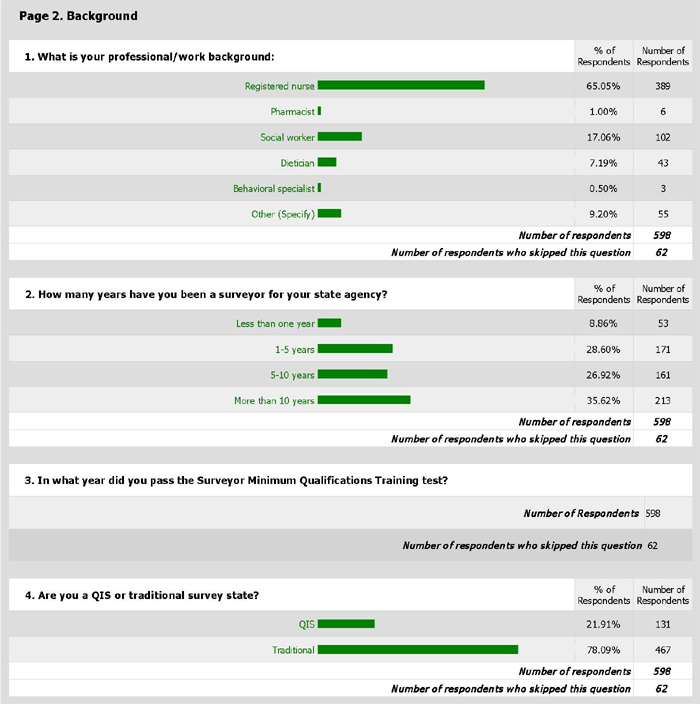
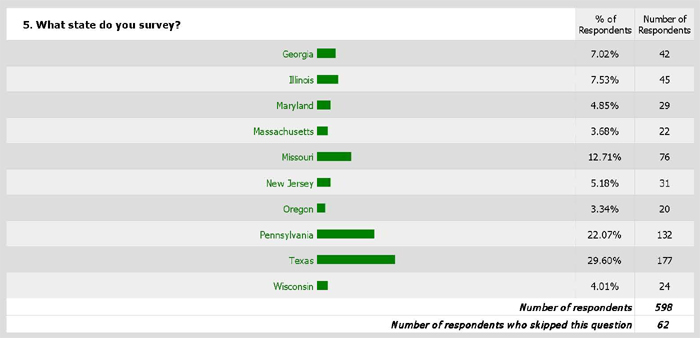
The second Part of the project involved talking with survey directors and their key staff and developing a Questionnaire for Surveyors (with the assistance of the Centers for Medicare & Medicaid Services (CMS’s) Central Office and Regional Offices and State Survey Agency Directors, both individually and at the January 9, 2013 meeting of the Board of Directors of the Association of Health Facility Survey Agencies). When the Questionnaire was completed, State Survey Agency Directors sent e-mails to their Surveyors about the project and including a link to the Questionnaire. Long-term care surveyors in 10 states (the seven states selected by CMS for the project and three states whose survey directors asked for their surveyors to be included) responded to some or all of the Questions. Project staff tabulated and analyzed the responses.
The detailed 49-question Questionnaire asked long-term care Surveyors and their managers and supervisors why they cite antipsychotic drug deficiencies as they do when they conduct surveys. It also sought to learn how facility and surveyor practices have changed, if at all, since CMS launched its Partnership to Improve Dementia Care in 2012. Finally, the Questionnaire asked what changes to facility Requirements of Participation for facilities and the federal survey process would strengthen the citation and enforcement of antipsychotic drug deficiencies and improve the quality of life and quality of care for residents.
More than half of the 49 questions were open-ended. Many included multiple subparts and invited Surveyors to write narrative answers. As a consequence, the Questionnaire resulted in voluminous amounts of numerical and narrative data.
Surveyors were exceptionally generous with their time. More than 400 Surveyors responded to the Questionnaire, writing extensive comments in response to many of the open-ended questions. More than 300 wrote detailed statements about how they believe their work as Surveyors matters for residents.
This Part sets out what the Surveyors told project staff about how and why they cite antipsychotic drug deficiencies, the barriers and challenges they face, what changes they believe would improve the survey process, and what changes they have seen as a result of CMS’s Partnership to Improve Dementia Care. This Part quotes Surveyors’ comments at length in order to give voice to Surveyors and to demonstrate the breadth of their knowledge and experience. Project staff urge CMS and states to consider these comments and the Recommendations in Part Three to improve the effectiveness and efficiency of the oversight system and to improve care for residents.
I. How Surveyors Describe How, Why, and When They Cite Antipsychotic Drug Deficiencies
Surveyors’ responses to the questions are reported below, question by question.
Background
Identifying and Citing Deficiencies Related to Antipsychotic Drugs
Question 6: Without simply referencing the SOM/Guidance, briefly describe the core elements of your analysis in identifying F329 antipsychotic drug deficiencies. We are looking for help in understanding how you primarily evaluate these deficiencies, in practice.
Four hundred one (401) Surveyors responded to Question 6, which was designed to focus Surveyors on the essence (“core elements”) of their F329 citations. The responses were varied, but cumulatively contained the following “core elements” of Surveyor F329 evaluations:
a) Accurate and appropriate diagnosis, and documentation of same;
b) Informed consent by resident, family, personal representative (“Sometimes resident/family never knew of medications”);
c) Start date, and where medication was originally prescribed;
d) PRN analysis;
e) Manufacturer’s recommendations/standards/off-label usage/Black Box Warning;
f) Dosage (least possible);
g) Resident’s drug history;
h) Behavioral assessments (lethargic/participating/sedated/signs of ill effects);
i) Care Plan analysis:
j) Continual monitoring by Physician, Pharma, Staff, etc.;
k) Side effects;
l) Effectiveness (improvement/deterioration);
m) Interviews with Resident, Staff, Family, Pharma, Physician, etc.
n) Whether psychiatrists/psychologists are involved;
o) Review of MDS;
p) Review of MAR;
q) Medication/drug to drug/interaction (Drug regimen review);
r) Observation of resident behaviors;
s) Gradual dose reductions, drug holiday;
t) Facility documented targeted behaviors (falls, incidents, activity logs, hospitalizations, etc.);
u) Drugs administered as ordered;
v) Facility training (studies on dementia/antipsychotic drugs, etc.);
w) Root cause of behavior;
x) Pharma scheduled review;
y) Assessment of ADLs;
z) Inter-Disciplinary Team review;
aa) Physician review/assessment/documentation of same (progress notes);
bb) Analysis of facility utilization rate;
cc) Analysis of “chemical restraint”;
dd) Laboratory analysis;
ee) Physical/other explanations for behavior (UTI, etc.);
ff) Drugging for staff convenience;
gg) Staffing levels;
hh) Promote obtaining highest practicable mental, physical, and psychosocial well-being;
jj) Other, non-pharmacological interventions.
Surveyors describe consistent, detailed, “core element” approaches to citing F329 deficiencies:
When looking at 329 I would look to see if the facility has done a root cause analysis and a systomatic work up for the resident. Did the facility identify the level of risk for the resident did the residents behavior chnage or worsen from baseline, was a medical work up done?. Current med review, and information from the family. Other elements to review would be sufficient staffing, medical causes for a behavior. Interview with perscriber and asking if staff described medical related issues and rational for use of medicaitons. Look at POC and family involvement and what is the facility process for montoring the resident and medications.
Was a behavior assessment completed ? Does the resident have a diagnosis to justify the use of psych meds ? What are the residents symptoms, and are they being monitored on a daily basis by nsg staff, routinely by the physician, and the pharmacy ? Is there documentation that non-pharmacological interventions were attempted prior to initiation of psych meds ? Is resident being monitored for side effects, lab work ? Is there a care plan ? Did the facility get permission from resident/family to treat with meds ? Has there been a GDR attempt ? Is the dosage appropriate ? What non-pharmacololgical interventions are currently being used to treat behaviors ? Has resident been evaluated by psychology/psychiatry ?
Review what is ordered, check for consents, review dose and length of time at that doese. Review pharmacist consultant notes and recommendations, and care plan. Ensure diagnosis for medication is present. Review when last attempt at dose reduction was done and if it was not done, is there documentation to show why it was not attempted. Call doctor and consultant pharmacist if necessary. Also review Psych consultant notes if applicable. Also review behavior monitoring sheets. Interview direct care staff if needed.
Review the medications and the indications for use. Determine if there is a diagnosis for the use of the drug. Determine if they are monitoring side effects and behaviors. Determine if they are doing gradual dose reductions and reviewing the use of the drugs on a regular basis. Determine if the pharmacy consultant has made any recommendations regarding their use. Observe the resident for any signs of adverse drug reactions and/or side effects related to the drugs. Review lab reports to determine if there are any concerns that correlate to the use of the drugs. Review psychiatric and psychotherapy progress notes to determine if they have input into the use of the drugs.
My understanding is we are looking to make sure residents are receiving such medications appropriately and at the lowest doses possible to afford them the highest quality of life. That means we need to make sure there is an appropriate diagnosis for the medication, and the facility staff should be implementing an individualized plan of care (POC), using approaches that are beneficial for the resident. The POC should include non-pharm approaches and should be evaluated routinely to determine the effectiveness of the plan, and to see if interventions need to be adjusted. GDRs should be attempted, if possible, and if not, the faciltiy should be able to substantiate why not. The facility staff should be making a concerted effort to find out the reason behind the use of antipsychotic and should identify specific behaviors exhibited by the residents for which the resident is being treated vs. using generalized terms, such as agitation, etc. Monitoring needs to be on-going and should support either the need to continue the medication or should support the need for a GDR. The facility staff should also provide the family/resident information about the medication to be used, its benefits and potential adverse effects.
It may sound like a simplistic response, but monitoring our facilities for compliance with F329 is a multitiered task. During our tour we are watching the residents and note the presence of any mood disorder or unusal behaviors that may indicate a major mental disorder or serious side effects from receiving antipsychotic drugs. During our visits we look at the facility's roster to identify those residents who are recieving hypnotics, anti-anxiety or psychotropic medications. We review clinical documentation and note the presence and/or absence of any behaviors/symptoms. We look at Psychiatry and/or, psychology consults , pharmacy reviews and recommendations, physican response to pharmacy requests for GDR's, MAR's, AIMS testing, behavior flow monitoring records, care conferences, care plans and any other relevant documentation related to the continued need for antipsychotic medications. We also interview staff, residents and family regarding the residents symptoms, treatment and care.
Initial and ongoing observations of resident done, care plan reviewed, MDS reviewed, Physician Orders reviewed, determine antipsychotic use. If so, what signs and symptoms or behaviors did resident manifest prior to determining diagnosis, was informed consent done, when was drug started and at what dose? Have there been any non-pharmacological interventions attempted prior to use of medication? Has resident been evaluated by psych and risk versus benfit been determined? Is facility monitoring for side effects? and by what method? Are there any adverse reactions documented? From observation-is resident displaying any adverse reactions presently? Is effectiveness of medication being monitored and evaluated. What are other psych diagnoses? Are there multiple psych meds being given for same diagnosis? Is the correct drug being given for the correct diagnosis? Any attempts to taper the drug being done. Drug Regimen review being done by pharmacist? Resident being followed routinely by psych MD. Does the medication nurse have knowledge of the medications and indications for use. Does he/she understand what adverse reactions med can cause? Interview with resident, staff, MD, pharmacist as needed.
At the same time, some Surveyors describe only cursory “core element” identification. These responses may simply be a function of the amount of time taken to complete this Questionnaire, or they may be a function of the particular Surveyor’s thoroughness of review or understanding of F329 analysis. One Surveyor’s insight might also be instructive in this regard:
Because this tag is so verbose, it is difficult to condense into just a summary, but essentially all residents shall be free of unnecessary drugs. This includes duplicate therapy, appropriate indications for use and antipsychotics to manage behaviors. It includes appropriate monitoring addressing gradual dose reductions through the physician and pharmacist.
There may also be a difference in the way in which a Surveyor’s professional or work background affects his/her analysis:
As a Social Worker I observe the residents condition for lethargic or confused behaviors. I review MAR for medications administered and its effectiveness (lethargic sleeping all the time). I also interview the CNA that works with that resident and ask about the behaviors and interactions of the residents to other residents and to staff.
One common theme throughout the Questionnaire, not just in response to this question, is the issue of deference to the physician:
check for a psych diagnosis. check for psych meds. check for right med for diagnosis, right dose, right route-po vs injection, check for duration of order. check for GDR attempt or discussion. check for pharmacy recommendations. check for psych consults- what was their eval and plan. Was it folowed. check for behavior monitoring, interventions prior to prn meds. check for behavior moniotring for antipsychotic meds, if no behaviors, look for GDR. MD usually does not GDR, but becasue he is the MD we do not cite.
Question 7: When investigating F329 deficiencies, do you determine whether a systematic, individualized approach was implemented for a resident with dementia who is in the sample? How?
Four hundred one (401) Surveyors responded to Question 7, which was designed to focus Surveyors on their evaluation of a facility’s systemic, individualized approach to caring for residents with dementia.
Fewer than a dozen Surveyors responding to this question indicate that they “do not” determine whether such an individualized approach was implemented or that the question is “not applicable.”
We are unsure what to make of these very few aberrant responses, especially given that fact that the vast majority of Surveyors link this question with Question 6 and affirm their assertions that a “core element” of their analysis involves examining whether a systemic, individualized approach was implemented.
When describing “how” they “determine whether a systematic, individualized approach was implemented for a resident with dementia,” Surveyors uniformly refer to several “core elements” cited in answer to Question 6 and also uniformly cite many common methodologies for making their determinations:
a) care plan analysis;
b) resident assessments;
c) review of resident life history, social history, and patterns;
d) observations of the resident in different situations in the environment;
e) observations of resident/staff interactions (staff training/interactions with residents with dementia);
f) resident/family/responsible party interviews, including involvement in care planning;
g) activities;
h) staff interviews;
i) consulting pharmacist; physician knowledge/involvement;
j) MDS;
k) Clinical record;
l) Medication review;
m) Interdisciplinary Team individualized approaches;
o) Is medication for resident, or facility convenience;
p) Is medication used as a “restraint.”
Many Surveyors’ responses are illustrative of these methodologies, with sometimes unique approaches:
By review of the care plan, review of the MAR and medication utilizatoin. I review the clinical record for the justificaiton of the administration of medications. Along with this, observation of the resident is important to identify behavior patterns which may either negate or justify the use of medications. I look at pharmacy reviews and for any psych. evals. I will also ask how the QA system works in the facility to potentially identify residents who may be over medicated.
Generally, I will look at my assigned residents to see if they are receiving antipsychotic medications and how the facility is monitoring the use of the medications, including the behavior being monitored and the frequency of the behaviors. I check the care plan, the resident medical record, and interview the staff to determine how well the resident's POC is working, if there were adjustments to the medications and why. Definitely look at the nurse's notes to see if there is supporting data. Once I've determined there may be an issue in this area, I take my findings back to the survey team to see if they, too, were finding similar issues. If so, then we expand our monitoring in Phase II in an effort to determine if there is a system failure vs. one resident having lack of oversight. Obviously, would interview the resident, if possible, family, staff, facility management and the resident's physician, as needed.
I do determine if there is an individualized approach by reviewing what meds the resident is on and their correlating diagnoses. If the resident has dementia, I review the assessments, care planning, behaivor logs to ensure they are individualizing the resident's care, including how activites are implemented related to their behaviors. I review why the resident is on the medication, review what the facility had attempted prior to adding the use of medicaiton as an intervention and reivew the pertinent pharmacy reviews, physician responses/ progress notes, history and physicals, facility progress notes and documentation regarding GDRs. I also observe the resident to ensure the facilty is following the individualized care plan.
I look for the documentation to merit placing the resident on psychotropic medications. Many are diagnosed prior to LTC facility admission and are admitted with these medications and this is where interviewing and record review helps me to make a decision if a resident with dementia should be continued on these medications. If a dementia resident is placed on Psy. meds for the first time I look for behaviors, consults, labs, recommendations and follow-ups by both the primary on consulting staff.
Look at what the facility staff identified as causes for behaviors, how staff described the behaviors (not in general terms like aggitation), what interventions were put in place, if staff communicated between shifts and with family and staff what they were observing and what interventions worked. If the staff conducted a reanalysis of the behavior to determine if interventions needed to be changed or altered in some way.
Yes, by looking at the social background to ensure the other elements of the resident's care (e.g. activities, meals, normal routine, other likes and dislikes) are care planned and being implemented by the staff. If these things are truly addressed and implemented for each individual resident, the "behaviors" and "agitation" would decrease for a better system of meeting the needs on an individual basis. Also, interviewing the IDT to determine how they formulate careplans that are based on different, individual resident needs and how the facility ensures the interventions are carried out and monitored.
Yes, by reviewing the physician's orders. What caused them to be ordered? Was there a new behavior? What interventions were done besides the addition of a medication? Were they effective? Was the family/legal rep notified and consent obtained? What was the monitoring after the medication was started? Has it improved the behavior? Has a reduction been attempted/recommended? What was the response? What does the care plan show? Is there a plan for reduction? Has the resident experienced a decline since the medication was initiated? Who monitors the effectiveness of the medications?
Yes. First by identifying if a resident was admitted on an antipsychotic medication or if one was started after admission. Then by reviewing documentation of behaviors and identifying thru staff interviews if any behaviors exhibited are distressing to the resident or other residents or if the behaviors interfere with the resident's daily routine. Then looking for trials at dosage reductions. If none have been attempted and there are no behaviors justifying the ongoing use at that dosage, a deficiency is generally written.
Surveyors also discuss “facility convenience” to explain their determinations whether a systemic, individualized approach is implemented:
After observation and review of the medicaitons. I check the care plan to see if the facility has looked at the resident as an individual. Do they know the habits and likes of the resident before they had dementia and how the dementia has affected their life.and those of their loved ones. I also look to see if the medicaiton is for the resident or for the facility. Sometimes residents are given medicaiton so they sleep most of the time instead of working with the individual needs of the resident to keep them content with worthwhile activities.
Yes. Do they have an individualized Care Plan? Does the clinical record show justification for use of antipsychotics or is the use a method of controling the resident to make the facility's work easier. And, what other methods has the facility attempted to control the resident's behaviors?
Yes…why are they giving the drug…dementia in itself is not a reason…is it chemical restraint….staff convience…staffing…look at monitoring documentation for the type of behavior it is given for… review the care plan to see alternatives and observe the resident to see if they are following the care plan..hospital records….discharge notes…interview staff, family for how they handeled prior to medication
Surveyors frequently cite care planning as a central feature in their determinations of whether a “systemic individualized approach” has been implemented. However, Surveyors also question whether the resident’s individual care plan had actually been appropriately developed, whether appropriate changes and updates are made, and whether staff are actually familiar with the care plan and how it should be implemented:
look at behavior analysis, how is it quantatified. is careplanning developed to address the behavior and is care plan consistently implemented? is careplan revised if ineffective in reducing target behaviors.
Often hard to determine. Most places do not have an individualized approach and care plans are scant. Mostly by observation and interview of staff
Review for an assessment of the resident, behaviors, preferences for care and activity and if resident and/or family was involved in obtaining information. Was the assessment used to develop and individualized care plan. How do staff know the information on the care plan, and how do they implement it? Determine how staff monitor if the interventions on the care plan are being implemented and if they're effective. Review how the interventions are periodically reviewed and revised as necessary.
Facility policies and procedures are rarely mentioned in Surveyors’ determinations of “systemic individualized approach” implementation. Two examples of the context in which policies and procedures were mentioned are instructive:
Review the assessments for the resident and assessments should be reflection of the resident. Likewise an individualized care should be driven by the assessment of the resident The facility should have polices and procedures outlining how a resident is systematically assessed, evaluated, and reassessed
Yes, through record review, observations and interviews with resident and staff. Was medications identified on MDS and care planned accordingly. Review facility policy and procedures for reducing antipsychotic use, review drug regimine reviews and actions taken. Look at reason on medication attempts to reduce medications, physician involvement, as well as pharmacist. Review behavior log or nurses notes to see if medication use is improving maintaining stable mood/ behavior for resident consistent with resident needs.
As reflected in many of the Surveyors’ responses to multiple Questionnaire questions, Surveyors’ concerns about the QIS process are apparent:
Very difficult in practice. Look for information in the medical record for this, but it is difficult to confirm during the qis process. The window is short and many tasks need to be completed.
One Surveyor’s notation regarding the true nature of the resident’s actual behaviors “needing to be addressed,” often hinted at by many Surveyors, states:
Yes, by reviewing the above topics for each resident.
Clarifying interviews with staff individuals often describe no offensive behaviors besides noise or extra bathroom trips.
CNA staff are very helpful when determining if their are detrimental behaviors presented by residents.
There was no mention of Surveyors examining staffing or staff training as a way to determine whether a “systematic individualized approach” was implemented by a facility.
Electronic medical records are sometimes noted as problematic, not just in response to this Question 7, but many others as well:
Yes, Antipsychotic medications are accompanied by behavior sheets. Review of this documentation indicated if behaviors are appropriate (i.e., anxiety vs. constant neverous movements of head and feet) and are consistantly documented with alternate attempts at redirection of behavior before medication is administered.
Review of the MDS and/or nurses notes to determine if the ADL decline occurs when the antipsychotic is initiated and if alternative interventions have been attempted. This is getting to be most difficult a task as the facilities become more computerized. It is hard to traverse the system and find parallel time lines for comparison.
Family involvement is rarely mentioned by Surveyors as a way to determine implementation of a “systemic individualized approach:”
Yes. Review the records of resident's that are on psychotropic medications. What chain of events occurred in each resident's situation? Did the facility consistently follow the protocol with regard to psychotropic? Is the facility doing all they can to manage the resident's dementia? What does the residnet's family have to say?
Not infrequently, Surveyors note that they examine whether some, many, or nearly all residents are treated identically, in order to determine whether a “systemic individualized approach” was implemented:
Done the same for each resident regardless of dementia or not. Look at facility's overall system for residents (IDT, Care Plans, Family Involvement) and drill down to how it was managed for that specific resident by following updates, etc as time has progressed. Focus on changes of condition for that resident and the reaction of the provider. If a non-individualized pattern is seen (same solution for all residents) dig deeper.
I try to make sure the residents medication is individualized for their needs. I would not expect to see the same medications/prescribed amount of medication etc. for all residents with the same diagnosis. I would look to see that the medications prescribed have a coordinating diagnosis and have been prescribed to meet some type of behavior that has been seen on the unit, or noted in the chart. . I would try to look at (if possible) more than one resident's medication who has dementia, and discuss any red flags with the team, to see if they have any similar concerns.
there is a sample drwn. then every one on the NF list that recieves psy meds is reviewed to make sure the facility medical practicioner is not just administering without just cause. Also an evaluation is made to see if different medications are given to make sure the medications are simpley dispensed by rote. individuals with certain diagnosis are not eligible for therapies as the would be ineffective but many are and counseling could possibly be more effective than medications that may have a long twem affect on the individual.
what is the history and assessments for the individual-is this repeated or very similar to other resident's treatment by the physician
Yes, I look for a system that covers all the important assessment questions, however, I do not expect every resident to receive the same interventions so after the initial recognization of a problem, staff must find the triggers and try multiple interventions.
Yes. Individualized approach is very important. Making sure they understand each resident and develop individualized intervention is very important. The problem has been the facilities’ have been using a blanket approach – one intervention fits all – compromises the care of the residents. They fail to understand the unique characteristics/behavior of each resident and fail to develop individualized care plan.
Sample selection is sometimes noted as essential:
Yes, We certainly try to do this thru a sample selection that focuses on more than one resident with dementia being selected.
Question 8: When investigating F329 deficiencies, do you determine whether the nursing facility has in place, and follows in practice, a systemic process for providing care to persons with dementia? How?
Question 8, answered by 401 Surveyors, relates to the ways in which a facility goes about providing care to residents with dementia. Question 8 was intended to explore whether facilities have in place, and the ways in which Surveyors evaluate, a systemic process for providing dementia care.
Fewer than 20 Surveyors indicate that they do not determine whether the nursing home they are surveying maintains a systemic process for providing care to persons with dementia. One Surveyor indicates they could not do so because of survey time restrictions:
No, we do not feel time allows for this. We just look at our sampled residents. We do not have time to do this along with all the other expectations of CMS.
Another Surveyor notes they do not do so because of the lack of regulations supporting this activity:
No. There are no regulations for this.
Two additional Surveyors who indicate they made no such determination state:
Not really when doing F329 revieiw. The care for the resdient is holistic and if dementia is a diagnoses the care plan should be individulized and identify what works and what doesn't regardless if they are on antipsychotics or not.
Not sure I understand….an overall systematic process for all persons with dementia? I guess I'd have to say no, but I'm not sure what you mean.
It remains unclear whether this limited number of Surveyors understood the nature of this Question. However, it is clear that the vast majority of Surveyors determine whether the facilities they survey have in place, and follow in practice, a systemic process for providing care to persons with dementia. It is also clear that Surveyors utilize common methodologies for their determinations, including, but not limited to:
a) Policies and procedures review;
b) Evaluation of staff knowledge;
c) Evaluation of staff training;
d) Evaluation of staff interaction with residents/interventions;
e) Evaluation of activities offered;
f) Care plan analysis;
g) Adequate staffing, Consistent staffing;
h) Communicating;
i) QA inquiry;
j) Root cause analysis;
k) Committee monitoring antipsychotic medications.
In answering Question 8, the majority of Surveyors incorporate, in one way or another, many of the same methodologies they note in answers to Questions 6 and 7. For example, care plan analysis was nearly uniformly noted as a way to determine whether a facility has a systemic process for providing care to residents with dementia. Very often, Surveyors would simply reference Questions 6 and 7 directly, or make reference to their answers “as above.”
A majority of Surveyors highlight a review of facility policies and procedures as their method (in part) for determining whether a facility uses a systemic process for providing dementia care. Many Surveyors also highlight their focus on activities offered to residents as a part of their determinations.
Care plans and assessment are uniformly mentioned by Surveyors:
Again, I don't believe facilities follow a systematic routine but have practices that dovetail information together and are implemented on a more individualized need analysis (via assessments such as MDS/CAAS, Nursing assessments, Social Service assessments, Nutritional assessments, Activity assessments, etc., leading to care plan creations that may or may not include medication (F329) concerns.
Analyze care planning for residents triggered for behaviors or use of antipsychotics, observe these residents and interaction with nursing staff. Not presence of restraints, oversedated residents, etc. Review records for the history of behaviors and use of medications and non-medication interventions. Interview staff with dementia management techniques.
Assessment, Care planning, observing the resident, making notes when behaviors occur, that the team has discussed what has been done, what didn't work and try alternative optioins before medications are started. Then we consider how the resident has been affected by the facility's actions or lack of action.
I do check the care plan. It is usuall a cookie cutter deementia care plan, no real individual plan to redirect, try this or try that -try this activity. But we are told we do not cite deficiencies based on care plans.
Review for an assessment of the resident, behaviors, preferences for care and activity and if resident and/or family was involved in obtaining information. Was the assessment used to develop and individualized care plan. How do staff know the information on the care plan, and how do they implement it? Determine how staff monitor if the interventions on the care plan are being implemented and if they're effective. Review how the interventions are periodically reviewed and revised as necessary.
Review the care plan and interview for interventions other than medications provided to deal with dementia
[R]eviewing assessments and care plans for clues about individualized approaches, observations of approaches, if able, and interviews to determine if staff are aware of resident conditions and care planned interventions.
We look at the individual needs of the residents and how the facility handles those needs. Do they try to do the same thing will all residents with dementia or do they actually do proper assessments and find what is best for the resident and care plan accordingly.
Yes. I review the plans of care, interview staff to determine their knowledge of dementia care as they relate to specific residents.
Specialized Units:
As above. Mostly by observation of the interaction by staff. On dementia units it is a little easier because the activities usually are better at engaging the residents. In standard units it is more a hit and miss.
I find the best systemic approach to dementia being provided on our State of Illinois certified Alzheimers Subpart B units. Thislicensure status requires a systemic approach by all departments and requires all staff on the unit whether part or full time to be trained initially and on an ongoing basis in dementia care.
I would start with observations of residents with dementia, if they have a special unit dedicated how does that unit work? Are things running smoothly (i.e. staff are able to care for residents, residents are not agitated on a consistent basis, staff is attempting to meet the resident’s needs). If I had concerns regarding the practices/systematic process I would interview staff and family, regarding the day – to – day functioning of the unit/individual care of the residents. I would also review the regulation and read the facility policy, to see if what the facility has set up to be the practice/process is clear if the staff are trained, an is that what’s being implemented on the units.
We look though the literature the home provides the families and their Alzheimer's disclosure. We also ask a sample of staff general abuse/neglect questions which includes the education they have received (including residents with Alzheimer's disease). Also, we attempt to pick residents on an Alzheimer's unit (if applicable) and monitor staff/resident interactions. If they do not have a unit, the teams still samples a stratified sample which may include residents with Alzheimer's disease.
Yes we check this on all residents who have issues with their disease and how the facility addresses any kinds of behaviors or memory impairment that the resident may experience. Specific questions are also asked during the entrance conference regarding dementia residents and how staff are trained and if there are special units for dementia residents in the facility.
Comparing residents:
By looking at the plans of other residents for comparison to see it is individualized. by observing the resident in the facility setting and how the staff interacts with the resident and how well do they know the resident as an individual.
Policies and Procedures:
I really have not focus on the facility's practice as much as on the individual sample resident. I do ask for policies and procedures and see if they are following their own policies and if they have educated their staff on dementia and its managment and this is the extent of my facility process.
Review behavior monitoring, review assessments. Review policy and ask staff what they do when resident exhibits new/worsening behavior.
Review facility policies and procedures, staff training and education, observation of resident care, review of assessment and care plan, and staff interviews.
Yes. After I have made a determination of deficient practice, I interview the facility's staff, including the administartive staff, then I review ther policy and procedure. I use the policy to confirm my findings not to determine deficient practice.
Quality Assurance (QA):
By review of the census and condition sheets, numbers of residents are identified with psych med utilization. QA meeting with administration is also an avenue to determine the effectiveness of the QA process. Policies and procedures are reviewed. Pharmacy policies are reviewed and many times consultant pharmacist interviewed to determine what their process is to justify medications and how they interact with the facility and primary physician on findings. Observation is also importannt as to how staff care for and deal with residents with dementia. Consistency is evalutated as how care delivery is provided.
What programs do they have in place? How is the medical director, physician, don, adminstration, pharmacist all in involved in the program related to dementia care? What are they doing in QA related to dementia care?
Sufficient staff:
Chech policies. And ed. Interview staff for their knowedge. And observe with rts. Do tjey know and follow plan. Are they involved with an. Do they think plan is effective. Do they have enough staff to follow plannot
Review of pyschoactive medication policy. Look at how many residents have dementia/behvaviors. Review of activity calendars, resident attendance, and care plans. Communicate with other team members to compare observations and that the facility is identifying residents with dementia and the increased care that may be needed. Would be helpful if guidance referred to actual time which may be expected to properly care for residents with dementia. With the minimum requirement of 2.7 hours per resident for direct care, at times difficult to cite deficient practice to expect facility staff to do as much as they should to treat residents with dementia (in an ideal situation).
yes we would look to see if the facility has done a root cause analysis and a systomatic work up for the resident. Did the facility identify the level of risk for the resident did the residents behavior chnage or worsen from baseline, was a medical work up done?. Current med review, and information from the family. Other elements to review would be sufficient staffing, medical causes for a behavior. Interview with perscriber and asking if staff described medical related issues and rational for use of medicaitons. Look at POC and family involvement and what is the facility process for montoring the resident and medications.
Yes. Observe environment, equipment/supplies, review staff training and interaction between staff and residents, appropriate amount of staff to deliver care needed, interview staff and residents, review record, care plan for care needed and identified.
Consistent staffing:
Depends on how a resident with dementia is presenting. If the resident has no behaviors how are they ensuring the resident remains busy. How are they providing the ADLs. How to they handle late stage dementia. Do they have consist care givers? Are the staff trained? With a well run dementia unit, antipsychotic use should be minimal
Look to see if they have a routine for the residents care. ie consistant care givers, routine. look to see if they reappraoch the resident if behaviors exist that will not allow care to be provided at any given time.
Review ADL's, care plans, make observations of how staff interact with residents, look at activities that are in place for residents with dementia.
Is the staff providing care consistent or are staff members moved frequently?
Yes. Determine if the staff have any training on residents with dementia, if they provide consistent staffing so that the staff know the residents. Also look at nurse's notes and NA documentation.
Staff training/knowledge/interaction:
Look at staff training, if they have ongoing training for working with residents with dementia. Also look at activities to see that there are activity programs available for varying levels of cognition. Look to see how residents with Dementia spend "down time", if they have residents in area where sensory stimulating, or if left alone in room without stimulation, facing wall. Also look at staff interaction with residents, how talk to residents with dementia.
Look at the development of a program with training for staff to help them understand the disease and the need for individualized approaches to each resident. Use observation to determine if the education was used in practice. Look at the record and interview staff to determine if patterns were identified, interventions developed and care plans implemented
Observation, interview. Look to see if the facility encourages and utilizes all of its staff to assist with caring for the residents. Such as staff from administration answering call bells, or staff from maintenance talking to a resident who is lonely. Look at types of in services being done other than those required. Does the facility have a staff educator? How involved is the activity dept with the dementia residents? What is the caliber of the activity for the dementia resident? Is there a purpose to it or is it just to mark time.
Review of nurses notes, behavior monitoring sheets and care plans. Also, observation of the staff/resident interactions. Determining what interventions have been identified by the staff that may deter from drug use and if they are used or effective.
Yes- training on caring for persons with dementia and how to address behaviors before administering medications.
Yes Review facility policy but only after observations of residents with dementia andsubsequent concerns about their care/interactions with staff.
Yes, I observed the resident, the caregivers interation with the resident and other resident interaction with the resdient. I observe the activity level of the resident and whether actively involved in the activity program. I interview the resident or the family member, interview the staff persons. i review the health record for care plans and determine whether the care plan was observed in action. I check the physician's order to determine if transcribed and given as ordered. I check the lab orders to determine if monitoring was done as ordered.
yes. I check for initial training to ensure that the staff working with the dementia resident has been adequately trained initially then on goingly to ensure the safety of the resident and the staff memeber. I interview staff and observe the interaction with the residents and staff members.
Communication:
First review the staff members interventions for the targeted behavior, observations to ensure the staff are following interventions, and interviews to show what staff do when an intervention does not work, communication between staff and family and physician, and changes made as a result of communication…
Is the environment optimal for residents with dementia? Does the facility flag for antipsychotics? Is the pharmacist communicating with the physician and does the physician respond.
Critique of the Quality Indicator Survey (QIS):
From record one can tell pretty quickly if the pharm reviews are superficial; fastest way to review system is to interview key staff and ask open ended question to explain process then review the medical record to see if the described process is in use; QIS doesn't allow for much in the way of following a direct path while leaving open the opportunity to change direction based on critical thinking skills and facts that come into evidence during the survey as it unfolds
Caregiving for all residents/holistic approach/systemic process:
I do not feel that a resident with dementia requires additional processes if a facility individualizes its care for all residents.
Every resident is assessed for activity preferences (although the demented resident may require family input), food choices, target behaviors that manifest from psychiatric history, roommate compatibility, ADL level, safety precautions, etc.
If you mean a behavior plan if the resident has behaviors then yes.
If a dementia resident does not have behaviors then in many respects the process is the same as for all other residents as far as engagment in appropriate activities, dining, care provision etc…should really be the same e.g. individualized to the resident specific needs
Most facilities use a systemic process in providing care toresidents with dementia instead of an individualized process. Generally psych recommends the use of the same drugs and will increase , decrease or discontinue or add a drug, the facility conduct the drug review with pharmacy and medical director monthly or quarterly and will discontinue drugs for non use or contraindications
Yes- include enough individuals with dementia diagnosis to enable determination. Are they assessing for individual interventions? Have they care plannned accordingly addressing all facets – activities, behavioral interventions, dietary, etc? In other words, a holistic approach.
Yes. Need to look at overall picture based on the residents' needs. Care for dementia residents is a specialty. Does the facility have a process in place looking at each person individually? If there are behavioral issues, prior to antipsychotic usage, does the facility assess if there are any medical or environmental concerns causing the behavior. Are nonpharmacological approaches attempted prior to antipsychotic use. What activities are provided and are they appropriate?
An array of elements/staff convenience:
Observations, interviews with resident, family and staff. Clinical record review. What kind of staff training is being done and is it ongoing? Policy and procedure review as needed. Observe staff interaction with residents with dementia. Are physician orders being reconciled monthly? Are physician orders being reviewed by pharmacist routinely? Is pharmacist doing a MRR and identifying and documenting irregularities? Are psych meds being given as ordered. Are prn antipsychotics being given inappropriately to control behaviors for the benefit of staff or are non-pharmalogical interventions attempted first? Are prns used consecutively greater than 10 days. What communication was provided to physician? family? Are s/e's being monitored? Is effectiveness of med being monitored and evaluated. Is nursing providing ongoing re-assessment of need for med.
This is determined by obtaining a list of residents receiving psychoactive drugs, and reviewed clinical records as appropriate. If there are a large percentage of resident receiving these medications, surveyors must then investigate to determine that they are not implemented for staff convenience. Are there other interventions, such as sensory, tactile activites; soothing music, etc. that would help residents to feel calm and less fearful?
Yes…review any policies and procedures they have…interview the staff and ask what they do….look at the training provided to the staff for the resident specificly and their behaviors…ask them what they know about dementia and how it is treated and how they care for specific residents…interview alert residents for their observations and thougths on the residents in their facility…review the residents care plans…activity program…staffing
Surveyor team effort:
Once information is shared regarding my findings and input from other team members regarding their findings related to their resident reviews, the team may then determine to continue observations, etc. to detemine if the facility is following a systemic approach.
Miscellaneous responses of interest:
Some facilities have a heavy psych population and I try to make sure these residents are getting the proper care with my chart review. It is easy for a practioner to just pop in, do a real quick look at the resident, scribble a note and bill the resident. But then again, with some residents, the meds they are getting is what manages them day to day. So if it works, it is best to leave it alone. Residents with dementia are not going to get better. They will have periods of stability then decline.
We don't see systems in place except paper policies from corporate hierarchies. It all comes down to the leadership of the administrator and DON. If they are both good, the facility practices good care. If they both lack skills, the whole building craters. Poor administrator +Good DON = good nursing care. Good administrator, poor DON = a building struggling to stay away from the cliff's edge.
Yes. Usually most facilities have a committee that monitors those folks receiving antipsychotic medications. I like to talk with those running that committee to see what/how things are done, and then I will address whatever issues I have with my resident to see if they had discussed it, had they IDd there was an issue, should GDR be attempted, etc. I would also talk with the direct care staff and charge staff to determine just how they identify issues, monitor them, attempt to intervene and/or reduce the behaviors a resident may have, etc.
Yes. Where is the resident located. Is the environment clean, calm and nurturing. What activities are available. How are ADLS provided. What special safety devices are provided and maintained.
Question 9: When investigating F329 deficiencies, do you evaluate the role of the consultant pharmacist, physician, nurse practitioner (NP), physician’s assistant (PA), medical director, direct care staff, family and other members of the interdisciplinary care team? Which ones? How?
The majority of the 401 Surveyors responding to this question indicate that they evaluate the role of most of these professionals and family members, but appear to do so to varying degrees. Many indicate that depending upon the issues they are investigating, they focus more on particular individuals and concerns, as they arise.
All are evaluated:
All are evaluated. if facility uses a multidisciplinary approach, each should be and is expected to be aware of what's going on with the resident up to and including medications used in the resident's care and treatment.
all healthcare professional and ancillary staff members involve with the reisdent.
do interviews, record reviews involve with the resident
All of them. determine the facilities plan for incorporating all these entities in resident assessment., when to pull in certain memebers throughout the care interim as the resident response and condition warrents.
The roles of all staff, and also family dynamics are reviewed to try to understand the resident's needs. By interviewing the resident if possible, and the family if available will help to obtain a picture of the resident's life long personality and behaviors. By doing this, the surveyor has a more comprehensive understanding of the individual resident. Before direct care staff, physicians and extenders, pharmacists, etc. can be reviewed, one must have a clear understanding of the resident's needs.
yes, consultant pharmacist's notes or phone call
physician, NP, or PA usually through consultation by facility staff
Medical Director , usually throught consultation by facility staff
direct care staff through interview and discusion
family through interview
social worker, activity director, food service supervisor through interview
therapy staff through interview
Yes. All members of the interdisciplinary team, including the family, should have input into the resident's care, especially when antipsychotics are being used. Each team member should show how different methods of care they have attempted have failed before using "chemical restraints". But I do believe that the medications are necessary at times, but only as a last resort to prevent injury to the resident or others.
All are evaluated (with further explanation/rationale):
All involved with the resident should be interviewed regarding the use of the antipsychotic–family and resident should be asked regarding what education/information was provided prior to initiation of the medication? Was informed consent given?
Pharmacist should be interviewed regarding knowledge of antipsychotic usage in the building and his/her involvement with the IDT regarding reduction plans
All of them by determining who is directly involved in the medication regimen, i.e. nursing, consultant pharmacist, MD, etc. Observe, interview resident and review clinical file for side effect / behavior monitoring and GDR attempts. Interview family and observe family / resident interactions as well as interactions family / resident and staff
All
look at the pharmacist recommendations, how thorough is the psych eval and are they willing to do a GDR, does the physician just copy the previous months notes or does he appear to really be looking at the patient and info.
what is the nurse documenting as far as behaviors. if no behaviors what are they doing, are they using non-pharm methods prior to drugs.
All. The order and follow-up dose adjustments orginates with the AP,NP,PA,MedD. Direct care staff and family, etc are responsible for monitoring the effects of the antipsys (observation of positive and negative effects. They act as a advicate for the residents…..Start low and go slow. If the AP has not acted in drug reduction, or refuses to take the Pharmacist recommendation the DON Administ needs to seek the assistance of the Medical Director.
CNA/Nursing: do they know what care to provide for individual resident. How to interact with resident with dementia? what type of dementia resident diagnosed with? and how to interect for various diagnoses? What to report to LVN/RN charge nurse? What kind of training received?
Review CNA documentation.
SW- has SW provided necessary assessments? Communication with resident and family? What is SW role? Review documentation.
Activity Director: how AD interacts and provides activities for resident?
Yes we look at the role each is playing, reviewing progress notes, physician orders, checking to see how often the physician comes to see the resident. We interview the family to compare the resident's status before and after admission and if they are notified of medication changes. We talk to the medication nurse to see why meds are given and evaluate her knowledge of the resident. we talk to staff and activity personnel to see what alternatives they try or how they occupy the resident to reduce behaviors.
yes. I look at their notes and see what kind of contact they're making with the resident. Do they just come in and consult with staff, or are they actually spending some time with the resident and discussing how they feel about their meds?
Yes. I look to make sure the consultant pharmacist is reviewing the resident's medications on a monthly basis and to make recommendations for reductions with antipsychotic medications or to determine if there are duplicate therapies. I also would expect to see the medical staff to be evaluating the resident for side effects of medications and to determine if a reduction could be initiated. The direct care staff should be monitiring the resident and reporting any side effects or changes with the resient.
Sufficient staff remains a concern. One Surveyor summarizes the problem in very few words:
I look at all their documentation. Rarely do I have the time to interview the MD or NP. It sometimes seems that they are all a different page about dementia care. The nurses call the MD and say that the resident is yelling and screaming. They do not have the staff and time to spend time with the resident, to even see if they can get the residnet to calm, or refocuse, or redirect, or do an activity with the resident at that time, so a med is ordered and thats that.
I evaluate the role of activities and make a determination if there is enough staff (CNAs and Activities) to have enough time to spend with dementia patiemts.
Some Surveyors note concerns about the truthfulness of staff and others, affecting the integrity of the survey process:
If I can review the nurse notes and then try to interview these staff; interview a family member; sometimes will interview consultant pharmacist and interview other staff especially in regard to policy/procedure; all these interviews can be helpful if these folks are forthright and available and provide honest information; but sometimes they tell you inaccurate information or misleading info which doesn't get revealed until last day of survey.
Coordination/cooperation/communication, and follow up:
I look at if the pharmacist has monthly checks and recommendations, If the NP, PA or MD followup on recommendations. I will look at the facility's process for notifying the MD when the pharmacists makes a recommendation. Coordination is important and I check to see if psych MD's recommendations are followed up by MD and nursing. Checking for coordination with all team members and how or if family is aware of drugs being admin.
Look at communication between pharmacist and physician. I will question nurses and DON on communication techniques. I ask direct care staff to describe behaviors and what they are responsible for when they occur. I ask family if available, of changes and their understanding of the drugs. I ask resident if possible, of their understanding of the drugs.
Yes, we look at all of these team members. Which physician orders the meds, does the pharmacist look at GDR, does the staff communicate that with the ordering physician. Is the medical director involved in the policy/procedure. Do staff talk with the family about giving the meds, do other team members communicate with the direct care staff for changes.
Yes.
We should look for medication regimen reviews by the pharmacist.
The physician should respond to the reccommendations in the affiratie or teh negative but they should respond. Nurse practitioners should do thesame.
The medical director should set policy to direct staff not to administer antipsychotics unless necessary for the well-being of the resident not the weel being of the staff.
The direct care staff in the facility should document side effects if any, notify physicians and or pharmacists. They should communicate with each other about the resident. Sometimes communication with family or friends to the resident either in person over the phone could be exactly what the resident needs but none of this is possible without COMMUNICATION.
You have to look at all individuals involved in the care of the dementia resident to ensure they are on the same page, are communicating with one another to ensure continuity which is key. Do this through observation, interviews, record review.
Surveyors make particular mention of time constraints:
Honestly, I wouyld say that although we try to evaluate the role of these clinicians, time is a factor, It is rare we would have contact with the consultant pharmacist. we are more likely to see and interview the staff, including the CNAs and nurse and families.
I find it hard to initially evaluate the roles of various individuals listed above because there isn't enough time.
Yes I would evalute the role of th econsultant pharmacist, physician, direct care staff, family, psychiatrist/psychologist, social worker, etc. It could be any combination of the above or all. It would depend on how much time I had to investigate. The ideal to me would be to speak with almost anyone who is involved, interview them regarding the mdication, if there has been changes in behavior, etc. This still depends on how much time I have been given in while on survey. If there is limited time/staff on a full health I would try to focus on the family (if available and it's family that visits oftern). Direct care staff, psychiatrist/psycholigst/medical doctor, and the DON. I would interview the above staff medications/behavior/changes etc.
yes, due to time, concentration is on the recognition of the medications that the residents are on through MARS, facility teams, pharmicist recognition that the medication needs a GDR and the physician documentation if a GDR was completed or the reason that it was contraindicated.
yes, except not usually medical director. Psych consult, physician, pharmacy and direct care staff are usually reviewed, observations are made, but limited due to time constraint.
Surveyors note that their analysis is factually dependent:
Depends on the facts of the individual case, most often review diagnoses, then orders, then documentation of the monthly pharn review. Unless something arises to support looking at other disciplines would not look beyond this. However, if deficient practice is identified, may then look to other disciplines to see their respective roles in the process where the deficiency lies. Any time the is a deficiency identified, surveyors should review and assess back to QA, medical staff accountability for medical care, and governing body responsibility for overall care as they relate to the finding of deficiency.
Depends on the issue. Some issues require more involvement…others not so much. Interviews would be conducted with most appropriate individula.
none in depth unless have a concern-then depending on the concern -may focus on any or all of these
yes, all as needed, if i can't get my questions answered from documentation in the clinical record through progress notes, behavioral documentation, pharmacy reviews and recommendations, physician and psychiatric documentation, then i interview to clarify. I also interview staff and families to see if interventions are in place for the resident with dementia.
Surveyors note difficulties contacting physicians and other professionals as a part of their investigation. Surveyors often note problematic physicians and other hindrances:
Also the psychiatrist, dietitian, social worker, activity staff. Interaction with physicians, pharmacist is mostly done by reading progress notes and asking residents/ family about the care. Physicians are often vague in their progress notes with regards to rationales for psychoactive meds. At times, the facilities report to us that certain physicians become upset with the surveyors when they are questioned about justifications for medications or if the facility is cited for deficient practice as a result.
Generally, I will look at the consultant pharmacy report to see if issues were identified and reported to the doctor or NP. I think I have already addressed the direct care staff and other staff members. I sometimes talk to the doctor, medical director, or NP if they are in the facility. It is very difficult to contact them when they are seeing patients as they are not able to come to the phone. Sometimes it may take days to contact them, so I generally try to get as much information as I can from other sources.
In truth, often we cannot get physicians/medical directors/NP to call us back most of the time. The pharmacist may be consulted, but if the physician and medical director go against the pharmacist recommendations; the physician has the final say (this is true in an IDR as well). Direct care staff are always asked and involved in this process. The families (if we suspect a problem) are also almost always involved. Nursing staff/DON/administrator are also typical asked. Also, activity/housekeeping/maintenance/social service staff may also be asked.
of course, look at their documentation and determine if they did their jobs accurately. Talk to all staff if possible. Medical staff is the hardest because they get very angry when you question their decisions by asking questions. Sometimes they just blow you off to.
We actually look to see if a team approach as been done for the best care of the resident. We find sometimes the physician and pharmacist are at odds which is not in the best intrest of the resident. To many pacilities are afraid to question a physician when a resident is over medicated. We also look to see if the family has been consulted and asked about the resident before they came to the facility and how the medicaitons affect the resident. We want to see a team approach. If pharmacists and physician disagree we check to see if the medical direct has been involved.
we look at all of these. but it will do little good if the physician point blank says to you during an interview…I make the decisions for this resident and I say he/she will get this medication.. some physicians will become angry and say things we just can't repeat.
yes all are involved but the physiican and medical personnel may not be available fo rinterview. the record should reflect the inmvolved they ahve. Drug regimen review is always reviewed as to it being done monthly and what is reviewed. whther the information gets to the phsyician is reviewed nad what the physician does with the information.
CNA's should be interviewed because they know alot about the resident. so does the charge nurse.
Yes, but this is often difficult. Often, most of the information is only garnered through interviews. Facilities often lack a paper trail to show who sat at that table and identified the resident's symptoms were beyond non-pharmacologic intervention. Often there's no documentation to show the family member was apprised of the risks vs. benefits, etc. Many times the MDS Coordinator or the DON remember some of the details, but sometimes they don't. In my practice, I find the medical director does not have an active role in any of this unless he/she is the PCP of the resident.
Some roles are less likely to be evaluated (more selective evaluations):
All listed above except I usually do not involve the facility's medical director.
All of the above should be involved. Family and Medical Director are the most likely to be left out of this process.
All of the above through record review and interviews. The Medical Director if there is a more involved issue or more widespread concerns. Rev QA if indicated.
If I have concerns with a residents drug regimine, i will review the consultant pharmacist reviews to determine if they identified the same concern. If they have, then I will review to see if the physician responded appropriately and timely to the pharmacist recommendations. I never involve the medical director, direct care staff or family in my decision to cite F329.
Mostly the direct care staff and interventions of the clinicians by record review. Interviews of direct care staff and clinician as needed. I review the pharmacy reviews to see it they addressed GDR. Family interviews less frequently.
pharmacist recommendations and how the facility & MD/NP respond to theose. How the direct care staff actually work with the resident and what the care plan indicates. I am looking at all the information and seeing if approaches are tailored to the individual resident.
The consultant pharmacist is used mostly to see if they understand the need for a GDR and make recommendations. The physician is usually not consulted unless there's negative outcome. The direct care staff is usually all I need.
Yes, all of the above. Maybe not the medical director unless they were the physician of the resident being reviewed unless there were issues I felt the medical director had not been made aware of or if he was made aware how he had addressed these issues.
Some Surveyors offer expansive explanations, describing far reaching efforts:
All of the above. Observations of all as necessary, record reviews related to anything related to medications, review of pharmacy reviews and consult notes, review of labs relevant to the mediications received. Interviews with any of the above as necessary. Review of policies and procedures related to medications. Ask QA questions related to medications. Look at patterns in the facility related to medications.
Consultant pharmacist- look to see if pharmacist providing consultation to facility-doing medication regimen review consistently? Making recommendations- is the facility following up with suggestions?
Physician/NP/PA: Is resident being followed routinely? Is facility communicating resident's signs/symptoms or behavior changes or need for increased/decreased use of medication? Is physician addressing pharmacy recommendations? Attempting to taper antipsychotic meds per protocol or provide explanation for continued use of med? Documenting effectiveness and need for medication. Surveyor to review physician progress notes and orders.
Nursing/ DON: reconciling phsician orders? aware of and monitoring resident for s/e's of meds. Using meds as ordered. Aware of indications for use of med. Communicating with physician, family and pharmacy as needed and per policy? Review NN's and other pertinent documentation.
Consultant Pharmacist-review medications/diagnsosis/length of usage of medications whether they identified irregularities and reported to the physician in their monthly report.
Physician, NP, PA-Actual accuarate assessment of the resident, diagnosis, medications including how long the resident has been taking the medications, GDRs, responsiveness to Pharmacist reviews.
Team-Accurate individualized resident assessment, reporting findings to team, development of an individualized care plan, providing interventions prior to medication administration, re-evaluating interventions, making sure line staff are aware of the individualized care plan and are following it, staff training
Family-staff interview with families to gather history and if possible have the family be part of the interventions.
Direct care staff/IDT: Knowledge of recommended daily thresholds, requirement for non-medicinal interventions, on-going monitoring of target behaviors, observations of interactions with resident.
Physician/NP/PA: Documentation of rationale for medication and appropriate responses to consultant pharmacist's reviews.
Consultant Pharmacist: Identification of excessive dosages, review of behavioral tracking, ensure PRN medications have documented non-medicinal interventions, appropriate communication with physician of identified irregularities.
Medical Director: Involvement as liasion between facility, consultant pharmacist, and physician, when medication regimes do not adhere to recommended thresholds or accepted standards of practice.
Look at the pharmacy consults to see if GDR's are being done and if a problem is found interview the pharmacy consultant.
Review if the physician has seen the resident, if the physician has documented the reason for the medication and continued justification for the medications, if the physician has signed the pharmacy consults and recommendations and given a rationale to continue or discontinue the medication. The nurse practitioner would be similar. The medical director may have addressed the antipsychotics during QA or if the facility could n ot get in touch with the residents physician in an emergency. The medical director would also have been involved in developing policy and procedures for the facility in regards to antipsychotics.
Direct care staff may be completing behavior monitoring sheets and should be reporting to nurses behaviors and or problems with the resident. The nurses may be documenting behaviors, writing nurses notes, incident reports concerning the residents, doing monthly summaries, and documenting if medications are effective after they administer medications.
The family should be included in making decisions about medical treatment and should be able to assist in what history the resident has, their normal behaviors, medications they may have tried in the past, current mood and behaviors they have observed, and family history of illnesses.
Everyone involved with caring for the resident should be included.
Pharmacist should monitor for drug side effects and interactions and recommend reductions. The physician should evaluate for physical causes and alternatives to med. The NP and PA should observe the resident in the environment to evalualte services, physical and mental status along with effectiveness of drugs. The medical director should track the amount of medications and problematic behaviors in the facility and work with staff to reduce them. Direct staff should be trained to intervene with behaviors and assess for changes and effectiveness of approaches. Family should provide information about past history and approaches that may work. Interdicsiplinary team should evaluate the resident in terms of their knowledge such as social functioning, nutrition, recrecreational and theraputic.
Physician evaluates resident symptoms and orders with assistance of RNCP and PA for ongoing evaluation and possible changes.
Pharmacist monthly reviews of drugs, labs and assoc. tests for ongoing review of drug,dose, safety, posssible dose reductions in concert with physician; Direct Care/nursing staff administer and keep a recorded awareness of resident drug response; Medical Director, family and therapists, dietary, etc are informed of individual medication as it applies to each person treatment plan and goals for best possible individual outcome.If problem in past–did quality assurance review for problem solving?
Pertinent to particular issues:
These individuals would be evaulated according to how their decisions affect use of anti-psychotic drugs.
Evaluations would depend on which individuals are pertinent to the particular issues.
Yes we interiview the pharmacist especially if there has been a GDR for a certain medication. If the Physician did not agree with the change we consult him. If the facility has a NP in the facility we will interview that person as well. We always ask the family what information they know about drugs that they sign an consult for.
Difference in the way in which Surveyor’s professional and work background affects the analysis:
As a social worker I mostly review employee files (direct care and othe members of the team). When necessary I interview doctors, pharmacist, NP or PA. I usually ask question of my team mates that are nurses. (Social Worker)
By linking the information reviewed with the federal regulations related to pharmacy and physician services. (Social Worker)
Yes all involved in residents care. Nurses, Pharmacist, Physician, Nurse Practitioner, Medical Director, CNAs, Charge Nurse, Director of Nurses, Administrator, CP Team, Social Services, Activities. (Social Worker)
Yes. Some of the disciplines if not all listed should be directly involved. Some of the individuals listed may not pracatice in the facility ie., NP, PA. If all those listed do practice in the facility and are involved in providing care you need to evaluate how they participate usually through their documentation and possibly interacations/interviews during the survey. Pharmacist plays a significant role in assessing the medication regimen. Physician needs to respond to the pharmacist's recommendations and examine any medical issues relating to resident possible causing behavior(s) . If a physician is not cooperative the medical director may need to intercede. Direct care staff play a significant role in communicating daily info regarding resident. Family can be valuable from life long history viewpoint. Documentation-care plans and care plan meetings. There may also be a correlation from a nutritional standpoint and the dietitian's documentation. (Dietician)
Many Surveyors cite observation, interview, and record review for performing these tasks:
Yes, all of those listed above. I perform this task by record review, observation and interview.
Yes. Potentially all of them. Distressing behaviors in a resident with dementia can come from many sources and key information can come from any of these participants and have the potential help the resident, without resorting to the use of antpsychotics. I use observation, interview and record review to determne if all involved parties are effectively communicating any key information with one another and that it is being incorporated and executed as part of the ongoing plan of care.
Question 10: When investigating F329 deficiencies, whom do you interview?
Similar to most Questionnaire responses addressing the writing of F329 deficiencies, the 401 responses to Question 10 regarding interviews are relatively “theme consistent.” Commonalities are found throughout responses and some Surveyors also indicate when their interviews are “necessary” and “possible.” One Surveyor’s list, although not all inclusive, is illustrative:
– resident, if possible
– nursing staff
– family, if possible
– PCP, if possible
– pharmacist, if possible
– acitivty director, if necesary
– social worker, if necessary
– therapy staff, if necessary
– food service supervisor, if necessary
– admiistrator, if necessary to determine policies
Another list identifies typical Surveyor rationale for choosing interviewees:
All involved parties: physician, nurses, aides, pharmacist, social worker, activities personnel, family members. Anyone who can better inform me of the need or lack of need for a specific psych medication.
Surveyors sometimes identify interviews rarely identified by others, such as “spiritual” staff:
All staff involved with care (physical, spiritual, medical and activities) and Family as available.
Most Surveyors report interviewing everyone “involved in the care” of the resident, but some also point to “anyone involved in the…history of the resident”:
Anyone involved in the care and history of the resident.
Surveyors regularly comment on difficulties encountered when important interviewees are “unavailable.” Several Surveyors describe physicians being unavailable or uncooperative, which are both noted by Surveyors as being problematic, not just in response to this Question.
See question 9: In truth, often we cannot get physicians/medical directors/NP to call us back most of the time. The pharmacist may be consulted, but if the physician and medical director go against the pharmacist recommendations; the physician has the final say (this is true in an IDR as well). Direct care staff are always asked and involved in this process. The families (if we suspect a problem) are also almost always involved. Nursing staff/DON/administrator are also typical asked. Also, activity/housekeeping/maintenance/social service staff may also be asked.
As noted above, the care staff, CNA and nurse, the DON, family if avaible, , if the doctor, CRNP is available they may be interviewed.
Charge nurse, nursing assistants, sometimes families, resident if able to, pharmacy if necessary, the physician when available, activities, the director of nursing, sometimes social services.
Nursing staff and residents are among the top priority interviews for Surveyors. Pharmacy also tops Surveyors’ lists. Certified nurse assistants and direct care workers are nearly always included in the list of interviewees. In many instances, but not all, family members are included. Surveyors infrequently mention members of the Quality Assurance Committee as interviewees.
MDS staff are sometimes noted, but not often:
Attending and or NP, Nursing Staff, GNA's, Consultant Pharmacist, Psychiatrist, Psych NP, Activity Staff, Family, QA nurse, MDS staff, any person involved in resident care.
Sometimes Surveyors indicate that their interview decisions are dependent upon what they learn from observation and record review:
Depending on how much I can learn fro observation and record review. If I have a deficiency I will interview direct care staff on various shifs, Scocial services, activiteys, and if necessary the family.
It is common for Surveyors to indicate that they exercise professional judgment when deciding upon interviews:
Depends on the deficiency, could be any staff from front line to physicians to QA and/or leadership. Every deficiency has systems that underlie the identified concern – who you interview depends on which systems are in play.
resident and family if able, direct care staff, unit manager, consultant pharmacist, physician and possibly others–dietary, therapy, receptionist. depends on the resident and what behaviors are exhibited and where.
Resident, family member/friend, direct care staff, activity staff, MDS Coordinator, therapy staff, dietary staff, housekeeping, laundry, social services, other residents, Resident Council Officer/Member, Front Office Staff, Nursing, Director of Nursing, Assistant Director of Nursing, Unit Coordinators, Weekend Supervisors, outside consultants including pharmacist, psychologist, psychiatrist, dentist, dietitian, physician, medical director, NP/PA (who I interview depends on the resident's involvement with others and the behavior(s) exhibited).
Resident, if possible, nurse aides, charge nurse, DON, MDS coordinator, SSD, family. Also will interview others if the investigation leads to the pharmacist, etc. Sometimes will talk to the food service coordinator and/or dietician if there is weight loss involved.
Some Surveyors explain their rationale for interview decisions; one specifically mentioned interviewing nursing management about the regulations on antipsychotic drug use:
Direct care staff re: behaviors, Nursing staff re: medications and interactions, pharmacist for review of medications, physicians for justification/diagnoses for use of medications, family for specifics about resident including past history, resident for need for medication, understanding of purpose of medication and reason for use..
Direct care staff, aides, nurses, and often if available family members of the resident to see if they had any input into these medcations and how they think the outcome of these medications has or has not helped the resident. If available its also good to talk to the physician and pharmacy consultant if they are avaiable. When a concern is noted, I also like to discuss with social service to find out what involvement they have had and how they are assisting in making recommendations ot manage these behaviors.
-I interview CNAs to see how they would describe the resident in question's behavior, normal day-to-day demeanor and how the resident responds to care. If that CNA knew how often the resident received any kind of prn or is aware of the medications the resident took and what side effects the CNA should or might be aware of;
-Interview medication technicians and licensed nurse's on how antipsychotics are administered, what is documented, how they are montiored, who is involved in determing the need, etc.;
-Interview nursing management for expectations regarding antipsychotic drug use and what the regulations say;
-I may interview the physician and/or the pharmacist depending on what the issue is.
I would interview the resident if possible, family members, physicians and nursing staff. One of the most important persons to interview are the nursing assistants who provide the daily, hands on care for the resident. These aides are often overlooked, but are the backbone of any good nursing home care. Determine if they have been properly trained to care for residents with dementia, and if they are able to go to nursing with their ideas and suggestions for better care. They often are close to the resident's family and know much more about the residents, than the licensed nurses.
The Director of Nurses, the Charge Nurse, the Pharmacy Consultant. Also the nurse aides to find out what they have been told and what they know about the resident and the medication the resident might be on. I also find out from the nurse aides what they are reporting to the charge nurse. I also ask the Charge Nurse if she is communicating to the Pharmacist, NP, and others if she sees a change in condition with the resident that could be a problem with the medication being given. I will also talk to the Activity Director and sometimes the family if they are available.
Res, Family, Alert and oriented residents r.e. other residents – are staff medicating to keep them quiet?
staff – observations correlate? coordination of care>
whom ever i have to to determine if there is a deficient practice.
Some Surveyors mention “members of the committee to reduce antipsychotic drug use in the elderly” and members of the “psychotropic monitoring team” as important interviewees:
direct care staff, DON, members of the committee to reduce antipsychotic drug use in the elderly
the nurse, NA, physician/practitioner and pharmacist and anyone included in their psychotropic monitoring team.
A few Surveyors indicate they interview “everyone” involved in caring for the resident and “everyone” with knowledge of the resident.
Psychiatric specialists are noted by one Surveyor for interview difficulties, with accompanying observations:
I interview the residendt first, if possible. Then the nursing staff, then the the NPs, then the MD if If I see him there. Very rarely do you get to interview the Psych MD. The Psych Md will maybe see the resident once every 3-6 months. The Psych NP sees the resident more often–but usually just orders what a MD would–keep the resident quiet, and behaved–not snowed but very quiet and calm.
Physical and occupational therapy are hardly ever mentioned by Surveyors for interview:
Interview all staff involved with residents care — physician, ancillary services …psychiatric, psychopharm, pharm consultant, nursing and CNAs physical and occupational therapy to ensure that the resident was not experiencing a decline in mental/physical functioning
Only one Surveyor reports not conducting interviews:
No one. Interviews are subjective data. You need concrete facts such as documentation in order to determine the facility's compliance for F 329.
One Surveyor relies upon incident reports:
read incident reports, make calls to facility
Question 11: When do you expand your sample and what “triggers” or circumstances cause you to expand your sample or to inquire further?
The majority of the 401 Surveyors who responded to this question offer concrete explanations for expanding their sample and note a variety of “triggers,” or circumstances, for such expansion.
Many Surveyors list a wide variety of concerns that trigger an expanded sample:
If during the survey the team identified a problem with GDR's, if resident's were on antipsychotics without proper diagnosis, if we could not find a rationale for the medications, observations were made that residents appeared oversedated, or if a complaint came up during the survey. We might look at behavior monitoring, social service notes, falls, injuries of unknown origin, interviews with residents or families that concern the survey team. We may look at physicial health concerns like UTI's.
Our team will get together and review preliminary findings once we have had an opportunity to observe our residents and/or check the chart and care plan to see how well the facilty staff is addressing the use of antipsychotic medications. Generally, the resident will have an acceptable diagnosis, however, the facility staff will fail to document specific behaviors, i.e., most the time they simply record the number of times the resident had behaviors, and will not describe the behaviors themselves. It becomes a bigger issue if we observe displays of behavior and the staff's response does not coincide with the POC developed for that resident. We look at the use of PRN medications as well to see if the staff has identified an appropriate reason for its use, monitored its effectiveness, and/or communicated w/the physician in the event that it wasn't effective. We lry to determine if anyone is actually responsible to assess/evaluate the behavior sheets and whether or not adjustments are being made. If several surveryors are having the same issue, we will expand, or if one surveyor has noted a significant concern, then we will expand just to make sure that event wasn't an aberrancy. A lot of the time the facility staff simply fail to assess the effectiveness of their actions, i.e., if medication given, and/or they only identy that one approach was used to help diffuse the behavior and it often was not effective, but they didn't try anything else!
resident appears tired or sleepy all the time
staff don't really know the resident
diagnoses does not match the medication given
PRN's being used too frequently
PRN's being used without a reason why
care plan does not include information about medication or behaviors
no process to evaluate plan or reevaluate if plan is working
family/resident interview yields concerns
resident not involved in activities
non-pharmacological approaches not being used
Observations made of residents provide evidence of inappropriate staff interaction with residents with dementia. Residents identified with side effects potentially related to use/overuse of antipsychotic medications. Clinical record review resulted in lack of assessments, ongoing monitoring of effectiveness of meds or lack of monitoring for side effects. Lack of informed consents or lack of evidence the pharmacy consultant did medication regimen reviews. Lack of evidence facility staff/physician followed up on pharmacy recommendations. No non-pharmacological interventions prior to using antipsychotic. Continued use of med without re-evaluation of need. Irregularities in consolidated physician orders, duplicate medications or excessive use identified.
upon observations, if we see residents who are sleeping "all the time"
resisting care
high doses of medications
medication contridications
residents who are pacing and touching the exterior doors, reminds me of the dinosaurs in Jurasic Park trying the fences
Surveyors cite numbers of residents taking antipsychotic drugs (without documentation or diagnosis) as a reason for expanding their sample:
If record review shows a lot of antipsychotic drug use without any documentation of a diagnosis, documentation of a diagnosis without any supporting documentation of what constitutes that diagnosis, perhaps a dementia unit where many of the residents seem like they are incoherent or lethargic and unable to do anything (possible chemical restraints), MRR that are not done or do not have the required GDRs in place for residents who have antipsychotics in the medication regimine.
if there is a large usage of antipsychotic medications, if residents appear lethargic
Roster indicates frequent use of psychoactive medication w/o indication for usage, observation finds residents exhibiting s/e, IMs used as prn medication
If you have completed phase 1 and have a potential citation but feel due to the number of indivduals receiving anitpsychotic medications you may expand the sample in phase 2. This may help to confirm there are more cases involving a deficient practice. May change a potential citation level from a "D" to "E".
Use of multiple antipsychotic medications or inappropriate staff responses serve as a trigger:
If a resident is on two or more psychotropic medications, (antipsychotic meds) and if that resident has multiple side effects because of the meds and if the behaviors are not being identified or monitored and no approaches have been put into place. If the staff are not addressing the reductions of those medications and if the physician is not responding to the Pharmacists requests or the facilities requests for drug reductions.
If there is a poblem with one individual that may be cited individually. But with suspicions of wide spead problems the sample would be expanded. For example seeing Residents who appeaer "Snowed" or overly medicated. Seeing inappopriate staff responses to Residents with behaviors.
Many Surveyors cite their impressions about the facility’s organization and mismanagement of antipsychotic medications as their impetus to inquire further:
This has actually happened – we expanded when we saw a pattern – so the 3 resident's we reviewed we all had issues and decided to pick up another resident to determine scope.
This particular survey what "triggered" us was that we were seeing increases in the resident's antipsychotic medication with no justification and/or documentation as to why – Plus when we interviewed CNAs – they were telling us that they hadn't really observed any changes to the resident's behavior…nor did the Resident Care Nurse Manager had any clear answers for the increase..
Residents just sitting in a chair in their room, in the hall or at the nursing station or overly aggressive, loud,sad, tearful, pacing, disruptive residents. I observe to see if staff interaction takes place and how. Is the resident invited to an activity or taken to an environment that is more stimulating/calming. I consider that what I am seeing is the resident's baseline and how progressed their disease is. This does not give the facility the right to ignore the resident. And sometimes you come back the next survey and see the same or that the resident has decline.
A review of GDRs provides another common reason for Surveyors to expand their sample:
When there is no rationale for the continued use of the medication. No GDR or attempted GDR. Use of medication in the absence of targeted behaviors
Use of Prn medications without documentation of behaviors that justify use. No dose reduction or documentation substantiating not reducing a medication.
A few Surveyors indicate that they do not expand their sample. Some offer various explanations:
Not sure that our team does that.
I have not been in a survey where the sample was expanded.
Do not normally expand sample for deficiencies in F329 unless decide to carry over from Phase I to Phase II.
Haven't had to expand sample. We have sometimes had 5 out of 10 sampled residents reviewed for unnecessary medications with citations of 329.
I normally conduct complaint surveys and have not experienced survey expansion during my surveys using the QIS process
We normally don't expand the sample unless we find a consistent problem with an area of concern. We always include at least 4 residents with psychoactive medications on our sample.
Given that 10 residents are reviewed, it would be rare to expand a sample – I guess if we only had a sample of 2 residents with dementia who were on an antipsychotic and both had issues, I might talk to the team regarding a need to expand the sample
I have not yet been in a survey when the sample was triggered to be expanded, but would look for or initiate an expanded sample if the problem did not appear to be isolated or if a process problem was suspected.
Rarely for F329. If more information is needed or if substandard care is considered.
Have not had to expand the sample. There are many residnets that carry over for unecessary drugs to include antipsychotics.
Don't usually expand the sample
Never had to
haven't really expanded the sample
I have not been involved to date in a survey that it was deemed necessary to expand the survey related to F329 for antipsychotic medications.
Some Surveyors indicate they do not expand the sample because of the limited time they have to survey:
We usually don't expand the sample because of limited survey time. We expect facility to correct for persons cited and then to review all residents' medications and correct them for their plan of correction.
A deficient practice that places residents at risk. Surveyors are "supposed to" expand the sample more often but time is a resource we don't always have, we have to focus on areas of highest priority.
If the issue is identified in multiple residents, if there does not seem to be any interventions with the resident, if there is harm done, if the problem has occurred over a longer period of time, if none of the professions are addressing the problem. We do not have time on the surveys to expand the sample routinely unless there is a serious issue
Some Surveyors link sample expansion to poor or negative resident outcomes, controlling behavior, staff convenience, or chemical restraints.
Poor/negative outcomes:
Poor outcomes related to medications / behaviors
uncontrolled behaviours that impacts the health of both residents and others in the facility. injuries unaccounted for ,poor general condition of residents and sudden death …etc
if there is a signifiicant incident or if there has been a medicaian error.
if problems are found on phase 1 residents, the sample would be expanded. Triggers would be negative outcomes from the medication
Primarily, the sampled residents are reviewed to determine if there is a deficient practice and if so, how was the resident impacted. The sample is expanded if a pattern of negative outcomes is observed, or if substandard quality of care or immediate jeopardy is determined to exist.
When a resident has adverse consequences to the drug such as ADL decline, weight loss, falls, cognitive decline etc. and the facility has not identified the adverse event.
Adverse effects to drug are observed (Signs & symtoms)
Long term use of drugs
pharmacitist recommendations are disregarded
No Dx for use of drug
Black box warning not considered or lack of knowledge by staff
Problems with three or more residents with similar concerns. An egregious concern with one resident.
As a team we expand our sample and triggers when we identify a particular behavior/side effect – not done as I would like but I do expand my own sample when I see effects of overuse of psy. meds.
If falls triggered, wt. loss, dehydration, swallowing problems. Increase behaviors and decrease in ADL's. If no GDR's have been done.
Controlling behaviors, staff convenience, chemical restraints:
When medications are being used to control behaviors as a primary intervention, when dose reductions are not being attempted, medications being used without indication, side effects or adverse reactions not being assessed and monitored,
when multiple residents are on the same type of antipsychotic medications,
if the residents seem to be sedated during normal daytime hours
if the staff seem to medicate a behavior rather than attempt other alternatives
Sample would be expanded if there is enough evidence of chemical restraints.
If it seems the resident is getting PRNs for staff convenience or the side effects are excessive.
I look for multiple individuals who are on psychotropic medications and look for lack of other interventions not being tried first. I evaluate it from the standpoint are they using psychotropics as chemical restraints
I expand the sample when it looks like the facility is using medication as a way to control the resident(s).
when I don't see any interventions either in the care plan or not being implemented, I have cause for concern.
When the sample is expanded is usually because the team as a whole has found a pattern in the methodolgy of administering the psych medc, or simply administering for staff convienience.
When possibility of psychoactive medications are used for convenience, not medical purposes is suggested during Phase I.
Expanding the sample was based on the information gathered in the investigation. If it was found, during observation, a resident was treated with antipsychotic drug for dementia due to the convenience of the staff, the resident maybe added. During interviews, including resident council, there was suspicion of F329, there would be an expansion. There are many reasons a sample size maybe expanded. As everything, it just depends on the circumstance.
If there are issues with the use of anti-psychotic medicaitons such as no diagnoses, no GDR"s , usage without non-pharmacological interventions, an overabundance of residents on these medications, use as a chemical restraint.
Obviously distressed residents, inadequate behavioral interventions, signs of over-sedation or chemical restraint use, presence of physical restraints, ongoing behaviors, obvious side effects such as extrapyramidal symptoms/signs, no attempt to decrease medications, no monthly medication reviews or pharmacy recommendations, use of medication without diagnoses or medical indications, lack of other intereventions by staff. Concerns from family members about decline or care or residents. Lack of appropriate activities for cognitively impaired residents.
Some Surveyors expand the sample when unusual issues arise or answers “don’t add up:”
When a problem is identified with the current sampled residents. If a resident or family interview shows a problem or if staff mention anything unusual about medications and practices related to behaviors and residents with dementia.
If I feel uncomfortable about situation and see answers "not adding up".
if all cases that i look at have issues
When I identify a deficient practice when one resident I expand the sample to determine if other residents are being impacted or could be impacted by the deficient practice.
When a medication error is noted during medication pass observation.
Physician issues are noted by Surveyors, not just in response to this Question:
Its what the MD wants, so you back off. We are told –who are to to question the MD.
harm is noted…ie resident lethargic for significant periods of time and no underlying physical medical cause noted. Same medical practioner with a lot of residents on antipsychotic meds. No aactivities geared towards dementia resident.
Substandard Quality of Care is another trigger for Surveyors to expand their sample:
When the team determines there is substandard quality of care the sample is expanded or is the information we have is not enough for us to determine if there is a deficiencit practice or at what scope, the sample is expanded.
SQC; to see how widespread the problem is: ex. resident injuries related to antipsychotics; staff administering PRN antipsychotics without symptoms or other interventions attempted; no diagnoses for the antipsychotics; the side effects of the antipsychotics caused a potential for harm to the residents.
if majority of the four residents reviewed initially for antipsychotics were found to have problems related to F329, would expand sample if harm present and suggestive of SQOC or if needed addtional example to determine if pattern existed
Surveyors use pervasive problems, inconsistencies, or patterns to trigger sample expansion:
The triggers for expanding investigations into psychoactive drugs would be the percentage of residents receiving these drugs, and if other interventions are routinely attempted prior to administering the drug. Another determination would be if there are appropriate activites to ensure a safe and calm environment. Seeing 20 residents seated in a room watching the "Jerry Springer" show is not conducive to calm behaviors.
If I found inconsistencies or potential findings, I would expand my sample. There are many "triggers" including not having comprehesive pharmacist reviews, lack of follow up with the facilty and/or physician, lack of an appropriate diagnosis, lack of assessment, care planning, monitoring or attempting GDRs if needed.
If there is a pattern of non-compliance in sampled residents, then would expand to determine if a widespread problem.
We expand our sample to include more resident's on antipsychotic medications when the survey team identifies a concern that appears to be pervasive throughout the facility with the residents being reviewed. We often do not have a lot of residents on our initial sample who receive anti-psychotic medications unless it was triggered during pre-survey prep as an area of concern.
Particular drugs sometimes cause Surveyors to expand the sample:
If we find residents with diagnosis of dementia who are on antipsychotics without adequate justification/documentaion of behaviors/interventions to support the use. Residenta with dementia who are on Geodon, Haldol or Risperdal are red flags.
Residents given injectable antipsychotic medications. No non pharmicological interventions implemented or care planned. Observation of many residents with behaviors and behaviors affecting others. Staff treatment of residents that is inappropriate during observation. High number of PB 22s on pre survey review.
One Surveyor indicates CASPER data may trigger an expanded sample:
If the CASPER data has a facility with a high percentage above the national average would trigger an expanded sample.
Some Surveyors use fixed numbers to trigger an expanded sample:
If three of triggered resident's have problems or based upon observations.
When there is a 5% medication error or more.
we were looking at 10 unnecessary meds each survey which seemed to capture antipsychotics The team would meet and keep all posted of findings so if concerns were identified others would check for same issues. We would expand sample if concerns identified in all sampled residents to capture scope
Only one Surveyor indicates that “staffing concerns” trigger an expanded sample:
In cases of substandard care would expand the sample. In other situations, concern is carried over into phase two. As a team, we try to conduct extra interviews and observations when needed. The group interview often gives us areas where to inquire further (such as staffing concerns).
Only one Surveyor indicates that complaints from staff or residents trigger an expanded sample:
When we receive any complaints from staff or residents we will expand our sample to include any concerns and if we see deficient practice that will trigger our team to dig further
Question 12: What records do you routinely obtain/review in order to investigate a potential F329 deficiency?
There is a great deal of commonality among Surveyors in which records they routinely obtain and review in order to investigate potential F329 deficiencies. Nevertheless, there is also some significant variation. For example, Surveyors’ background or professional discipline appears to have some influence on the specific records that particular Surveyors obtain and review. Additionally, some Surveyors appear to approach the records they seek from a broader “facility” emphasis (e.g., policies and procedures), as opposed to a more “individualized” resident focus (e.g.,. MDS). Some Surveyors place more emphasis on historic records, such as hospital discharge records, while others concentrate on more current events, such as GDRs. Multiple Surveyors note that the selection of records they routinely obtain and review is driven by each particular issue being investigated.
A near-global list of the records obtained and reviewed, in no particular order, includes:
a) Physician orders, visits, progress notes,
b) MAR,
c) Behavior Monitoring Sheets, flow charts, etc.,
d) Hospital Discharge records,
e) Social history,
f) Psych progress/consult notes,
g) Consent forms,
h) Nursing notes, etc.,
i) Pharmacist notes, reviews, etc.,
j) Clinical record,
k) Care Plans,
l) Policies and Procedures,
m) Behavior Committee notes,
n) Interdisciplinary Team notes,
o) Lab work,
p) Incident/Accident/Grievance Reports,
q) Resident’s record,
r) Diagnosis,
s) MRR,
t) Social Services notes, assessments,
u) CAN documentation,
v) MDS,
w) GDRs
x) Psychotropic Med. Review meetings,
y) “Thinned” resident records, “Purged” records,
z) Dietary notes, etc.,
aa) Nutritional progress notes and weights,
bb) Progress notes from all disciplines,
cc) Activity Logs,
dd) 802, 672
ee) Falls data,
ff) TARs,
gg) DARs,
hh) Side effect monitoring sheets,
jj) Residents sent to acute care settings,
kk) List of all residents on antipsychotics,
ll) Reference manual(s) used by facility,
mm) H & P,
nn) Casper,
oo) Lists of meds administered, (am) (pm),
pp) Drug manufacturer information/black box warnings/instructions/etc.,
qq) Drug handbook,
rr) Sleep Schedule,
ss) ADL records,
tt) Physical Therapy, Speech Therapy, Occupational Therapy, Rehab. records,
uu) AIMS (Assessments involving antipsychotic medication) testing,
vv) Staffing records, evidence of Staff training/inservice records,
ww) Braden assessment,
xx) Admission assessment,
yy) POSs
zz) X-rays,
aaa) Whatever records QIS picks,
bbb) Grievances,
ccc) Family conference notes,
ddd) CAA,
eee) Prior citation history.
Some Surveyors offer explanations for the records they obtain and review:
The Medication Administration Record, the Physician's Order sheet, the nurse's notes, the Medication Regimen Review, the behavior monitoring sheets and the Controlled Substances record to see if the administered medications correspond to the MAR.
MDS information (meds received and diagnosis, behaviors or mood states), Physician's Order sheet, psychiatric progress notes, physician's progress notes, nurse's notes, assessments involving antipsychotic meds (i.e. AIMS), MRR and GDR, pharmacist recommendations to the physician and how they are followed up on, possible labs.
Clinical records,POC's MAR, pharmacy reports and behavioral monitoring records, sometimes incident and accident reports to determine if side effects/ medication use are related to falls .
I look at medications both routine & prn, sometimes the initial orders & corresponding progress notes for rationale. I always look for psych consult notes, & any behavioral documentation. I review the Care Plans, and if a medication was increased or changed, I review nurses notes and care plan to see why. I always look at pharmacy reviews too.
The Surveyor’s professional or work background may have some influence on record selection:
Nurses notes, social service notes, physician notes, monthly order sheets, Medication administration records, care plans, dietitian notes, monthly weights and Lab values if they apply. (Dietician)
MDS, care plans, physician's orders, MARs, nursing notes, social worker notes (Social Worker)
Clinical record, nurses notes, physician notes, progress notes from all discplines, review neccessary facility policies, pharacy reviews, psych notes, psysocial notes, care plans. (Social Worker)
The medical record, lab reports, ADL records, behavioral monitoring sheets (if available), and the drug regimen review. (Pharmacist)
The records of disruptive, distressed, and/or lethargic residents and those with weight loss and decline in ADLs. (Dietician)
I routinely review the following :
– resident's current physician's orders,
– the medication administration record,
– the consultant pharmacist's monthly evaluations,
– the consultant dietitian's notes
– Psycharist or Psychologist reports
– the incident and accident logs [review if there had been any changes in antipsychotic meds/or doses] (Dietician)
Facility policies and procedures are often sought by Surveyors:
Physician's orders, Pharmacist consultant notes and requests. Behavior monitoring, MDS/Care plan. Nurses notes, Physician's progress notes. and the faciities policy and procedures regarding the use and reduction of psychotropic drugs.
Medical Record, Care Plan, Pharmacy Reccomendations/Reviews, Social service Notes, Nurses Notes, Physician Progress notes, Facility Policy for the use of Antipsychotic medications
The facility's psych drug policy. Any documentation relat4ed to the use of psych drugs as identified in the policy. Medication Administration Records for documentation of routine psych drugs as well as PRN psych drugs. The RAI and CAA. Daily progress notes that would record any resident behaviors (or lack of behaviors)
Medical record, Psychotropic Monitoring, Pharmacy Consultant report, nursing documentation of behaviors, MDS, Care Plan, Psychiatric or Psycology consult reports, facility policies regarding the use and documentation of pschotropic medications
Surveyors indicate that their record review depends upon the particular issue:
Current medical record for diagnoses (preferably from Physician Order Sheet), Pharmacy review/consults/recommendations, lab work, history and physical, physcian and nurses progress notes and anywhere else depending on the particular issue.
Clinical record,MARS,Pharmacy, Consults,Care Plan and anything necessary for a thorough investigation.l
residents record, consent form for psychoative medication, progress notes from both physician ,pyschaitrist, nurses notes and monthly pharmacy reviews or recommendation, behaviour monitoring flow charts and any other documnts deem necess to enable the case
medical record, old chart from their previous admission like if they have been to the hospital, MAR, closed records, History and Physical, whatever it takes to make a decision.
Assessments, care plan, physician / NP / PA notes, pharmacy review and follow-up, psychotropic review notes, IDT notes, MAR/TAR, informed consent, lab work, monitoring, information from mental health practitionors and anything that is found to be pertinant.
Residents with a psych diagnosis, taking psych. meds, behavior issues, falls
Some Surveyors offer a unique perspective concerning certain records they obtain and review:
residents on antipsychotics
residents recently sent out to an acute care setting r/t behaviors
residents identified to have behaviors
Medical records of sampled residents (Orders, diagnoses, MDS, labs, side effect assessments, care plans, nurses notes, physician and psychiatric progress notes, other consult notes, cna notes or data.
pharmacy reviews of sampled residents.
roster matrix, QI's
Resident's medical record- Physician's orders, Nurses notes, social service notes, activites notes.
Drug Regimen Review-Pharmacist recommendations
Activites Schedule
MDS; Care Plans; Physician Orders and Progress Notes for rationale, to include psychiatric; Diagnoses List; Antipsychotic Consent Forms; Consulting Pharmacist Recommendations; Nurses Notes; facility Policies for antipsychotics; any Reference Material used by the facility for guidance; Dietary Notes; Social Services Notes.
On survey- add Casper reports
pharm review
physician orders
psych notes
physician notes
TAR
behavioral flow sheets
care plans
MDS
drug manufacturer website
Physician's orders, MARs, Behaviorial Monitoring, Care Plans, assessments, Medication (psychotropic med meeting notes), pharmacist notes, nursing notes, drug handbooks, treatment records.
I would review:PHys. Cert, MDS, Care Plan, Med sheet, History, sleep schedule, activity, dietary, Psycho social
Resident's medical record, MDS records, 672, 802, MAR, H&P, Consults, Nurses Notes, Dietary Notes, Activity Notes, PT/ST/OT notes if pertinant,
What ever documents I can get my hands on including CASPER Reports,
Pharmacy review, physician progress notes, behavior tracking, MAR, facility policy, nurses notes, physician orders, diagnosis list.
Medication records, nursing notes, behavior logs, incident reports, social service notes, physician progress notes, monhtly pharmacy reviews and recommendations, hospital notes, manufacturer's instructions for medications.
incident acident reports, medication orders, MAR, pharmacy review, policy and procedure, manufactures instructions for use and nurses notes.
Residents who are on any type of medications but most importantly those medications that have a black box warning or the medications that would put a resident at risk for serious adverse side effects.
General staffing information, staff training, and in-service records are sometimes sought:
Medication administration records, behavioral flow monitoring records, care plans, AIMS testing, nurses notes, care conferences, consultations, physician orders and progress notes. Also look for eveidence of staff training.
Clinical records to review nurses notes, pharmacy recommendations, social service notes, care plans, MDS assessments, nursing assessments, all telephone orders, lab values, psych referrals, physician progress notes, hospital information, psych notes, and medication profile. The facility policy on psych medications and/or managing behaviors. The facility staffing schedules. Also, staff training on dementia and managing behaviors.
Resident clinical records review PCP notes and/or other prescribing physicians, nurses notes, social worker notes, pharmacy consultant reports, inservices, accident reports and grievances.
physician's orders, nurse's notes, physician's progress notes, psychiatry consults/progress notes, care plans, MAR's, pharmacy review sheets, gradual dose reduction reviews, behavioral sheets, staffing reviewed if observation shows few staff members
Medical record, monthly pharmacy reviews and recommendations, MDS and CAAs.
In addition I review the facility's policies and procedures related to antipsychotic medications. I also look at inservice over the last year related to behaviors, dementia, etc.
Most recent admission documentation to include previous health care staff impressions; physician's notes and h&P; psychologists and psychiatrists assessments and progress notes; behavior assessments; MDS, CAAs, Care Plans, direct care staff plan of care; pharmacy review; physician orders and POS compared to Medication Administration Record and Controlled Drug Records; behavior and PRN medication documentation; nurses notes; and staff training.
Family conference notes are mentioned by one Surveyor:
physician and medication records, social worker notes, family conference notes from meetings with family or POA
Prior survey citations are mentioned by one Surveyor:
Behavior monitoring, history and physicial, MD orders, labs, psychological consults, MD and CRNP/PA notes, nurses notes, activity notes, prior hospital records, pharmacy reviews, policy on dementia /behavior related care interventions, care plans, prior citations on surveys, MARs, related grievance or incident reports.
One Surveyor offers a critique of provider computer programs:
all nursing records , pharmacy reviews, psyche and psychology notes to start with. Behavior documentation unless it is not individualized such as one finds in the computer programs most facilities use.
Surveyors often mention incident and accident records:
MARS, MDS, Care Plans, Physician's Orders, Psychiatrist and Consultant Pharmacist records, Behavior Monitoring Forms, Incident/Accident/Complaint reports.
Care plan. Antipsychotic flow sheets, medication admin records, physician orders, pharmacy recommendations, nurses notes, physician progress notes, incident and accidents, social service notes, psych consults.
I&A….incl falls, weight loss (are they over sedated, and can not eat), pharmacy review and recommendations did the facility follow, Nurses notes for catastrophic events and what the facility did about the event…did they just medicate and remedicate…..review the number of prn mds given for behaviors.
MAR, MD orders,nutrition notes, psych notes, MD notes, pharm review, care plan, behavior flow sheets, any incident/accident reports for behavior
Physician orders, MARs (including monitoring sheets), Care plans, Consents, H&P, Progress Notes, Nurses Notes, SW notes, pharmacy notes. Any related lab work. Medication Regimen review. All assessments including MDS. Facility policy and procedures. In-service training. Incident/Accident log. Complaint log.
A few Surveyors mention PASRR as a source of record review:
– physician orders
– MAR
– Behavior monitoring sheets
– hospital records
– social history
– psych progress notes
– psych consents
– possibly a PASSAR
MDS, Care Plan, MD orders, RPh reviews, PASSR, MARs, side effect records, SW notes, Nurses' Notes.
Some Surveyors note purged or thinned records as important for their review:
The resident's current clinical record and any records that may have been purged regarding psych medication use. All pharmacy reviews and and physician's orders. All psych consults and any counseling consult or neuro consults if pertinent.
Medical records, pharmacy reports/recommendations and the responses to any GDR or D/C recommendations to these. It seems that the faciliies keeps these separate. Purged parts of the chart if necessary if the resident has been there long.
The current clinical record, thinned records, behav ior monitoring tools, MAR';s, Careplans, physican orders, copnsultant pharmacist's documentation.
Medical chart behavior monitoring sheet, psychatrist consult, pos, Mar, old record if it was thinned fro the record. consultant pharmacist review sheets.
Some Surveyors refer to the QIS process as determinative:
Whatever records QIS picks
Since QIS these records are chosen. When we review a resident on antisychotics we look at those triggers. We do not have the luxury of tiime to routinely chose extra individuals unless there is something so obvious we can not overlook
computer picks them
Question 13: Are there one or two key elements that determine whether you cite F329? What are they, and why are they key to your determination?
The 401 Surveyor responses identifying one or two key elements in determining whether they cite F329 are, for the most part, consistent. A list of many of these key elements, in no particular order, includes:
a) Diagnosis, justification for use,
b) Harm, potential for harm, poor outcomes,
c) GDRs,
d) Behavior/Etc. monitoring,
e) Amount of medication,
f) Multiple medications,
g) Interventions prior to use, and thereafter,
h) Documentation/lack of documentation for use, etc.,
i) Following pharma recommendations,
j) Data supporting PRN administration,
k) Risk/Benefit analysis,
l) Abnormal labs,
m) Lowest effective dose,
n) Side effects of medication,
o) Duration,
p) Care plan,
q) MD involvement,
r) Pharma involvement.
Many Surveyors offer broad and extensive key elements (more than two) involved in their decisions whether to cite F329 antipsychotic drug deficiencies:
Failure to follow the requirements such as medication prescribed without adequate indication for use, or in the absence of documented behaviors, no attempts at gradual dose reduction, inadequate documentation to justify medication use or continued use.
Resident outcome, documentation to justify appropriate indications for use of medication, behavior assessment, behavior monitoring, documentation of interventions attempted prior to medication use, evidence of attempts at gradual dosage reductions.
An absence of behaviors and no attempts at a GDR when there is no documented evidence with supporting information that a GDR would be contraindicated for the resident – such as a psych history and recent attempts of a GDR that failed. I also cite 329 when routine monitoring is not being done – such as monthly summaries that review the medications in use, the behaviors targeted, the number of behaviors exhibited that month and the use of non-pharm interventions that have proved successful in redirecting the resident.
If the resident is receiving routine visits from psych, either the psychiatrist, psychologist, or NP, there are usually lots of notes for each visit addressing the psych meds, nursing reports of behavior, discussions with family & education, & a recommendation following each visit to continue current TX & meds or to recommend changes, I am not as concerned about the meds they currently on. If there is no psychiatric specialist following a resident with serious psych issues, I start looking for the reason why. I look to see if the resident been stable for a long period of time and if not, if behavioral changes are being noted, addressed, and if they are making a difference. I look for outcome of care.
Resdient's on antipsychotics without a MH dx and who do not display any behaviors, aggression, or escalate to a point they are dangering themselves or others is a huge red flag for me. Regardless of the diagnoses the facility can get the MD to make up, I want to see evidence that the disturbing behaviors still exist or want to know why a GDR has not been tried. Any demented res on antipsychotics is a red flag and antipsychotic use needs to be questioned.
Multiple use of antipsychotics on one person. Resident appears sedated. Physician refused to try GDR without explanation. Staff report that a resident used to be more active and animated and medication has changed them. New illness related to lack of activity – developement of respiratory illness or urinary tract infection or pressure area or failure to thrive. Sometimes the pharmacy consultant will say that the doctor is adamant in keeping resident on heavy doses of antipsychotics. Sometimes the medication used is old and newer more effective medications may be more effective but the doctor did not consider a change or reduction.
In relation to anti-psychotic drug use, have not cited at this time, but have been surveyor about six months. But if see a breakdown in the system, such as failure to notify families/attaining consents, staff not monitoring or notifying physician of related issues, such as increased falls, weight loss, or behavioral changes when medication started, or if see a common factor such as many prescribed same medication, high level of residents on anti-psychotics without supporting documentation.
If resident's receive antipsychotic medications without an indication for use. No documentation to support the use of the medication. Observations of the resident over-sedated and not having quality of life. Staff unable to explain the need for the medication. The affect of the medication on the resident and continuing the medication without dosage reduction attempts.
The primary determination that would indicate a deficient practice would be if the resident is experiencing negative outcomes related to the facility not using the medication appropriately, such as the resident sleeping all the time related to an antianxiety medication for which there is no indication for use, or a resident experiencing loose stools who is also on several medications to alleviate constipation without the medications being held. Also, if the facility had a resident on a medication and did not monitor for side effects (such as toxic medication levels, suicidal thoughts, increased blood sugars, tardive dysknesia, etc.). Also I would look for gradual dose reductions for medications unless clinically contraindicated.
A number of additional, unique Surveyor responses may be valuable to incorporate into a protocol/checklist:
No communication between facility, pharmicist, and or doctor. Lack of effort to reduce the number of medications, duplicate therapy, over use of medications and the biggy if the resident has suffered ill effects..
I think for me – I need to see a clear indication of the use of an antipsychotic use – just because the resident has dementia w/aggression is not enough:
I really need to understand everything the facility did prior to introducing the antipsychotic –
If I don't have that – then I cite
Did the nurses follow up on a pharmacy recommendation to titrate antipsyc medications down, byu contacting the physician?
Did the Care plan reflect reflect changes, continuation of the psyc meds?
The main elements are the resident response and outcome to the medication and the facility monitoring of the effectiveness of the medication. If the resident has been impacted negatively – being snowed, losing weight, a change in demeanor that is not natural for the resident we would consider the facility's compliance with this requirement.
Is the resident benefiting positively from use of the medication and has everything else been eliminated as possible solution to the residents issue. Has the risk/benefit been clearly discussed, explained and examined with the resident or POA AND is there documentation of this.
Staff providing nonmedicinal interventions prior to the administration of a psych med.
No diagnosis/indication for the usage of a psych. med.
The key is whether or not the resident really needs the medication.
Excessive use of PRN's on a daily basis and corresponding inaccurate behavior modification records not necessitating use of antipsychotic medicatiopns.
GDR are very important because studys show that after a period of time in most cases antipsychotics no longer have the desired outcome
excessive side effects, lack of gradual dose reduction and administration for staff convenience. All are potentially harmful to the resident and decrease their quality of life.
Lack of GDR in the absence of symptoms or lack of improvement in symptoms – because I have found that behaviors for both dementia and mental illness can be transient and don't require consistent dosage and or / use of anti psychotics or drugs used for dementia and if targeted behaviors for use don't improve the resident is receiving an ineffective drug for no reason.
Use of two medications in the same classification unless there is a clear indication for use and no contraindications
is resident having a negative impact
is the facility aware of it
does the facility have a system in place to address
Yes, I look to see if non-pharmacological interventions have been attempted first and if not I cite. I look to see if there is a clinical rationale to continue the medication and if not I cite. Social Worker, 5-10 years, Traditional, TX.
Were other intewrventions tried before antipsychotic medications
Medical causes ruled out
lack of care planning for behavior with consistent behavioral interventions before use of AP, drugs used for staff convenience due to lack of adequate staffing
Does the resident have a legitimate supporting diagnosis and does the use of the medication maintain or improve the resident's functional status and/or psychosocial well being.
Gradual dose reduction attempts are key because there are very clear and concise requirements. Target behavior monitoring provides the justification and evaluation of the effectiveness of the medication.
GDR because a gradual dose reduction (GDR) needs to be completed at least two (2) times within the first year, and then yearly after that.
If the pharmacist makes a recommendation, and the facility didn't follow up by notifying the physician, especially if a resident continues to receive a medication that the pharmacist recommends to discontinue.
For me personally I look to see if the staff tried a non-pharm interventions first and I look for the frequency if the med is a prn and if the med seems to be given by the same nurse same shift, i.e. a pattern. I also look for justification of the usage.
When residents suffer side affects from a psy medicaitons and the facility has not tried to reduce the medicaiton.. Means they are not looking at the resident's needs.
When medication is used as a restraint. This is a quality of life issues. We have found facility's who keep residents sedated instead of dealing with their individual needs and behaviors. Whey need to determine why the resident is having the behavior not just make them sleep all the time.
When physician refusses all recommendations made by the parmacist.. We see power play instead of look at the resident's needs. Should be about the resident not who is in charge of the residet's care.
Over medicated, falls with medications
I try to use the Investigative Protocol to help me make that determination. If I observed a sedated resident and none of the criteria (indicication for use, monitoring etc.) is not being done and the interviews do not go well, then it gets cited.
whether or not facility is monitoring behaviors is the major reason we cite. The thought is that if there is no behavior or evidence of monitoring, then there is no documented evidence the drug is needed. We also cite if there are no docuemnted attempts at non-pharmacologic interventions, or if the facility is documenting but they consistently docuemnt no behaviors without a dose reduction.
If medical causes are ruled out was there staff intervention to find out the cause of the behavior
Did any staff consult the family or caregivers regarding prior behaviors/
Only cited once due to resident receiving prn antipsychotic medication for behaviors when the resident was in pain.
In citing F329, look to see if there is deficient practice and if the facility was or should have been aware of the situation. Refer to investigative protocol.
Failure of the MD/ pharmacist or psychiatrist to evaluate the resident's medications and responses – and to address GDRs if appropriate.
Failure of communication between the direct care staff and medical staff to ensure the resident is receiving the proper medications and care and any changes in condition were communicated.
If the facility staff failed to consistently identify the resident's behaviors and to comprehensively assess and reassess and track those behaviors.
The use of antipsychotics without indications for them or follow up notes. The use of prn injectable form.
multiple antipsychotic medications Always investigate for someone taking more than one behavior medication or taking multiple times per day
The ordered drug and did drug assist intended favorable outcome for resident? If a resident is given unnecessary medication that cause side effects like confusion, for example, a resident cannot live a life that is favorable. All drugs are potential poison if not used for treatment or benefit.
Two key elements when determining whether to cite F329 are where the facility determined the root cause analysis for the residents behavior and did they determine the level of risk for the resident?
These two key elements will help make the determination with the investigation involved.
Some Surveyors note that F329 enforcement is a challenge, that they have never cited F329, that “paper work” alone would not warrant a citation, that Surveyors receive little support, and that such a citation depends upon team consensus and outcomes:
As mentioned earlier… its hard for an F329 to go through our enforcement unless I can prove a care issue has resulted from a psychotropic medication… sometimes I can show potential with polypharmacy but this is sometimes difficult.
Haven't identified this citation before.
if there is only one or two instances of something that had no effect on the resident and involved paper work i useually would not cite it. if there was any effect on the resident then i would automatically cite the deficiency or if it effected the care being provided by staff then i would site it. also if it was something that involed more then one resident no matter how small i would also cite it.
If there are adverse reactions or side effects that are evident, or if the resident is in obvious distress and no evidence or little evidence is found the facility assessed to determine the need of medication.
ie: Constipation, frequently is the result of medicaiton use. Anxiety is often misinterpreted as aggitation, and the wrong medication/treatment is given. When a resident is very sedated or somnulent, I look at medicaitons. If there are no non-drug interventions in place, and medications are given without looking for ways to resolve the problem without drugs I look at drugs.
Without some outcome experienced by the resident, or an apparent risk of outcome, I do not cite F329.
The presence or absence of the psychiatrist following. The key is my time is too short to spend it writing a violation, if I am going to lose an IDR. Our region does not give the surveyors very much support or guidance, we are pretty much on our own.
Is it an unnecessary drug for that resident and why?
Team consensus for deficient practice.
If you dont have a good interview from the physicians you are out of luck
the resident has to be grossly sedate, increased falls etc and then it's hard to get it out of the office because without a physician saying the psyc med needed to be GDR, no citiation.
No, I try to cite with just one or two variables with no preference to what they are; but the barrier often times is the team or/field office supervisor who will not support a deficiency for one resident with only one variable/key element as my determining parameter.
Haven't cited F329 in ages
In response to several other questions in this Questionnaire, many Surveyors note that they cannot or do not question the authority of the physician. Question 13 also elicited this concern:
I cite F329 when I see no interventions attempted with a prn medication–or when no GDR is attempted, when the pharmacy has also recommended a GDR– but if the MD-the residnet's MD or the Psych Md says no GDR–but with no reasons, and I see no behavior or whatever for the use of the med–I can't site it because I can not question the authority of the MD. I think that few nurses asses for adverse reactions to meds, some of the symptoms include geriatric conditions–tremors, sleepiness, etc.
At least a dozen Surveyors respond that there are no few “key elements” to identify and instead point to the entire process:
No there is not one key elemnet it depends on findings on site.
No, I would cite if any of the requirements are not being met.
I would not say there are just one or two key elements involved. The entire process needs to be reviewed when it comes to antipsychotic medications.
Not really. I look at all of the information.
I don't know if there are one or two key elements. I try to look at it the entire picture, if they meet the regulation and the intent of the regulation. If they have tried other means to decrease the resident's meds i.e. activities, toileting, snacks, etc. Are they able to show me with documented efforts what they have done.
not just one or two its a whole system issue
That is an oversimplification, many factors have to be weighed.
No, there are not only one or two. You have to look at the overall picture of a resident to determnine wheteher or not there is an issue with 329
Surveyors indicate that staff convenience and chemical restraint are key elements in their decision to cite F329:
is there arm/the potential for
chemical restraint/unnecessary/staff convenience
If other surveyors have the same issue with, for example, residents' not engaged; receiving antipsychotic meds at the same time for he convenience of staff; inadequate documentation on behavioral sheets.
We look for outcomes when determining whether we cite or not. If the resident is exhibiting behaviors and their quality of life is being impacted, we delve into the situation more intensely. If we determine the facility isn't monitoring the behaviors, isn't monitoring the resident's response to the interventions used (both pharm and non-pharm), and if the staff isn't aware of/doesn't use the resident's POC to help the resident, we will cite this. We will cite this as well if/when it's apparent the use of the medication is for the benefit of the staff vs. the resident…
no evidence of psyche history /diagnoses. No behaviors that are harmful or have the potential to be harmful to resident self or others. Been on the same dose for long time and no evidence of trying to reduce dose. They are key b/c otherwise residents get medicated so they are behaviorially controlled. That leads to less direct care staff interactions and of course less calls to the physician.
Many Surveyors note that a system-wide problem would constitute a key in determining an F329 deficiency:
Yes, as stated above, if those elements show a pattern of poor practice then I site this
Potential for harm to the resident.
Is it a system wide problem?
Initailly no awareness by the facility that there is a problem is part of the determination then subsequently if there is no system in place to monitor the drug use or if pharmacy recommedations are ignored or no MD/PA involvement on the drugs necessity
Lack of system which would enable the Facility to determine if drug interventions are appropriate and working – such as behavior tracking and care planning.
care plan, behavior monitoring, oberservations of activity and interaction – do they know how to deal with dementia without drugs
Determining if this is an isolated situation or multiple happenings noted. Has this affected the resident' quality of life? Has the physician properly responded to pharmacy recomendations? Has the pharmacy review indicated that a timely reduction be attempted?
Scope/severity – interested more in a systematic failure vs. isolated failures that have no outcome to the resident.
Facility's knowledge of the regulation/requirements that is also supported by their policy's expectations.
if the facility has no policy to determine unnecessary drugs, no policy for GDR, residents who appear to be drugged.
Two Surveyors provide their perspective that fear of harassment or interference by the State Survey Agency are problematic:
Is there evidence to indicate that the facility allowed a resident to suffer because they were afraid to medicate a resident properly due to that the fear of harrassment by the State for using neccessary psych meds.
Through documentation and observation are there residents that appear oversedated.
Mostly that dose reduction has been considered and evaluated. For some people, they have taken years in the community to find a correct theraputic dose far before NH placement. If it works and is proven with prior failure for reduction–we should not mess with that.
Question 14: Are there any other elements of primary import?
Two hundred forty-six (246) Surveyors responded to this Question, which was designed to allow Surveyors to supplement their responses to Question 13, if they felt constricted by that question asking for only one or two key elements that determine whether they cite F329. Surveyors primarily identify the same key elements they detail in response to Question 13, but note some unique elements and revealing approaches:
A radical change in a resident's behavior such a violence or attempted suicide or elopment with injury or severe weight loss due to lack of appetite.
Always consider any complaints and if they relate to antipsychotic use
Are the medications being used as a staff convenience.
As needed medications are not used as a chemical restraint during times of decreased staffing or during select time periods.
Assessing the combined side effects of the medications, usually residents are on antidepressants, antipsychotics, and other meds affecting blood pressure and balance issues that can lead to falls.
beers listed medications
Check to see if the staff have had the training needed to take care of residents who are on psychotropic meds. How to handle resident's with different behaviors and the different activities that residents with dementia require.
Communication is key and acting upon that communication.
Continual education of facilities and physicians as to the importance of using medications only when truly warranted and looking at the resident as a whole person with individual needs.
Conversations with nursing staff and family members as to the mental condition of the resident and the quality of life they are currently experiencing,
During observations are the residents content or distressed. Are they worried, afraid. Observation is really iiportant and it need to be done both in the day time and in the evenings. and sometimes during the night depending on the resident. Why it is important to talk to care givers of different shifts. Residents with demential act differently at different times of the day. .
Evidence of a facility's overall lack of assessment of residents receiving antipsychotic medications.
Facilities don't really get how dangerous these meds can be for older residents. A lot seem to use these meds as a way to slow down or control behaviors that otherwise could be managed by other less restrictive means.
How committed the facility is in reducing the number of medications given and their commitment to alternative therapies is very important.
I do feel having a discussion around side effects/ risk and benefits – but I don't know if I really do a great job and determining if the facility is monitoring for those side effects….I know for some of my teammates it is very important to have medication side effects on the MARs…
I have no psych background and I see in the literature that drugs such as Aricept and Namenda have no long term benefit yet we see residents on these drugs for extended periods. They are expensive. I do not know how to evaluate their effectiveness. I do not see the resident on a daily basis so I don't get a full perspective of them. Can these drugs be used on a limited basis and if no improvement be discontinued? My psych experience is nada. So a physician can hand me what appears to be a credible reason and I do not believe I would know any better. I realize I have my team to consult with.
I think the surveyor staffing is important. The more surveyors on a team, the more time we have to spend making observations, talking with families and reviewing the charts. It can be very challenging to complete the entire task in a timely manner, review documentation and make observations when you have a limited number of surveyors during a full health survey.
I'd just make a note that I have concerns that we're asking facilities to take a lot of time and effort to document and justify the appropriate treatment of residents with diagnoses of schizophrenia, bipolar disorder etc. when the real issue (from my point of view) is identifying the facilities/physicians who utilize antipsychotic medications as a front line intervention for behaviors associated with dementia. It doesn't make sense to me to ask physicians to justify, even on a yearly basis, why a GDR isn't being done for residents with long standing histories of schizophrenia, bipolar disorder, depression, etc.
If the facility has all the i's doted and t's crossed (monitoring, diagnoses, evidence at lowest effective dose, consent forms etc) and the resident is engaged in meaningful activity during the day I will accept the use of the antipsycotic med.
If the Resident is hard core psychiatric. Are they living a better quality of life for a short period of time or a miserable quality of life for a longer time. Some do not do well with dose reductions.
Is there a pharmacy service system breakdown. Is the Pharmacist recognizing deficient practices? Is the NP too free in writing orders for meds? Is the MD responding to pharmacy recommendations and justifing disagreements? Are R/Ps consentng and/or being consulted? Is the use of meds care planned? Response of DON to Pharmacy reports? Medication Pass.
It seems that in State J with the closing of the mental hospitals there is an increase in the population of antipschotic drug use as there residnets had been on these drugs for many years. It is reveiwed if the facility has had any of these admissions.
Lethagic residents, and going in at HS to see if the night staff is medicating for their benefit. After a staff members says something like Mr. so and so gets___ at night if not he will be up all night bothering us.
look at the resident, watch what they do. You can talk to dementia people and find out more then you think.
Mostly that dose reduction has been considered and evaluated. For some people, they have taken years in the community to find a correct theraputic dose far before NH placement. If it works and is proven with prior failure for reduction–we should not mess with that.
Multiple drugs are common- hard to prove why a resident should not be on 2 or 3 anti-psychotic or anti anxiety drugs, even when they are on 25 other drugs.
My own Mom had a seizure of unknown etiology. She was placed on Depakote, both for seizures and behavior. I believe she suffered from the drug's side effects. She then had a carotid endarterectomy and MRI showed a previous CVA. After moderate rehab with therapy services, she was acting kind of "goofy" and her gait was unstable for someone who had walked an average of two miles daily with her dogs. At a nursing home, she had a change in mental status and her lower extremities, both for unknown reasons. Her SNF MD sent her to a hospital and the neurologist dc'ed her Depakote. She never had a seizure after the first one, approximately one year previous to this. To our astonishment and pleasure, her affect became baseline and her gait improved greatly. I personally believe that she had suffered from side effects of Depakote after having read about edema in extremities and seeing her affect decline during the duration she was ordered Depakote.
not that I know. The questions below seem to be assuming we are chosing residents and not the computer.
Observation of the resident-are they sleeping all of the time, are they crying out, what is their history, have they been seen by a psychiatrist or psychologist, have they been care planned, are the staff aware and are providing the interventions, are staff knowlegeable, are there enough staff
One of the biggest issues is staff doesn't tend to identify the specific behaviors the residents may be exhibiting. Instead, they use generic descriptions, such as agitation, and their approaches to help alleviate the behaviors tend to be generic as well. We look for individualized plans of care…otherwise, the facility staff just treats every behavior the same and justify the need for medication…seems it's just easier to give a pill and less time consuming than to take the time to redirect a resident, distract them, etc.
resident interview, yesw some will tell you that do not recieve there meds corectly or at all.
RN, 5-10 years, Traditional, TX.
Residents with dementia who are on Geodon , Haldol or Risperdal.
That what is on paper is being implemented and that all staff are aware of the interventions.
Review facility's policy on Antipsychotic Drug Use.
Staffing of facility.
Staff interaction with residents. Staffing levels and training.
The individual resident response to the medication. Some residents may have behaviors that are detrimental to their health such as constant walking/pacing that may cause weight loss. The psychoactive medication may actually help them to slow down enough to eat. If titrated well and documented well then I don't cite the facility.
The use of psycocative medications and restraints has greatly dedcreased since 1994
We surveyors may want to cite and do cite with facility but when brought back to the regional office, the deficiency is dropped due to not sure…
Question 15: When you are conducting a survey related to F329, do you:
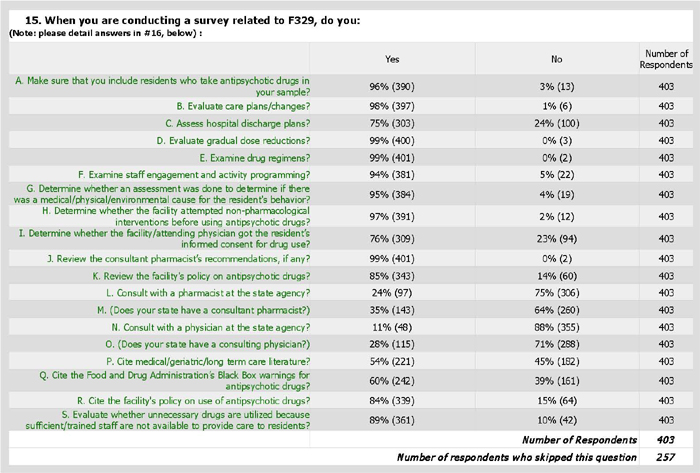
Question 16: Add any details or comments you have for the items from question #15, above:
Question 15 contains several subparts asking whether, when Surveyors are conducting a survey related to F329, they perform certain enumerated tasks. Question 16 allows Surveyors to elaborate on their yes/no responses to Question 15.
A) [Do you] Make sure that you include residents who take antipsychotic drugs in your sample?
Facilities often do not "offer" information on antipsychotic use, usually put residents in other catagories like "antidep" that why record review important.
not always done when conducting complaint investigations
Residents on Ritalan and Benedryl
try to when the facility can provide a list at entrance, sometimes they don't know themselves who is taking what
Yes but CMS needs to look at process in requiring four cases selected must be in Phase 1
almost always-sometimes depends on QM
also include drug interactions
presurvey selection determination does not always trigger antipsychotics
sometimes it is difficult to include due to short time available to survey
We always select four, but it's sometimes hard as the sample requires inclusion of a number of things (i.e. triggered care areas, residents who were present during the flu season, WPH's) and it's hard to include all those areas, especially in small facilties.
One of our team coordinators refuses to do this at survey
This is now a requirement that at least four residents are sampled in phase one of the survey process who are on anti-psychotic medicaitons in the last 30 days.
To this point have always had in sample and if note resident receiving IMs on stage 1 will add
try to-difficult if have to pick residents from off-site and this info not available when doing off-site.
B) [Do you] Evaluate care plans/changes?
Ensure care plans written and reviewed relating the use of an antipsychotic medication
Were the interventions utilized? Observations on all shifts when applicable. Did the care plan ever change?
Antipsych. meds, behavioral interventions need to be care planned.
Check to see that the care plan is followed and revised as necessary
Yes, for MDS or changes in resident's status and/or needs.
Written resident care plans are seldom useful. They consume excessive amounts of facility staff time and typically do not reflect all of the interventions actually provided during bedside care. For example, every resident is not issued a care plan regarding abuse prevention; however, general staff education is sufficient to ensure that staff are educated on how to provide care without being abusive. The same holds true for dementia. Staff education regarding dementia will be sufficient for staff who desire to administer care to the highest level possible. Twelve care plans will not improve staff performance at the bedside.
Care plans are always revewied for individuality and critical care points
Antipsych meds, behavioral intrerventions need to be care planned.
Very important part of the review.
Always expect to see care plan updated for behaviors or changes
Planned approaches need to be changed as the situation warrants.
Social Worker, Less than one year, Traditional, TX.
making sure they are individualized and followed
determine if care plan is generic or individualized
Do not feel as a team this is being addressed.
always look at CP/look at seeing if revised with appropriate interventions.
Care plans are to meet goals. They have been misinterpreted by CMS and surveyors.
C) [Do you] Assess hospital discharge plans?
usually don't tell you anything other the meds at time of d/c
– if provided by the facility // sometimes hospital records are readily avaible / other times not readily available
when newly admitted with meds like PRN Haldol
on occasion but not routinely.
never available
Yes to see if the drug was started at the hospital. Is it still necessary. Hospitals are know for giving the elderly Haldol when the resident is experiencing a change in condtion that may only be delirium. So the med is unnecessary.
these are usually vague and do not deal with psy meds but I take a look becasue it may deal with other aspects of that resident's care
Please provide rational for why this is an element I should be viewing.
No, unless it was an in-patient psychiatric stay where care is specifically driven by intervention responses. Routine hospitalizations provide little focus on psychiatric conditions; hospitals are driven by a medical model.
only in specific instances where facility indicates the importance
Depending on if the resident is a recent or new admission
Review for orders in the hospital that the Long Term Care Facility carries over.
when available especially from psych facility or crisis admission
Not surey what you mean. What does D/C plans have to do? Usually they just list the medications at discharge.
To see what changes were made when admitted/readmitted to the facility
to see if the resident has a long history with taking psychotropic medications, diagnoses etc.
We look at the hospital discharge, if there was a red flag I would compare and contrast the medications
Not relevant.
Yes. Hospital discharge plans give vital information.
not usually. Hospitals tend to start residents on psych meds who do not need to receive psych meds and who do not requre them once they return to the LTC facility. I look to see what actions the facility staff took once the resident returned on a psych drug.
Not really other than to see the orders sent to NH. Looking at current NH orders for resident
I review the discharge plans to determine what the recommendations from the hospital are.
Ususaqlly they are very basic and vague,
Only if the med was initiated in the hospital.
Only when the resient is recently admitted and the information is on hand.
D) [Do you] Evaluate gradual dose reductions?
Were they timely? Was there evidence that the pharmacist read the chart, talked to the staff, observed the resident? Social Worker,
Yes, especially when on meds for long periods of time
if in the time frame, If GDR's have been attempted and the resident has not tolerated them…do not always expect GDR to cause a relapse in the resident
Unless substantial amounts of time are spent in the clinical record (not recommended by all other SOM instructions), it is not always feasible to track the onset of a psychiatric symptom, psychotropic medication, last attempt at GDR, etc. I depend mostly on physician H&P/progress notes and the consultant pharmacist to pull most of this information.
difficult to due in such a short time
We check to see if they've been recommended and implemented, or if the doctor gave a reason not to.
that the facility has placed critical thought into the reduction
always review for pahrmacy recommendations and/or contraindication by the residents physician
Review frequency of reduction attempts related to facility policy
yes, however when this is brought up at team meetings the response is "if the psychiatrist documents medication outweights the risk" there is nothing that can be done.
As resident is acclimated to the facility, are attempts made to decrease medications.
none some facilities feel that a GDR can be accomplished trying only for one day or so
Always according to the regulatory guidelines there are times when families refuse a GDR and this is a fact that is important to consider.
Yes–you usually see this done before the full health survey–every faciloity knows about when their full health survey is due and they do a full house sweep of GDR
They may have attemped GDR over a year ago, it didn't work, and the notes have been removed from the clinical record.
E) [Do you] Examine drug regimens?
Were they accurate? matched the orders? given as directed? Behaviors, SE monitored?
Is there consistent Patterns for all residents
Always look at doses, duration and drug interactions, Necessary labs ordered
overview on all my sampled residents and then narrow in if I see a need
how many kinds of meds how many tims per day
Is there consistent patterns of meds used for all residents
to ensure the facility is following up on pharm recommendations.
We do this on every resident regardless of medication regime.
to ensure that there were no duplicate therapies and that diagnoses were there to support the medication use
Do not feel as a team this is being addressed.
Compare daily medications with PRN's.
seeing what the monthly DRR is recommending and if the MD is agreeing
for duplicate therapy
F) [Do you] Examine staff engagement and activity programming?
speak with activity staff , ask how they are working with residents for interventions versus drug therapy
If in special units
Were the care plan interventions practiced?
consider this part of person centered CP
Eval. whether they are good alternatives, age appropriate & meaningful to the residents
look for staff trained in dementia activities
See what activity program is designed for the indiviual resident. How resident reacts? What causes the behaviors is the resident bored and acts out?
Yes. Do they attend? Participate?
Yes but don't have the supprt from the remainder of the team to also examine activity programming which could lead to a F248
this is hard to do
what was tried first? did they look to see if it is triggerd by staff or certain daily activities
Yes, that's a major factor especially individualized activies.
This is key to determining if they really know this resident and behaviors and how to deal with them
to monitor if behaviors are present or different while engaged in an structured activity
During care observations, are staff picking up on things that may cause a resident to exhibit behaviors.
Really not enough time in just 3 days to do everything in these protocols.
Yes. Activities/staff interaction may be enough to deter or decrease behavioral issues.
can indicate other interventions and effectiveness, can let you know if satf are aware of the interventions detailed in the care plan
Typically when the resident had experience a negative outcome or the facility failed to follow through on drug dose reduction or failing to evalute other meaures prior to giving an antipsychotic.
For residents with behaviors I think it is essential to providing care, you never want to see a lack of activities or no activities at all.
I dont think what staff do for activities would be appropriate for F329.
Do not feel as a team this is being addressed.
Observations on the variuos shifts to evaluate staff care and services.
Concerns in this area are often dismissed by a TC
not really, who has time
Activity assessed throughout survey & closer for individual samples
yes, to see if the resident is kept stimulated and how the resident's behavior is during activities.
Yes but we neverr cite this–staff-cna sit with residents while they watch tv for hours–this is different from activity staff.
This is very difficult to do effeciently do to the amount of investigative protocol to complete.
I always observe the activity program to ensure residents are engaged in meaninful activities.
Are the medications due to a lack of staff engagement and available programming?
Residents gathered in front of tv sleeping left up by nurses station etc.
If necessary if this is nonpharm approach
G) [Do you] Determine whether an assessment was done to determine if there was a medical/physical/environmental cause for the resident’s behavior?
not ususally
interview staff about what behaviors necesitated the drug. what was going on?
Yes should be done b4 implementation & admin psych meds
look for diagnostic testing to rule out metabolic cause, make observations of nursing unit for undo stressors of noise, light, activity, crowding, need for care
I haven't always seen this in a formal written assessment
Really important but too often not done or not done well.
I don't recall ever seeing these type of assessments occasionally a note from the nurse or physician but not a thorough assessment to determine cause of resident's behavior.
The term, "assessment," can be many things from something as simple as a T-P-R/BP assessment to a physician's physical and obtaining labs. Who defines how extensive an, "assessment," should be before it is considered an, "assessment?"
This is rarely found
Woudl ask if new behaviors are tracked somehow and what conclusions are drawn from them RN, 5-10 years, QIS, OR.
difficult to due in such a short time
is the residents exhibiting behaviors at a certian time of day, around certian people, after certian medications are administered or during a certian activity of lack of an activity
Yes, this is a important piece. Look to see if the staff know the resident and what can lead to escalation of behaviors.
necessary to find the antecedent to one's behavior….could be pain, not feeling well, or tasks that were not adjusted to the residents routine and not that of the facility staff
Clinical record review includes assessment of causative factors.
Review behavir monitoring sheets why resident is behaving in cetain way
Look at labs, UA's, behavior monitoring to see if they could explain behaviors
this may take work to find
Do not feel as a team this is being addressed.
Usually the medications have been in place for some time before survey review or the resident's admission so this information may not be available.
yes, it's important to know the resident's history and if the IDC team has evaluated the previous behaviors and determined that the drug may be due for a GDR or no longer necessary at all.
Facilities have routine assessments and assessments that are completed if there is a signifcant change in residens conditions. We ensure that this is completed to determine the residents next level of care and ensure that needs are met.
No assessments are done to determine this–the Md says impression/plan but its his thought process that he has been doing for years–its demementia thats it.
This is done more when behavior health IDT members are involved in the care.
many physicians do not appreciate surveyors questioning diagnoses or drug orders
not all facilities do an assessment
if the resident has been on the drug for a very long time this evidence usually goes beyond previous survey and often is weak. Not effective use of time.
H) [Do you] Determine whether the facility attempted non-pharmacological interventions before using antipsychotic drugs?
try to but limited documentation. Half to trust what staff say as true. talk to the aidn not adminstration
Normally both nursing staff and MD do not consider alternatives/interventions
Interviews tell the story. Surveyors should be skilled interviewers. Look at documentation
was the resident on the drugs prior to admission? behaviors at home?
yes, especially activities and pain assessments
Did not address this earlier but we do check this and also interview on how staff handle specific situations to see if they do antipsychotic drugs at the last resort.
such as milk and a sandwich at midnight for insomnia
Definitely, this should be clearly documented and included in the resident's care plan.
Many times the behavior can not be controlled except with medications.
Look for these interventions with each behavior episode
this may take work to find
Do not feel as a team this is being addressed.
Resident's have most often been on the medicaitons long term before the survey review. Can be reviewed for new medications.
Every facility does this differently which makes it difficult to determine at times. Sometimes it is documented on an E_MAR or on behavior monitoring sheets or in the nurses notes.. Often the documentiaton does not always coincide with the administration of the medication.
facilities often only attempt non-pharmacological interventions prior to prn meds, they will change orders to straight to avoid this requirement
The facility's behavior sheets are not clear and the numbers don't always match or are written in..
I) [Do you] Determine whether the facility/attending physician got the resident’s informed consent for drug use?
how do you informed consent from a dementia resident?
I don't believe I've used this for determining a unneccesary drug
Yes. most of time responsible party are not fully informed on drug side effects in a manner that they fully unsderstand.
Usually only if comes as a complaint
Should be consider but not a driving force
This is usually from the families. We have some issues with families wanting the meds and the MD ordering the drug based on the family request, which we cite if there is no other justification.
Most of the time I remember to do this. On occasion I forget.
most consents are obtained by nursing! point of discussion who should get consent?
Have not done this. I think that I need more info regarding what I should be looking at for the informed consent.
I have never seen this; not sure in regulation where this would be…
Usually not done by the physician…mostly by the nursing staff, if documented at all
somehow I have never thought of this
Never
usually not done in our area and question whether necessary
not routinely
routine practice
Well this should be considered, it may not be the driving force b4 implemtation especially if the residents behaviors, conditions place them or others possibly in harms way and alternativres are not effective
I have not doen that one before. Is this a new directive?
Yes. Since the medication might be a chemical restraint.
Have not been reviewing.
This is generally documented in the chart, but it is not the first thiing I look for, as all treatment is done with the consent of the resident… It is a resident right.
Never thought I had too.
This would be hard to do. Is it required?
is this in the regulation?
Not usually as many couldn't give consent. Also, many resident's don't have anyone who can legally give consent.
residents receiving these medications are often unable to understand/consent
Only if started in facility
J) [Do you] Review the consultant pharmacist’s recommendations, if any?
always review the pharmacist's recommendation , ask for an explanation if there is no documentation that the attending physician has addressed .acted upon the pharmacist's recommendation
Are they consistant? Follow guidelines? Acknowledged by the MD? Does nursing follow up timely?
make sure it is done monthly. does the physician get their recommendation? is it well received?
should be consistenly done. Recommendations should b checked that they were reviewed
drug interactions? reduction? ask MD?
to see if he has picked up on any issues not addressed
Should be consistently done by surveyors & especially the physicians response to clinical recommendations, etc
did the facility follow or document why recommendation was not followed
Look at this to determine if the pharmacists are doing these and are they reflective of the regulations.
If doing the pharmacy review or if a concern for an individual resident
to ensure that the pharmacy is following the regulation with recommendations for gradual dose reductions and/or monitoring all medications
Some pharmacists are not aware of CMS regulations, some do not write legible notes.
Yes but if the physician disagrees every time what else can be done?
IF THESE RECOMMENDATIONS ARE NOT FOLLOWED, THEN I WILL PROCEED TO INTERVIEW THE DON, PHARMACIST, AND POSSIBLY THE MEDICAL DIRECTOR
the consultant usually keeps track of the length of time a psych drug has been in place and often suggests it is time for a GDR. We then look to see the physician's response of the follo-up from the nsg staff.
important-reviewing the recommendations to see if the MD agees with the pharmacist or not
I do review these–many times you will see the consultant word his rcommendation based on F329 and most of the MDs wilol listen and do GDR.
K) [Do you] Review the facility’s policy on antipsychotic drugs?
if they have one. most places have general policies that are not informative.
have never done this, I might start asking for it..
If a deficiency is cited
If there is a negative finding then this is reviewed.
yes, though policy not needed to cite F329
yes but tags cannot be written on P=P– just for not following it
always; citing alternative interventions to drugs
to see that they promote compliance with the regulations
Important to identify if the facility is aware of the regulations and if the medical director had involvement in development of the facility policies and to confirm if the facility is following their policy.
only if outcome to a resident, and needed for the SOD
If a deficiency is found, might request their policy
Will start doing this. I don't think many will have a recent policy
Yes, to see if it appropriately addressess the need for antipsychotic drug usuage.
This is not always useful unless there is a widespread problem
never thought of this
If I find a problem with the residents drug regimine I would look at their policy. but I would never cite the tag soley based on their policy. The facility has to not meet the regulation.
yes ad if staff are aware and what is their understanding of it and involvement
this is necessary to see that the facility has an appropriate procedure in place to reduce the number of psych drugs and to see what the staff's responsibilities are in reducing psych drugs
Not all facilities have policies regarding the use of these medications.
Many places do not have a policy on this so we can not use it against them.
L) [Do you] Consult with a pharmacist at the state agency?
our region has a Pharmacist – we are lucky to be able to consult with our co-worker
Our State Phamacist is a great resouce.
not sure if we have one and NO idea how to contact one
we have 3 pharmacits that work on 3 teams. They are availible to help us but it is not usual practice to calll them on everything
don't have one and wish we did!!!!!
if we had one i would do that
Yes, I did not mention this above, but I have done this often. They are a very valuable resource.
I have never interviewed a pharmacist.
I have done this once or twice. It usually has been at the request of a manager who did not understand medication use, or when and how to cite F329. Managers are somewhat hesitant to cite this tag, because of a lack of knowledge.
Wish we had one.
Have called facility pharmacy for info
I don't think we are allowed
I'm not sure we have one. Never been informed of one.
rarely. We usually consult with the pharmacy who provides the medicines
this would be so helpful to have
Not aware if this is a resource available to us
We do not have state pharmacist but do interview pharmacist who supplies medications for resident.
M) (Does your state have a consultant pharmacist?)
Only 35% of the 401 Surveyors answering this question indicate that their state has a consultant pharmacist. Over 40 Surveyors (approximately 10%) were unsure, or did not know, whether their state has a consultant pharmacist. Several Surveyors commented that they would benefit from the opportunity to engage a consultant pharmacist. Some noted they consulted with the facility’s pharmacist:
would love to have one though
I've never been told we have a consultant pharmacist. I call the pharmacist the facility utilzies.
Yes, but I have never consulted with him during a survey, only afterwards at management's request.
Our region does not and phrmacists are a wonderful assesst to the survey team and they can perform the best review of the drug regimen and they are an awesome resourcs for the team during survey.
N) [Do you] Consult with a physician at the state agency?
don't know we have on that know about ap meds in long term care
A physiican is available, but the turnaround is not timely to actually use it for a def.
not sure if mean our state has a physician to consult here. [E] doesn't have one and wish we did.
Never have…I call the resident' MD or psychiatrist.
Would be great to have availble
State survey agency does not have and can not afford to have a doctor employed.
I have interviewed the attending physician
Wish we had one.
no physician would work for this pay
only if concern that is rising to level of harm or IJ
I don't think we are allowed or encouraged
Don't believe [C] has one – would be nice
rarely. Generally, the resident's physician is contacted.
Maybe this would be necessar at some point…but not usually
O) (Does your state have a consulting physician?).
Only 28% of the 401 Surveyors answering this question indicate that their state has a consulting physician. More than 50 Surveyors are unsure, or do not know, whether their state has a consulting physician. Several Surveyors comment that they would benefit from the opportunity to engage a physician. Some comment they could visit with the medical director.
no but could talk to the attending of the medical director at facility.
not sure if we have one and NO idea how to contact one
I believe that we do however am unaware of who and how to get this person involved
don't think we need one
In [E] who can we call if we have questions?
This would be very helpful and may put more accountability onto the homes' medical directors.
P) [Do you] Cite medical/geriatric/long term care literature?
don't have time to research this. duringor after a survey
It is important to be abreast of new information and to seek expert opinions and studies.
Worried about what source to use
This is used occassionally if the facility has no clear policies themselves.
if needed— do not want to muddy it. may cite literature if 281 is cited
Especially review of new medications not previoulsy perscived to the Resident
typically don't cite this information
the manufacturers specifications used most often. doesn't help to cite the latest from The Lancet for a 25 beds rural LTC
no access to literature that is sanctioned by central office for the state
instructed not to cite literature
Unless the facility has adopted the literature in to their policies.
Biers list? Geriatric medication handbook?
refer to but not cite except for standards of nursing practices
to ensure the deficiency is supported by medical information
At times will use as a reference.
so long as literature is current and comes from an approved source
As directed by my state, I use the Drug Handbook used by the facility, as well as pharmacy recommendations and the guidance/tables in F329
Yes review drug guides and look up info on the internet
Did not know this was an option?
I refer to other sources mainly for Standards of Practice.
Only if it pertains to what I am citing and it will help my deficiency. I try to take literature from the facility first.
it is hard to know what is acceptable.
As needed or as supplied by the facility.
yes if nessesary certainly manufacturers recomm.
I'm not sure where or what this would be.
only CMS approved literature
Usually a more direct route to the citation
Not unless absolutely have to as some literature/opinion contradicts the other. It is either a regulatory violation or not! May times this muddles up the deficency statement and the public doesn't get a clear picture of what is wrong.
Ned some books and literature so I can site them
do you mean cite as write a deficiency or use this as a reference?
not usually but possible if dosage exceeds maximum daily recommendation
Q) [Do you] Cite the Food and Drug Administration’s Black Box warnings for antipsychotic drugs?
I have not yet cited the FDA's Black Box warning – it is a good idead
Didn't know this existed??? Use PDR
Very wise to be aware
a fine idea, wish I had thought of it
Occassionally used if the facility has no clear policies themselves.
Have used BEERS but it has been known to be challenged. Use less.
If the medication it detrimental to resident will cite black box warning.
I look at this but not suffiicient to determine a citation even med error since going on this culture change with medications.
instructed not to cite literature
Not sure what this referrs to
no but would like to
Not generally considered in determining a citation.
I have used these in citations frequently.
doctors can order off label use without recourse
to strengthen the deficient practice…and if there was outcome
Did not know this was an option?
Some physicians are resistant to the Black Box warnings. Nursing staff frequently do not know of the Black Box Warnings. But I do cite it .
Do not feel as a team this is being addressed.
I do not know the process to do this
I do not think we are allowed or encouraged–if the Md orders it, its fine
yes if strong enough to add to the cite
This may be done, I am just not aware if it has been done in the past/it may get added to my SOD prior to being sent to the home.
R) [Do you] Cite the facility’s policy on the use of antipsychotic drugs?
Do they follow their own policies and does their policy follow regulatory guidelines?
if their policy does not reflect what they are doing
yes, if the problem is identified with more than isolated scope.
I haven't asked for this before
not strong enough must have outcome but will make a concern for them to review and change
We do not cite to facility policy.
Policy is reviewed if there is a deficient practice to determine scope – if the identified concern has been codified into policy that would support a widespread scope
Did they follow their own policy on when to assess and level of medication and notifications
policy would only be added to the F-tag
we are not permitted to cite on policy
Reference on occasion but not cite for failing to follow. Cite what they failed to do in reltionship to the regulation
I only review and cite their policy if there are findings and if their policy is not appropriate or not followed.
If there is clearly a deficiency and it is also against their stated policy I would include it in the citation.
no can not cite per facility policy only for actual regulations
yes need to have the facility's staff trained and follow the policy
Only if there is no outcome from the deficient practice and don't have a strong citation at F329. Then I cite to the policy not being followed.
No. It doesnt matter what the facility's policy says, if they dont meet the regulation, they get cited.
Policies are usually Ok- it is harder to implement the care.
if not cear, if staff are unaware, if a def. resulted from same
haven't, but good idea
I usually find the policy is appropriate but the staff do not follow the policy
I have cited facility policy before but never on antipsychotic medication for F-329
We are told we can not write def. just on policies-and alot of places do not have them so they are not held to them.
Usually, I would not just write a deficiency based on the policy soley, but it may be a part of a deficiency.
if their policy is specific enough and relates to the care resident is receiving, some policies are very generic
S) [Do you] Evaluate whether unnecessary drugs are utilized because sufficient/trained staff are not available to provide care to residents?
this is why we are there is it not?
In specialty units this is done
Not usually.
Interviews and observations should tell the tale here. Record review is not always reliable
think about it but hard to prove
harder of cite and would have to say cannot remember last time done
tough to do but needs considered
Difficult to assess; how can we expect the facility to provide 1:1 with a resident exhibiting behaviors?
This would be done if more of a widespread issue or a pattern involiving a number of people and the first instinct from observations is that there are not many staff around.
we rarely write staffing because we can't PROVE a negative outcome, we get bashed by our own administrative staff
we see this a lot but do not have standards whether fed or state to cite staffing. This is probably a big reason for many problems in our SNFs and we feel hands are tied.
I do not write that specfically in the deficiency but rather what I saw and what stff, residents and family told me
No we don't pull staffing sheets to determine a correlation but simply reference to facility that the time of administration shows a pattern of useage
usually only regarding activities staffing
yes to support any over use or lack of proper supportive evidence for use
difficult to prove.
Yes. Observe staffing patterns, resident behaviors and interaction of staff with residents.
have not but would like to. L
Difficult to do, but attempt to. we do consistently evaluate staffing ratios but cross comparision is difficult
are antipsychotic meds being used for staff convienence due to inadequate amount of staff or staff who are not trained to monitor for effectivness and side effects
This is a very important focus and part of the survey process for all residents.
There really is not sufficient time, and the evidence to prove insufficient staffing leading to drug overuse would be very difficult to prove.
Yes. If there is not enough staff to assess the causative factors and/or provide therapueti non-pharcological interventions antipyschotic medications will be reverted to.
staffing is always reviewed, this often is discovered in interviews with residents of families and in group
Calculate facility staffing to determine if related.
It will be very apparent if staff are insufficient or untrained… or just not providing care up to Standards of Practice.
this takes work but is essential
One of the hardest things to cite. More staff are there when we are and are afraid to say anything negative.
we often cite staffing when not sufficient to care for all res. needs.
haven't had to make that connection
Observation for sedation of residents and attempts of staff to re-direct residents with behaviors.
I do not fiind this to be the case. I generally find lack of thorough monitoring and failure of the facility to follow the regulation
I have never found antipsychotic medication to be used due to untrained/sufficient staff
I know this is true–but how do you prove it.
These seems it would be very hard to prove deficiency and take a long time to investigate…we are facing long intervals
This would be hard to prove, they may have adequate staff, but not really trained to provide alternative methods to work with residents with dementia, medication may be the front line they have used in the past and continue to take the easy way of over medication
95% of the facilities do not have enough CNA's (which means they do not have the time) to carry out all the assessments, observations required by the new dementia initiatives.
Is there ever enough staff?
I know this occurs, but do not know that it can be proven when the facilities meet the required nursing hours
I feel that some of these issues may be there but difficult to prove.
Staff convience.
Question 17: Are there survey tasks that you are required to perform that you believe are less important, or unnecessary, or that otherwise lessen your ability to fully investigate possible F329 deficiencies? What are those tasks, and why do you think they are less important/unnecessary?
Four hundred one (401) Surveyors responded to Question 17, which was designed to determine whether Surveyors believe certain survey tasks are less important, or unnecessary, or lessen their ability to fully investigate F329 deficiencies. Question 17 also asked Surveyors to identify these tasks, if any, and to explain their views about the comparative importance and need for these tasks.
More than 80 Surveyors indicate that they do not believe certain tasks fall into the “less important” or “unnecessary” category or lessened their ability to fully investigate F329 deficiencies. Many of these Surveyors simply answer “No” to the question, while others qualify their answers, offering responses such as “None that I can think of” or “Not in complaints” or “No, it is just a busy process all together.” One example is illustrative:
After surveying for so many years, I do not see any of the areas less important than the other. When it comes to F329, all the other areas reviewed can impact F329.
Similar to most, if not all, of the Surveyors’ answers to several questions in the Questionnaire, Surveyors respond to Question 17 with many common themes, a significant number of nearly identical answers, and an abundance of unique perspectives. In no particular order, the common themes and answers are:
a) Group interview (at least nineteen Surveyors)
Group interview often does not yield information that leads to identifying deficient practices, takes up time, residents often bring up individual concerns, (although often valid and not to be easily dismissed) and have to be re-focused on making a group consensus. Abuse and Title 6 intervies (state requirement) take time and do not usually yield information that leads to a deficiency.
Group meeting is usually a waste of time. More information is obtained from 1:1 meetings with individual resident, and their families. Sometimes the Group meeting turns into a bully pulpit for one or two residents who attempt to outdo each other, without regard for other resident's input.
The Group Meeting seems unnecessary when residents are already interviewed routinely. The abuse and QA questionnaires which are done every survey seem unnecessary unless an issue is found during the course of the survey.
b) Demand billing,
c) Quality Assurance
QA – if there appears to be a problem with QA related to a deficiency, then you can look into QA. If there is no QA issues related to a problem, then wasting time doing the interviews.
d) Environment (tour)/Life Safety
i. Boiler/Boiler room,
ii. Dumpster/waste disposal,
iii. Generator,
iv. Maintenance areas,
v. 803
Yes, I would like LSC to complete the General Observation Task since they are already looking at some of the things for the task and that would free up survey time to look at more resident care issues.
e) Closed record review,
f) Title VI Civil Rights Survey,
g) Review of disaster plan,
h) In-service,
j) Abuse/neglect protocol/tasks, (Task 5G)
I think task 5 G has become a redundant task… if we are suspecting abuse or neglect then the task should be done…but all interviews are clone remarks now… seldom cited…
Group interview seems useless but has nothing to do with F 329 really. All the interviews for Abuse/Neglect protocols with front line supervisors and direct care staff load survey down with sheets of interviews that we don't do anything with. It takes up too much time for survey. This is not relating to F 329 though.
k) MDS review/generated tasks (Vision, Rehab, ADLs, Urinary Incontinence)/weight
Yes, most definitely! The MDS review would be the foremost. This task is more useful in introducing the resident in an SOD. The specific information needed for F329 would be better found in the POS, MAR or other daily used documents and observations.
Following up changes on MDS between admission and 30 day the resident has not been there long enough on admission for good comparison.
Wasting time data entry with weights. Can look at weights and see if losing or not if not no need to document If they are losing weights then document
l) “General” interviews,
m) Resident funds,
n) Surety bond,
o) Meal and activity observations
I feel the group interview takes alot of time and usually doen't yield that much critiical information. This could be obtained by reading the Council minutes and perhaps speaking only with the President of the Council. I see know need to observe two meals on residents who eat independently and have no utritional concerns.
p) Corrective lenses investigations,
q) Observation of two meals during the survey,
r) Too many unnecessary med reviews, and too time consuming in relation to other areas,
s) Fire drill records, records on flu and pneumonia,
t) Typing in complete drug regiments,
u) Resident and family interview form
The resident interview form and the family interview form. A lot of times those questions are addressed during the survey, but a separate form is time consuming.
Many Surveyors are critical of the QIS process (not just in response to this Question, but others as well), variously commenting that it impedes the investigative process:
Some tasks are triggered when there is no issue and are just general time wasters, albeit quick to investigate.
Every QIS survey is different as to what will trigger for investigation. Some of these triggered areas, such as 1/4 siderails as potential restraints for cognitively-impaired residents usually turn out not to be restraints, and you have to keep picking another resident that triggered for restraints until you find a true restraint device. There are several areas that trigger from MDS in a QIS survey that often seem unnecessary. For instance, Vision often triggers for residents that are inappropriate for review; Lack of Rehab Progress and or Increase in Behaviors often trigger and have a very small window of time (i.e., how can you expect transfer rehab progress to improve in a 5-day period).
There are many parts of the QIS survey which I feel are just time consuming and impeed the investigation of not just F329, but other Care Areas as well (i.e 30 Admission Records)
Too many interviews to be done and too many questions about dental and other areas that tend to be repetitive.
The admission sample seems to be just an exercise in gathering information for statistics and there is little evaluation by the surveyors based on the answers. Some of these resident's should be reviewed more closely.
I personally find the QIS process restrictive. I know that during Stage I investigation if a resident responds to the abuse questions ,then the abuse prohibition is triggered. You can spend time in Stage II investigating this only to find that this incident had been reported and investigated already. That is only 1 example but as stated previously I normally conduct complaint surveys.
The majority of the tasks in stage 1 of the QIS process. We are forced to focus on only collecting and entering the data for the first two days of the survey. The majority of the time this does not yield productive information in regard to identifying actual deficiencies. Or it triggers items that could have been investigated and dismissed in a matter of minutes if allowed to investigate in stage 1.
Having to attempt to interview all of the resident's in the census sample is very time consuming and rarely yields productive information.
The resident interviews and observations in stage 1 are redundant and very time consuming.
Only mandatory tasks in QIS are Liability which I understand will not be removed
Res counsil interview which are not too helpful usually
Medication Pass, infection control and Kitchen Which are important.
What is not helpful are the Stage 1 questions and Skilled residents, they end- up triggering care areas that lead us down a rabbit hole ALL THE TIME and takes away from the important investigations.
For 329 we are required to write down all of the resident's medications. Most of the medications are not antipsychotics. If our focus is antipsychotics why the other medications? I have only had two drugs that were not antipsychotics that I cited a facility for the use of. One was vitamin D3 50,000 units that was supposed to be given weekly but was given daily. The other was if I remember correctly a muscle relaxer that was duplicated a generic and a brand name both being given at the same time. This was picked up utilizing the QIS system. Otherwise it seems a waste. Checking for labs related to all of the medications yields some isolated findings but most long term care residents were monitored every 3-6 months and the facility would recognise the omission eventually. However, tracking of fingerstick blood sugars and the administration of sliding scale insulin for coverage or notification of the physician for blood sugars outside of the parameters needs more attention and gets almost none with this system. Tracking of protimes also needs more attention and gets none with this system.
Because QIS is so focused and the pathways require so much documentation I am discouraged when asked to do an entire pathway for an isolated observation or finding. The time contraints and team staffing contraints prohibit the addition of more pathways. I believe that a direct cite is warrented when all of the elements are addressed – observation, interview and record review.
The first two days of the QIS process (Stage I) and the part of Stage II where surveyors investigate things they know weren't a problem but were forced to trigger during Stage I. QIS could be an excellent training tool that provides an example of evidnece based process – collecting data then analysis and then investigating comprehensively to "close the loop" There is a lot of wasted talent in the dta collection Stage I activities; CMS could authorize CNAs and brand new surveyors learning survey process to collect data in Stage I and then have seasoned surveyors with more advanced skills and education conduct Stage II – I'd still give those more advanced surveyors greater latitude to use critical thinking skills and survey rather than just following the written pathways as a checklist
Many Surveyors (in response to this Question and many others) are critical of the time constraints on their Surveys, often commenting about unrealistic workload requirements and insufficient Survey staff:
We have many many issues to look at during a survey and there is limited time to review any 1 issue.
Time constraints, all task are important
I do really think all the tasks are important–. I do think also if the facioity is over 150 residents we shoul have 5 days instead of 4.
It's not that I think some tasks are unnecessary or less important, but I believe the survey process does not provide sufficient staff and/or time to complete all tasks as thoroughly as I would like to.
F329 takes so freaking long. I once had 4 to investigate, and I thought I was going to have to start using antipsychotics.
If involved with a situation regarding pressure ulcers, pain there may not be sufficient time to look into all aspects of the psychotropic drug monitoring.
Not less important, but in order to investigat throughly we are not given the time necessary to really investigate adequately. We are allotted three days, with 3-4 surveyors for recertification survey. Therefore the time necessary to really do a good job for any tag is compromised.
I understand the need for survey tasks but it is time constraints of the survey that make it very challegening epecially when social workers and dieticians are unable to work more than 40 hours a week.
Just the multitude of areas & tags we evaluate. All are important in their own way, however, the amount of staff we have on teams, in such a short period of time out at each facility do not allow all ares to be sufficiently evaluated or assessed for compliance. We are like the "Jack of all trades but Master of None." even though it is expected that we are.
No. I believe the survey process has been streamlined down to where everything is important. At times, some aspects of a survey can become a bit overwhelming when the facility has a lot of problems. Gathering the important information to support a deficiency can be very time consuming. At those times I worry that other areas may not receive the attention they truely need, but I always try. It seems like the problems found earlier in the survey receive the most work. Things found later are often rushed through. But no particular tag is responsible for this. It's just a timing thing… what was found first. These early problems are brought to the attention of the whole team and additional information is sought.
The survey process is very involved and many different issues must be considered. To properly evaluate as outlined each of the areas of concern limits the amount of time available to determine whether or not deficiencies exist. There are times when one surveyed resident takes a great deal of investigation, this limits time available for other issues. We are expected to evaluate care that goes on over an extended period of time in a matter of days. The above F- 329 investigations require a great deal of time to gather information as it is not generally together but must be pulled from many different sources
I think that it is an issue of time rather than task. If done correctly, it takes lots of time to investigate a resident for F329. Once a determination is made, then more residents have to go on the sample and it takes almost as long to investigate F329 for them. Very time consuming!
I do think the traditional survey process is very writing intensive. Having to handwrite all the residents meds and recopy the MDS info, and all interviews/observations is time consuming. I also think that a lot of the things we look at, such as observations in the environment, are also looked at by Life Safety. If we could coordinate our efforts and talk to Life Safety prior to arriving then we could save time having to investigate those items that are shared between the two divisions. I think that the biggest impediment to investigating is that the minimum nursing hour requirement is no longer realistic, and allows the facilities to operate with inadequate staffing in relation to resident needs.
Its not that survey tasks are unnecessary but, certain residents have so many issues that at times its difficult to have the time to address all triggered areas to the full extent.
I don't think that can be answered yes or no for all situations. In general, I believe qis causes surveyors to spend too much time documenting and reviewing things that are not concerns and that takes away from focusing on other potential problems at times. The concept of surveyor initiation of possible concerns is sometimes impractical due to time constraints. That is my belief about the whole process, not just F329
Not really, It is all important though time management is essential. There are many things to look at and never seems to be enough time to do as thorough of a job as I would like.
I do think having nurses look at resident funds is a little much: we really aren't trained in that area and seems our skills would be better spent in other health related areas.
Securing Abuse/T6 employee interviews is time consuming and involves time constraints especially when on a survey w/only one other staff and we have only three days to complete the survey; having to gather 8 staff interviews and ensuring that all areas of the interview are recorded (and maybe a 9th employee) for each annual survey can be challenging and will end up taking priority over the review of a clinical record.
not enough survey time to explore all the required elements to investigate a 329
Additional information on entrance sheet especially if in the role of Team Coordinator…lengthy MDS reviews, surety bond and waste disposal contracts. A total of 8-9 record reviews. I think the problem is that we are not given a sufficient number of surveyors to conduct the survey in the first place.
The survey process gets more tasks almost yearly (F371, F441, F309…) and we do not get more time to do them. Every survey has become a series of choices on what issue to invest our limited time.
Pick focus areas for the year and communicate it to industry, as time goes on, circle back on the improtant ones.
No. All tasks are important, but there is just not enough time to complete a thorough investigation. This is not the case for all of the SNFs I survey, just some of them.
The task are all important. Time constraints to complete all required tasks make it difficult to complete all observations, interviews and record reviews for all tasks and F-tags.
There are times when CMS initiates S & C memos and expect the surveyor(s) usually team leader to inform the facility. List for entrance conference seems to have grown over the years that entrance takes a chunk of time from the team leader who has to proceed with other tasks. Is anyone looking at the time frames of surveys. Getting to the point of being rushed which can impact quality of work. When CMS staff completes look behind/validation surveys they have either a considerabley larger team or spend a considerable lengthier period of time in the facility. IF all survey team members took all their breaks and lunch they would not complete the survey within the required time frame. Also, CMS needs to evaluate the requirement of sampling four residents receiving antipsychotic medications in Phase 1. It makes the process difficult at times due to the other areas that are required to be incorporated in Phase 1 based on QIs.
I understand the importance of interviewing so many people with this deficiency, it is just difficult sometimes when surveying to find enough time to interview all of these people in regards to F329.
no. I just wish there was more time to do a thorough job.
Too many tasks. Takes away from qualitative surveys. Not enough days, not enough surveyors to thoroughly complete everything in a qualitative manner
Several Surveyors mention State mandated tasks detracting from their Federal responsibilities or duplication of effort:
The state requires a review of staff, whether there are necessary background checks and training. It is much more than the requirements for abuse prohibition protocol. This task takes a significant amount of time to review, when we already look at some information of Task 5G.
No, State mabndated tasks often take away from survey time.
group interview, staff interviews required by our state, environmental tour at the end of survey, MDS review.
All of our activiites are important – it is hard to rate one over the other. My top issues Infection Control – Unnecessary medications – Pressue Ulcers(hydration, nutrition, …really Quality of Care, and of Course Quality of Life. When the above areas are investigated thoroughly it seems that youwill uncover areas of abuse, lack of appealing food, issues with PM snacks, etc.
Surveyors note unclear Federal guidelines/requirements and paperwork and other survey process hindrances:
Psych diagnoses are complex and sometimes lifelong. With no psych background I find drug reviews for residents on antipsychotics past my comfort level. I try my best to do a good, fair and accurate evaluation and ask my team for help. It would be helpful to have a short list of criteria to use as a guideline instead of extensive paragraphs full of mumbo jumbo that means nothing. The current is overwhelming and too long to use every time youo have unnecessary drug reviews.
F 329 is not difficult to investigate. I believe CMS is under the impression that surveyors are experts in health care. Read our job descriptions. Only have to have an associate degree in nursing and 2 years experience in the field to be qualified for this position. Dietitians don't have to be registered to be qualified for this job. In this field office we have several surveyors who never worked in health care and don't have degrees in it either. Surveyors are to determine compliance with regulations only. We are investigators. We are not qualified to teach facilities on how to render care. You wouldn't want us to. Our supervisor doesn't have a degree in health care and never worked in health care.
There are alot of forms and paperwork that I feel should not be the teams responsiblity. Most if not all of these forms should be done by computer and email. I think interviews of the residents and family are outdated. The forms are redundate. We are required to fill out the forms in their entirety and I feel that we should only have to fill them out with concern information and that the interviews should be an open discussion. I also dont feel that reviewing entire MDS information is pertinant. Getting this information requires alot of staff time since they are computerized. The faclility has to print them out. I feel that we should only get what we need from an MDS if it is an identified concern. I think the division of safety inspection should be the ones to regulate fire drills, generator safety, ice machine drainage, water temps, etc. There are alot of things that need revamped in the survey process.
I feel specific disciplines do not investigate F329 as they feel it does not fall within their scope of practice. I also feel it is harder to get the more tenured surveyors to investigate possible F329 deficiencies. Many times there is only one nurse in a large facility who does not have an opportunity to review antipsychotic medication use due to observations for resident care, infection control, showers, wound care, etc…
I do not feel any are less important or uncessary. However I do feel that they are extremely lengthy in investigative protocol and it is extremely frustrating to be able to complete everything and do a thorough job especially if the sample needs to be expanded.
the rigidity of the whole sample selection protocol makes surveys less effective. Fed protocols force surveyors to sample certain records that fit into categories just to meet those protocols. It prevents surveyors from focusing on areas of concern that arise during the initial tour. Also, the overemphasis on the importance or the MDS is a waste of time, time that could be better spent elsewhere.
everything is important, however there is too much detail in investigative protocols. wish it could be simplified.
Sometimes it's hard to prioritize correctly. I have left med review for "later " and really regretted it.
The extensive paper-collecting/proofreading from the Entrance Conference Checklist [facility licensure form, influenza information, irrelevant information verification on the census/condition (pay sources, ADL numbers that become part of next year's CASPERS, etc.) administrative licenses, civil rights questionnaire, and various other items could be completed via fax/email to the central office prior to/or after the survey and not bog down the survey team from actually investigating regulatory requirements.
Filling out the forms which should be pre-populated with available technology
Our team tends to get "bogged" down from time to time on the issues of the group meeting. While I do believe the group meeting is of upmost importance I do not think it should take 1.5 hours in a 30 bed facility (5 residents in attendence) and then the rest of the day chasing down each issue. If it is a re occuring issue – sure. I think we should randomly check a test tray from the kitchen with each survey. It is always a group concern so we should just take it on as an issue from the start.
The Family and resident interviews are very time consuming. The questions do not really provide enough informtaion to target specific deficient practice areas such as F329 or F314 or areas related to Quality of Care or even F441 of Pharmacy Services. Individual Resident and family interviews should be utilized to complement the Quality of life and care or resident assessment in my opinion.
Demand billing. Because in 20+ years there have only been 2 requests.
Closed records. If someone was truly unhappy about the situation, death or discharge, they would call us.
QA interview. Because the staff will tell you the "right" answers regardless of what they actually do.
A fair number of Surveyors cite providers’ “computerized records” as a problem:
Interviewing 5 random staff for abuse-one must be 11-7A. Reviewing staff licenses. Review beauty shop licenses. Reviewing Medicare "cut letters," ? UMR. Very time consuming trying to pick Phase 1 residents-waiting for the antipsychotic list and we must include 4 residents and making sure we have enough WHPs and interviewable residents, and residents who have families for interviews plus ensuring all other categories are met, Facilities who are computerized who place all the computers in the conference room which lessens observations or they have difficulty getting us connected which takes time. The time it takes for some facilities to provide paperwork. Checking ice machines for air gaps-?DSI
No, I don't think any of the tasks are any less important than any other. What I do think is important is the amount of surveyors on site and the amount of time allotted to the surveyors on site. Computerized records make things challenging in terms of getting observations and doing the work from the computer limits you.
As facilities become more computerized, the time involved becomes greater to do a complete investigation and come to a decisive conclustion. Therefore, to complete the survey process and evaluate antipsychotics in depth when other issues are predominant can become a time vs. profiency issue.
I believe computerized records and access issues take up an extraordinary amount of time, particularly relating to using facility computers for MDS review – this also often takes surveyors out of the resident care areas and to a back office limiting the observations of resident behaviors, staff treatment and care delivery.
Defining the type and amount of interviews by facility size rather than the concerns being raised isn't always useful.
Access to gain electronic records is necessary but can be time consuming at the facility.
A number of Surveyors indicate that providers “know what to say,” are not truthful, or hinder the process:
The depth of 5G – while I do beleive it is important to check the employee files for a registry check on the part of the facility – to ask the same questions of so many staff members becomes reduntant. As all employee's know what to say. I think it is more important to observe for abuse and if you have complaints of such from family and residents to dig deeper at that time.
tour. Generally, staff lie about the residents, hoping you won't pick them. I try to choose a sample based on my observations, unless the person giving report is candid. Sometimes, facilities will give us restorative aides who won't tell us anything. Then we have to depend on QI reports and our observations anyway.
Several miscellaneous Surveyor responses provide additional insight:
If I do the nine core elements that I first wrote of, I believe I can well evaluate anti-psychotic usage. I'm very proud that our region has been 'gung-ho' on this for well over six years and have seen a significant improvement in facility compliance. Other F329 concerns are fairly self evident with the first physician order sheets review and investigative guidelines from there.
I think the big thing I don't like about F329 – is that I'm not a Pharmacisit, and yes, at times I do look at the drug interactions, but to actually cite because there was a possible interaction between to drugs…is hard for me. Especially when there is a monthly pharmacist review and there are no irregularities noted – so then I feel like – this is a Pharmacist job – to assess for interactions – Why then does a surveyor need to look up every drug to determine possible interactions? It can take a chunck of my time during a survey, especially if I have to review 3 unnecessary drugs
Reviewing for activities. Many times these people can not participate in activities because of their behavior. Behavior is very difficult to control and manage, and many times you are not going to change a person's behavior because they've been acting that way most of their life–it is part of their personality.
Looking at boiler and dumpster. (It can be spotless 300 days of the year and then on the few days it is not the survey is in progress and the facility gets a deficiency)
Medication pass (The best staff get nervous and make mistakes, the staff that are devious never get caught because they are devious. At best, we gain no useful information from it. At worse, people get fired from jobs)
All survey tasks are important however, pressure sores, restraints, dehydration, pain and other major care areas often become primary focus just because I am a nurse and I know resident care very well. Many of us are not extremely familiar enough with antipsychotics and other potentially unnecessary medications to speak on a level basis with the prescribing/monitoring physician. Its more of a comfort level problem than anything.
Group Interview – rarely results in citations as the residents usually have not informed the facility of the problems. The group interview is often used by individual residents as a gripe session.
Closed Record Review – rarely results in federal deficiencies.
F329 deficiencies are difficult to determine and charging the pharmacist with recommending a gradual dose reduction from the MD when they do not understand the interactions for psychotropic medications puts residents on a roller coaster for control of behavior and/or psychiatric condition. Psychotropic medications should be prescribed by a psychiatrist and reviewed by same. Once resident's medications have been titered by a psychiatrist they should not be changed just because the pharmacist said CMS requires it.
when mds pull up a 99 year old resident with mulpil conditions for community placement.
Resident and family interviews forms questions are not appropirate to issues at hand or of no value in some cases.
Review of facility policy, policies are often developed using direct wording from the regulations and not tailored for practical use in the facility
MDS tasks such as vision, incont for bladder and bowel, lack of transfer for rehab, ADL for cleaniness-these tasks are less important/unnecessary because half of the time they are on expired residents or on residents who are discharged and when you go to do interviews half of the staff don't even remember the resident. And also, half of the time you don't end of citing anything out of this anyway and if you do, it may only be a care plan tag.
I think there needs to be a sliding scale on the number of clinical records chosen to represent the antipsychotic medications. Four charts is too many when you only have 5 charts in Phase I, and you have to also find interviewable residents, or resident's whose families can be interviewed, in additon to the other areas that need to be selected.
The intense investigation that is just a required part of the survey. I feel as though some of the review (meds/MDS/QA/abuse&neglect… are very important, but sometimes we can spend hours on these things where there is not a problem and it tends to take the focus off the problem issues (such as F329) as well as other issues.
I don't believe routinely assessing all medications for interactions, side effects and adverse reaction, such as using a drug review program and printing it out is necessary. I believe if you are looking at the resident, interactions with staff, interventions for behavior, and acute medical conditions which arise, then you will identify medication issues. There are usually some key medications which raise red flags for me and they are antipsychotics, antianxiety meds, and hypnotics. It is seldom hypertensives are not needed, but sometimes there are not parameters for their use. I also strongly believe that surveyors who are not nurses, or pharmacists have a very difficult time with F329. For nurses it is second nature to look for all those things, and to know who to interview and what to question. The survey team would frequently disagree with the nurses for lack of understanding what we were saying was a problem.
Almost all of the Stage 2 MDS-triggered tasks such as vision, incontinence decline, transfer decline, no discharge after 60 days after receiving rehab, etc. take too much time of our survey time and add little to improving the QOC to the residents. I also do not believe looking at PASSR and Hospice on Stage 2 adds any value to the survey process.
Don't want to spend alot of time uon residentws when the psychiatrist state in an assessment that resident's behavior is stable under this regimen. Staff, especially second shift, don't have the time to deal with residents with a history of psychosis who have many difficult behavior issues for a nursing home staff to be able to deal with.
all the tasks i mentioned are important. A devised check off list for each resident would be helpful As part of our resident review worksheet
No, all tasks are just as important as spending hours and hours trying to find some way to punish a facility for using physician ordered medications so that someone at the Federal level can get up on their hind legs and bray proudly of how they have reduced the use of necessary psych medications in health care facilities.
Some of the tasks associated with general obs overlap with tasks Life Safety surveyors also perform. It would help health surveyors to have those tasks which overlap deleted from the general obs task.
The Civil Rights review task done every survey, year after year, without indications there is a concern. The answers never change and are not as relevant as observations, resident / family, interviews and staff interviews throughout the survey.
The same can be said about the QA Review interview without evidence of any concerns with the facility's QA process.
The infection control review protocol is long and time consuming and done with each survey whether or not there are any evidences of an infection control problem determined by Phase I and II Resident Reviews.
Title six interviews. I can tell you that in 11 years I have not had any issues with descimination, lack of handicap access etc.
Sample selection has become very time consuming with the last revion by CMS. Having to wait for the facility to compile info in regard to who is on or has taken AP medis in the last 30 days. The requirement to look at AP use in Phase I is very difficult to do in small facilities where you have a limited # of record to look at in Phase on especially if you have to WHP the sample sel;ction. It was much easier to do sample selection for AP use when the the AP use was on the facility Roster. It would be easier if we could look at Ap use in Phase II. It would be easier too if the rosters actually matched the QM's .
Form 806C Family interview as it is currently written and used, is time consuming and provides relatively little usable information for the survey.
I think its more the issue of going to facilties every year…I would rather reallocate resources to be in the bad facilities more often. I would say the requirement to pick people on antipsychotics is misguided. We should pick people with dementia who have no behaviors or psychiatric conditions yet are on these drugs….the low risk QM.
number of abuse interviews required. WHPnumbers, most pressure sores in my facilities are not facility acquired, structured resident and family interviews with specfic number, most of those questions are stupid. Interview resident based on the deficient practice you see or find. Sometimes a quick chat tells you more then and formal one does. Group interview..residents usually give individual concerns
Question 18: When citing antipsychotic drug deficiencies, do you:
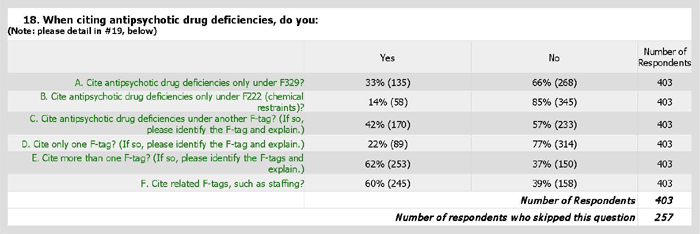
Question 19: Add any details or comments you have for the items from question #18, above:
When citing antipsychotic drug deficiencies:
A) [Do you] Cite antipsychotic drug deficiencies only under F329?
Although 268 of the 401 Surveyors (66%) indicate that they cite antipsychotic drug deficiencies at F-tags other than F329, 135 Surveyors (33%) answered that they cite only under F329. Even when Surveyors indicate they cite other F-tags, their emphasis, choices, and explanations are quite varied. Some indicate that insufficient survey time dictates tags cited or that they “focus” on F329. Others note additional (but often different) common F-tags. Still others will not cite multiple tags for the same example.
tend to cite the strongest tag – not time to cite all associated tags
In my short time of OJT, this has been the tag I have been taught to focus on.
Not always, sometimes assessment deficiencies, sometimes care plan deficieces, pharmacy deficies, etc.
could go under F323 if outcome related to the medication use
No ithe justification for the medication has to be determined also…staff convenience…to chemically restrain the resident..due to a lack of staffing etc?
generally yes
Not just here if other F-tags are appropriate, such as F428.
try to cite at most specific area
many tags can be evaluated – activities and staffing come to mind immediately
sometimes assessments, care plans, F428, F309 for not following physician's orders
Other issues may also exist, such as lack of care plan, lack of behavior plan, lack of assessment.
if medication administration error is observed cite under F333
may have dignity issues
May have other tags such as under administration, nursing services
usually here first but also looking at associated tage
depends what has been cited in the past, and if they reamin out of compliance
may cite 281, 282 implementation care plan
Normally involves other deficient areas involves
It depends on the individual situation, we may also cite behavior programming under F309, F319,or F320 or F250 or F248
some times it might be cited under other tags; for not assessing/monitoring, not developing care plan etc.
cite only under this-I believe this tag covers the whole thing
No. We can also Pharmacy services, F425, F281 professional standards
This is the most common place for these types of problems.
This is the F tag that I have needed
So far, this is the majority of the deficiencies
Each situation is different, and the most appropriate tag/s should be cited.
May cite staffing, assessment, care plan, SS, activity, pharmacy tags, not often not always
No depends. Look at other tags, 154, 155, 157,272, 279, 280, 325,385,428
No b/c we have had Med Errors cited under F332 & F333 b4
Need to look at more than just the drugs
Evaluate to see if there was a significant med error with it, or failure of RPh or physician
could have excessive falls and weight loss.
usually cite 425 with issues of medications
Look at quality of lige, dignity, staffing, chemical restraints, F425, documentation
No to all above as I have not cited anti-psychotic drug use yet.
Would depend on the situation. If there were no other aspects to the problem, then we would, but if there were additional issues, such as lack of staffing, meds used for checmical restraints, etc. we'd opt for more than one tag….
No look for relevant tags related to affects the drug had on each resident
usually also include F 428 if appropriate
Every single deficient practice identified shouold trigger surveyors (1) to look at the facility QAPI program – did they or shouold they have known about the concern before the surveyor found it; (2) to look at medical staff accountabily if it involved medical care as anti-psychotic med use would; and (3) governing body responsibilities. Many other F Tags may relate depending on the actual findings, nursing services, pharm, dietary, etc.
depending on the severity of the outcome a 309 may be more appropriate
No also have cited under 428, 323, and 333
either F329 or F222, not both for the same example
I have not had a situation where another F tag was applicable.
At times if there is only potential for outcome and documentation is a problem it could be cited under 514 on occassions.
Depending on the findings at times use F319
No, depending on the issue, can relate to QA, Medical Director Activites, staffing, etc.
could be cited under F222 if antipsychotic med is being used to sedate residents who exhibit undesirable behaviors and staff are not properly assessing and monitoring
This is dependent on the individual situation and the scope of the citation,
B) [Do you] Cite antipsychotic drug deficiencies only under F222 (chemical restraints)?
Eighty-five percent (85%) of the Surveyors indicate that they do not cite antipsychotic drug deficiencies only under F222. Although a common Surveyor response to this question focuses on restraint, Surveyors note that F222 is difficult to prove, “just [their] opinion,” and that “it needs to be modernized and re-vamped [because] there isn’t a lot of information for Chemical restraints.”
cand do both areas if they are using them as a chemical restriant.
Only if applicable to being a restraint
In [State E] we do not get to cite F222 very much. I tried citing it back in 2005 and it was moved to another regulation.
This would seem hard to prove…that they were using it as convenience…
I haven't used /looked into this much
potentially this is cited, often not
Its just not done–I have been told its just my opinion-
perhaps, but ususally involves more than one tag including F309 if inppact to resident is negative in daily function
If being used as such. (i.e. before a bath and resident dislikes baths identified by staff and no alternative plan developed)
F222 if applicable. If someone was drugged to where they could not function, but this is rarely the case.
Have not but would use it if I had evidence to show it was used a s a restraint. I had not thought of this opition before but yes it can be appropriate and I would use it.
no cite also under 329, orif appropriate consents,
when drugs arwe given in high does with out justificatins
this may also require a 425 or 428 tag depending on circumstance
some times it might be cited under other tags; for not assessing/monitoring, not developing care plan etc
I think F222 needs to be modernized and re-vamped. There isn't a lot of information for Chemical restraints.
It would be cited here if the resident appears to be "over sedated" and we have good supporting documentation chemical restraint has occurred.
only when it has been determined that the staff is using the drug as a restraint. I have not identified this practice in a long time.
It is rare that you can show chemical restraint, but it is an option
I'd only cit this if I felt the resident was overly sedated.
I would only cite this if a resident got prescribed a new psych med without indication and the resident showed behaviors that the facility didnt know how to deal with besides give a medication.
I have not but could see this being used.
Not always a chemical restraint could be a staffing problem
not yet. but understand how it is a chemical restraint
have not identified any use of chemical restraints
I have not seen our office use this tag
Yes if the resident was being chemically restrainted or was not consented.
It depends on the circumstances surrounding the use of the medication. For instance, if the medication is administered the instance the resident acts out and there is no evidence of attempts at nonpharmacological interventions, then this tag would need to be considered
I have never done that yet!
haven't ever
May also cite F- 329,428, 501and 520 if appropriate
Find it hard to support that the intention was to use the medication as a restraint.
either F222 or F329, not both for the same example
This seems harder to prove.
Not common to use this tag but can be used possibly in conjunction with another tag.
only if resident is obs to be oversedated
not always. if the resident is negatively affected by the drug use it could fall under QOL or QOC
these are usually also the places that physically restrain so it may have both
Chemical retraints are hard to cite based on definition…so most of F222s becom F329
tough one to prove
C) [Do you] Cite antipsychotic drug deficiencies under another F-tag? (If so, please identify the F-tag and explain.)
Although there is a level of consistency in other antipsychotic drug deficiencies cited by Surveyors, they also note an exceedingly wide range of various F-tags as alternatives. Abuse is cited by two Surveyors.
F323 if outcome related to the medication use
It could be more a problem with proper monitoring of the medications and lack of documentation.
facility staffing could be cited if it is determined that the use of the medication is related to staffing.
Following Care plans, Staffing, developing care plans, consents, notification.
medication administration, care plan, follow physician orders, pharmacy
There could be a significant med error, there could be failure to follow physician's orders
F309, F319, F329, F222, F226, F353
F-428. Consultant RPh role.
unlikely
F514
may also cite F428
I think that sometimes it could be cited under F514 if facility is not documenting behaviors and/or effectiveness of the antipsychotic
F-279-care planning(interventions) F-428-Consulting Pharmacist/irregularities F-250-social worker involvement in behaviors/medicationsF-319-Does the resident need outside psych consultation.Also in F-428-did the physician act on the pharmacist recomendations or provide a reasonable explanation
F309,F272, F279, F428, No behavior plan, No assessment, No careplan, No drug regimen review.
F309 lack of behavior plan, F272 lack of assessment, F279 lack of care plan, F514 lack of documentaion
Reveiw interpretive guidlines in F222 / F320 as well as triggers in Append Q
F241-if dignity is noted
F-425 if error in administration of the drug
F272 – Lack of Assessment ; F425 – Could be arrors in administration, doseage
157-notification of change; 154 et 155-rights, services et choice; 272-comprehensive assessment; 279 et 280-care plans; 310-decline in ADL; 315-urinary incontinence; 319 et 320-mental et psychosocial functioning; 325-nutrition;327-hydration; 385-physician services;386-physician visits; 428-medication regimen review; 501-medical directorc
Will cite multiple tags if necessary ie: F248, F250, F279, F386, F428,F514
If there was a medication error I would cite 425, lack of consent for medication use would also be a state tag. Pharmacist recommendation not followed I would cite 428.
Its case by case… may cite F222… or F425 also… or have cited consultant pharmacist tag…
309 when the general life of the resident is affected by a failure or effect of psychoative medication,279 ; when behaviours is not care planned ans resident not assessed or monitored.
F-240, F-241, F248, F272, F274, F276, F279, F319, F323, F325, F327, F 353, F385, F428,
F425 if resident is receiving a medication that should have been discontinued or changed. F281 if a nurse is providing the medication without checking physician's orders, which is part of her job.
F329, sometimes F428, and other tags, depending on the findings.
F319/F320, I would ensure the appropriate mental health care was also provided
309 if there is side effect- i.e. chocking on food or 323 if a fall caused by psycotropics
Not typically done.
They can also be cited under Standards of Practice, F309 for inadequate care and services, insufficient staff training, abuse
Would always cite any related tags if appropriate, such as pharmacy, care plans, or sometimes inaccurate or incomplete medical records.
Possibly 225 Abuse
May lead to citing staffing, assessment, care plan, SS, activity, pharmacy tags
cite where the breakdown in the system has occured, could be F329, F309, F222, F514, F279, F353
possibly 157, 310, 319
No b/c we have had Med Errors cited under F332 & F333 b4
Our office moves these to 309 or 514 quite frequently
F-248-drug regime, F-278 accurate assessment, F-309 Care & service for highest well being – resident always asleep, wt. loss , F-323 accidents & supervision if falls occurred etc.
If there was not enough information, it might be cited at F309 so that the facility has to address a failure identified
F 323 F 325 F 327 hydration. F 318 F 314
often under F 278, F 280, assessment and care planning
F323 or F22, F223, 224, 226 as related to accidents or incidents
sometimes if our team does not feel the tag is strong enough it will end up under 309
depending on situation Resident could be to old for efficacy
F 309 or activities or weight loss or injuries
would use 425,
yes; F-425; 309; 157; 272; 428; 431; 279
Again, it is hard to speak globally but depending on the circumstances surrounding use of the medication, you would have to consider Activities if there were no or insufficient evidence of a structured program.
F428 if consultant pharmacist reviews are not being done or are not acted upon
Typically F329 & F428. Have cited a physician services/medical director tag in situations where everyone else filled their role; however, the physician was adamant about a treatment path without rationale.
F240, F273, F 280, F 309, F 310, F353, F385, F 425, F 497, F 498
F309
sometime compliance reviewers insist on same info in different tags
309 quality of care and 225 possible abuse, 279 and 282 care plan developement and implementation.
Could cite under appropriate staffing (very hard to do), F323 falls
maybe F309 if the med use negatively effects the residents , F222 if the antipsychotic is used as a restraint, F151 if the antipsychotic med administered violates the residents rights, F279 if the plan of care is not followed, F329 if it is determined the medication is unnecessary, F428 if monthly drug reviews are not conducted or not followed
428 281 sometimes but many professions have generic standards, hard to put it there. we are to have a quality outcome also for 281 and that is hard to prove
D) [Do you] Cite only one F-tag? (If so, please identify the F-tag and explain.)
Seventy-seven percent (77%) of Surveyors indicated that they do not cite only one F-tag when citing antipsychotic drug deficiencies. Considering Part One of this Report noting a total of 29 F222 deficiencies cited by seven states over a three year time period (compared to nearly 300 F329 deficiencies cited during a two year time period), further data analysis of Surveyors citing multiple F-tags may be warranted.
Typically only F329.
F282; F428 sometimes also cited and cross-refered to F329.
We are often lucky to get one tag through with sufficient evidence to proceed, so often times we cite the highest CARE related tag and don't pursue a care plan tag, for instance.
depends on circumstances may cite one tag or several (F329, F222, F428)
If only one resident cited, choose the best tag to use. Do not cite two tags for one resident.
Tend to cite only one tag that is most appropriate for the circumstances.
Depends on the issue to which one is cited and if more than one tag can be cited.
Normally involves other deficient areas involves
It may only be cited at one tag, if the problem is isolated and the one take will get the correction needed.
some times it might be cited under other tags; for not assessing/monitoring, not developing care plan etc
I don't know how we would cite one F tag like 329 without citing 425
usually staff use 329 but at times also use 281, 514, or 222
We typically site F329 unless the resident is over sedated, then it may go under F222 instead of F329.
depends, less tags cited is state wide thought
Each situation is different, and the most appropriate tag/s should be cited.
If pharmacy did not identify irregulaties with psych meds I would cite F428.
No b/c we have had Med Errors cited under F332 & F333 b4
It can be more than one deficiency–lack of monitoring, lack of informed consent
We've been instructed to cite it once not the same issue in other areas
More effective if tied to other deficiencies related to care
usually F329 or F279 (if possible F329 is the preferred tag)
depending upon the situation more than one tag could be cited
Might only cite under 329 or 222 depending on the findings and what the emphasis was. We might include aspects of the other tag to support the one carrying the most weight….
Generally F329 is used.
F 329…policy not followed
Usually will be 2 tags or more
yes depends on outcome
Which ever appropriate tag has more severity associated with it.
assessment and careplanning usually are cited as well
sometimes compliance reviewers insist on using only one tag
F329 which cover more about antipsychotic medications.
F329, F222, Activities, Staffing issues, Pharmacy, Physician
This is dependent on the examples and scope of the citation.
no we place where ever it fits best for the benifit of the resident involved
depends put the deficiency were it has impact.
Sometimes cite F-514 for medical record
E) [Do you] Cite more than one F-tag? (If so, please identify the F-tags and explain.)
Sixty-two percent (62%) of Surveyors indicate that they cite more than one F-tag when citing antipsychotic drug deficiencies. There is a great deal of variability in the F-tags identified by Surveyors. Some Surveyors note “time to cite” issues or explain that their “office does not like to cite more than one tag per deficiency.” Some Surveyors note “staffing” concerns, a few note “Abuse/Neglect,” some note “falls,” and many note “care plans.” Several Surveyors indicate that “F329 and F222 seem to go together” and some say that their citing more than one F-tag “depends upon outcome.”
it takes too much time to cite every possible tag, and gains nothing. Cite the most relevent tag and move on to the next task. We have to be more efficient with our time.
Only if necessary
F428 if not recognized by pharmacist or the physician does not acknowledge the pharmacist review.
Sometimes F428, F250 and F406 comes into play.
Social services for failure to evaluate factors that could have contributed to the behaviors exibited by the resident.
In many instances F329 and F22 can be cited as well as facility staffing.
F333 or F319, F318
pharmacy services depending on the involvement / or recommendation of a pharmacy consultant.
informed consent; social services, supervision, physician involvement Med Director awareness, Consultant Pharmacy involvement documentatin in the clinical record
F309, F319, F329, F222, F226, F353
If the facility has not car planned for non pharmecuetical interventions and indicated specific interventions that might actualyy be effective then i waould also cite care plan not developed, if interventions not effective or not attempted then i would cite that.
depends on circumstances may cite one tag or several (F329, F222, F428)
F-329-the physician did not provide a diagnosis and F-428-the consulting pharmacist did not identify it.F-329 a resident receives a sleeping pill because her roommate yells all night. F-250-the social worker knew but failed to intervene. F-329-no interventions prior to adminstration of psych. med. F-279-no care plan identifying interventions. F-280- care plan was not updated.F-329-sleeping pills with no prior interventions F-323-falls at night
poss. 281
Professional standards, F333
If there are two or more residents with different problems identified may use both F222 and F329
MIght cite F279, F282, F280 related to development, updateing and following the Care Plan
329 or 222 or staffing if indicated
F490 – Administration ; F520 – QAA ; F240 – Quality of Life ; F241 – Dignity
there usually are associated tags based on the situation such as staffing, activities, care planning, social services
155 – Right to refuse. If medication given IM after resident refuses with no evidence of potential threat ; 386- physician services for failing to respond to recommendations , fail to have a justified diagnosis or order a medication in the absence of symptoms , 428 – pharmacy failing to identify or question continued drug use or the diagnosis for use
F425 or F428 may be considered; may consider F250 related to behaviors and lack of any intervention to address possible causes; F319 or F320 if evidence points in this direction regarding adjustment
depends on the cite, many tags may be out of compliance
Sometimes it may only be at F329, but if the situation warrants there may be findings under other tags such as behavior progamming at F309, 319, or 320 or preferances may be cited or the activities program may be cited if there are alot of residents being cited and the program is def. etc.
some times it might be cited under other tags; for not assessing/monitoring, not developing care plan etc
F428 drug reg review, F319 Mental/Psychosocial adjustment
depends upon situation – would review SOM/Guidance
If there is an issue with Neglect then we go that route as well
F279 is often cited in addition to 329 when the facility has not developed a care plan with appropriate interventions. Also 272 if the staff has not performed a thorough assessment of the resident's ADLs, behaviors and attempted to identify possible causative factors.
Look at related tags also, such as assessments, care plans, staffing, documentation.
F154, F155 not advised of medical condition, F272 no assessment, f310 decline in adl, f319 mental & psychosocial functioning, F325 Nutritional F327 hydration, F385 physician supervision, F428 MRR, F501 medical director
Abuse, chemical restraint, staffing,
If the citation was in regard to the facility's failure to monitor and there where significant blanks in the MAR or behavior monitoring sheets I would cite under 514 medical records.
May cite staffing, assessment, care plan, SS, activity, pharmacy tags as well
As stated above it could be med error, a 319, or a F222
acitivites, staffing social services
Every situation is different and has to be looked at separately. There is no one answer for those questions.
F 309- for failure of the nurse to give the medications as ordered by the physician.For example the physician discontinued one medication and started another but the nurse gave both medications and the resident subsequently observed sedated. F 281 for nursing standars if the nurse failed to clarify the physician orders for a given medication and gave the resident too much or two of the same medication and or failed to monitor for effectiveness of a medication or for behaviors and the resident had long ago stopped the behaivors but was still being treated. If the nurse failed to communicate adverse effects or side effects of a medication. F 425 if the facility failed to procure and provide the medications ordered by the physician and if the pharmacy consultant failed to suggest gradual dose reductions or discontinuing of psychotropic medications
F323 falls, F428 not following pharmacist recommendation
F-241 could be an issue of dignity & respect, those listed above.
Sometimes, also cite RPh at F431, Care PLan tags if care plan not devleoped, revised or followed, F281 if failure of licensed nursing staff,
sometimes use cross-overs, F 502 labs,
Possibly F157, F279, F310, F325, F327, F428, F501, and others.
Our office does not like to cite more than one tag per deficiency
F329 and F222 seem to go together if citing antipsychotics
F329 and F222 I attempt to cite both of these areas if it is relevant; F329 for not implementing interventions prior to administration and also no attempt to dose reduce; F222 I try to apply if staff use an injectable inappropriately or first before an oral form
no dont double cite cite the strongest impact
Generally only one F tag is cited to strengthen the scope and severity of the deficient practice.
Usually cite assessments and care plans.
F329 and or F222 if both are applicable. F222 usually cited re; staff convience.
yes, depends on outcome
Depends on the situation-outcomes could relate to abuse/neglect, self determination, services…
This is dependent on the examples and scope of the citation.
329/222/323151 right yo be free of unnecessary6 meds. falls/accidents from over medication
no reason to double cite if you are saying the same thing in both deficiencies. Facility has to fix the problem.
F) [Do you] Cite related F-tags, such as staffing?
Sixty percent (60%) of Surveyors indicate that they cite related F-tags, such as staffing, when they cite antipsychotic drug deficiencies. Many Surveyors note the difficulty of proof in writing a staffing deficiency (related to either inadequate numbers or training). Throughout this Questionnaire, Surveyors often refer to staffing concerns being directly related to facility antipsychotic drug utilization. Only one Surveyor answered this question by stating they “have not found staffing issues to be related to the use of psych drugs.”
Again, would seem hard to prove deficiency
medication administration, care plan, follow physician orders, pharmacy
F154,F250,,F309,F323, F386, F387, F428, F501, F514
not usually
IF there is a problem and we identify staff is part or all of the cause we would cite it.
usually cited because of staffing
If I had the supporing information such as interviews from staff that it directly related back.
always the potential to look at staffing with medications. Is this therapy related to staff convenience?
if staff not able to follow plan. or cant have effecttive an due to staffimg
Can not do this becasue the facilitys meet the minimum 2.7-which is a disgrace.
observations show staff do not know how to handle a resident's behavior related to dementia which may be as simple as providing a doll for them to hold or providing something of comfort to the resident.
Rarely
This would be cited only if there is additional evidence of poor staffing
MIght cite F157 related to notification, F353 related to sufficient Staffing
If it is determined that the facility did not monitor etc. due to inadequate staff.
sometimes activities in dementia units as staff rely on meds rather than diverting residents with relevant activities
could be Staffing, Medical Director,Physician's Services, QA,
If it is determined that the staff utilize antipsychotics for staff convenience due to short staffing
r/t staffing numbers or lack of training
yes if appropriate, if drugs are givenfor staff convenience staffing may be cited
have not cited staffing related to F329
not usually. difficult to proof
yes, if resident as chemicalky restrained for the benefit of staff
Staffing can be factor of use … the "sedation" of resident
This is usually only cited when the problem of behaviors is occurring with a large number of residents and we can clearly show that there is not enough staff present to handle the problems of residents acting out etc and no staff around or staff being pulled constantly and not knowing the residents' individual preferances and needs.
Yes- Sometimes F353 can be hard to cite.
never thought of this one but maybe so
F499 Staff qualifications
I would only cite the staffing tag if I could determine that care was not being provided, and if we could correlate that not enough staff affects receiving or not receiving antipsychotic
staffing levels are reviewed but mimimum requriements hard to use this as reasion for resident's behavior outbursts and not redirecting residents
This is done if we cite staffing and staff told us they give the medication because they could not get done with thier work otherwise.
Yes, if appropriate. I look at training for staff also.
I have not found staffing issues to be related to the use of psych drugs
yes, was there enough staff to monitor the behaviors
Only if appropriate – has been difficult to prove the connection
If staffing can be proved it may also be cited under staffing.
I think it would be difficult to prove the relationship between low staffing levels and unnecessary drugs.
It's for the facility to decide if staffing is related to F 329 deficiencies.
if appropriate and can be supported.
Not usually- would probably cite F281 if licensed nursing failure in dealing with AP meds
not yet. I'm fairly new. But I do understand how it could easily be a staffing problem.
This takes multiple observations. Not always able to prove.
Our office does not cite staffing because the facility always meets requirement
Usually not staffing. Other tags as above
difficult to cite. direct observation or documentation of specific incident helps
related F tags but usually not specifically staffing
difficult to prove
yes if giving for staff convienence cause of lack of staff.
Haven;t done so but can see how it is related to staffing
if under staffing and residents isolated F353 F221
Staffing is not an issue that we can usually cite/is not supported.
yes if care not done as a result of same
Have not had to, but do see when this may apply.
Yes. If it is identified that staffing patterns contribute to the use of antisychotics.
In our office, I have found this tag was almost impossible to use. Most failure in care was placed under other tags.
353 if applicable along with other tags if this came into the picture
yes; not often unless there was no RN
Again this is a possibility if you determine this was a contributing factor to continued use of antipsychotics.
I have never cited staffing.
calculate staffing for relation to drug use
would cite if had enough evidence
I have cited staffing, but not as it related to F329. It was related to falls and weight loss.
have not linked staffing to F329 but have cited for lack of suffient oversite esp on MCU
Would cite if it were determined to be a attributing factor.
if there is a lack of staffing to provide the care.
Given the regulatory set does not provide us a concrete expectation of staffing, staffing adequacy is often subjective.
If possible to prove but very difficult.
Not commonly used.
if it relates to giving meds for behaviors and low staffing. Hasn't happened for years
only if staffing has been shown to be involved.
This is rare to cite staffing
If resident restraint is associated with inadequate staffing.
Would like to but this state requires a low number of staff
if staff are not aware of the reason for use, monitoring/side effect or insufficient staff to provide care for the resident using antipsychotic drugs
If that would be a proven circumstance
only if I can prove it
if insufficent staffing is the root cause for the use of the medication
Citing Antipsychotic Drug Deficiencies and Assigning Scope and Severity
Question 20: Without simply referencing the SOM/Guidance, briefly describe the core elements of your analysis in assigning scope and severity to F329 antipsychotic drug deficiencies. We are looking for help in understanding how you primarily evaluate F329 scope and severity, in practice.
Asked how they determine scope and severity of antipsychotic drug deficiencies, many of the 402 respondents describe variations on a common theme – scope and severity depend on the number of residents affected and the severity of the effects on residents.
Some respondents identify the difficulty of establishing harm:
It is difficult to prove harm related to antipsychotics so we usually go with a D or E severity and scope.
Harm is only cited if harm can be specifically identified, ie side effect not treated, such as constipation, falls from over sedation. Very difficult to cite at G level as cannot always correlate side effects etc directly to the med.
Defining ‘harm’ is subjective unless it is clearly documented (i.e. excessive sedation documented by staff, resident verbal complaints, fractures from falls, medication allergic reaction.
Some respondents describe using more specific criteria to identify scope:
If more than 3 residents affected, would scope as pattern.
It depends on how many residents it affects – if it affects one (1) to four (4) residents then a “D,” then five (5) to eight (8) then at an “E,” and if it affects above eight (8) residents then I would put it at an “F,” which would be widespread.
If it affects more than 4 residents then a pattern.
If there are more than 3 residents in the sample with concerns for F329, I would cite an E. Or, if one resident has multiple episodes of incorrect use of a psych med, it would be an E. Otherwise it would be a D.
1-5 residents = D
˃5 – ½ of residents using psych meds = E
˃1/2 of residents using psych meds = F
1-3 isolated; 3-6 pattern; 6 plus look at widespread. Systemic error with low examples can be widespread or pattern
Some respondents describe the use of more specific criteria to identify severity:
Level 2 or level 3 and it is based on total number of deficient practice found in at least 3-4 of the residents with antipsychotic drug reviews.
Some surveyors have an approach to assigning both scope and severity:
Never A, B, C
Often hard to prove harm
D – one or a few residents
E – more than a few residents
F – system-level problems
D – no harm to resident
E – more than approximately 20% of resident have Ftag with no harm
G – harm ie., injury or emotional issue
H – approximately 20% residents from sample have harm (p. 8, tra. PA)
At least 18 surveyors from eight states identify the possibility of identifying a jeopardy-level deficiency:
Unnecessary antipsychotics administered to a patient could be assigned a scope and severity from a level D to J, depending on patient outcomes. AP present potential risks to all patients especially if there is no benefit to be gained in giving them or giving them for longer than needed. Continuing to give them in the presence of adverse effects that lead to patient harm where the risks outweigh the benefits or giving them for staff convenience and the patient suffers adverse effects may constitute jeopardy.
Question 21: Do you believe that you are citing F329 at the scope and severity required by CMS guidelines?

Question 22: If you answered “no” or “sometimes” to question #21, above, please explain (e.g., are the guidelines too long, too short, complicated and hard to understand, not detailed enough, lacking examples, complicated by too many choices, etc.).
The two most common explanations for why surveyors do not cite at the appropriate levels are that the guidance is too complicated/too long and lacks sufficient examples.
Too complicated/too long:
Too complicated
Guidelines are long and complicated and hard to understand. There is always a lot of gray area when dealing with medications and we are not physicians.
Guidelines need to be more concise and easier to understand.
complicated and hard to understand
guidelines are exhausting, overwhelming, gray areas
The guidelines are long..and it takes a lot of time to read this during a survey
The guidelines are definitely too long and too complicated to understand. There are also too many scenarios – for example residents may be receiving medications that are classified as sedatives/hypnotics for conditions such as a seizure disorder. There are residents receiving anti-depressants as appetite stimulants. There are residents receiving psychoactive meds that require a therapeutic blood level and we ask them to attempt a dose reduction which makes no sense. The scenarios are endless.
Complicated and not clear. If one resident was harmed because of the cause then that is one to many!
complicated by too many choices
Regulations are long and need more examples.
The guidelines are too long and the need to review other concerns can make the review somewhat cursory.
too many variables
Too long and complicated.
F329 is long, complicated, detailed to the point of overwhelming the surveyor.
complicated and hard to understand
Too long & complex at times to ensure consistent application
There is A LOT of material to sort through on a 3 day onsite survey in the interpretive guidelines. Our former state pharmacist was overwhelmed at the amount of information. The guidelines need to be field references not the whole text book. We try really hard to follow them but things could sometimes not follow everything under F329.
Guidlines are to long, compicated, hard to understand, to detailed and complicated by to many choices.
too complicated and hard to understand — lacking examples
The guidelines are definitely too long and too complicated to understand. There are also too many scenarios – for example residents may be receiving medications that are classified as sedatives/hypnotics for conditions such as a seizure disorder. There are residents receiving anti-depressants as appetite stimulants. There are residents receiving psychoactive meds that require a therapeutic blood level and we ask them to attempt a dose reduction which makes no sense. The scenarios are endless.
Lacking sufficient examples:
need more examples
not enough detail and/or examples
The guidelines do not give enough examples and do not seem to be based in reality. There do not seem to be y drugs that really help dementia and perpetual confusion and distress.
too complicated and hard to understand — lacking examples
hard to understand –not enough examples-not enough training
Surveyors describe the special complexity of citing antipsychotic drugs when the drugs have been ordered by the physician:
I feel that the root of the problem is the perception by some of our team that the physcian ordered the drug so it should not be questioned. This perception is also evident and vocalized in some of the facilities.
Facility practices make deficiencies difficult to cite:
Determination to cite can be complicated by facility documentation (a lot of facilities document by exception only which makes it difficult to get a true picture of the resident), facility insistence that there is no deficient practice which is reported to SA office and can be interpreted as surveyor not being fair, difficulty in telling the facility exactly what is expected of them in caring for residents who require continual hands on care., lack of access to qualified psychiatrists in certain areas.
The guidelines have loopholes for the providers. They are missing an "and" requiring that residents have negative outcomes of their behaviors in addition to the diagnosis of dementia with behaviors.
Surveyors cite the lack of sufficient time to complete all survey tasks:
Due to time contraints during the survey process as a team we may not have enough time to do a through job
I think it is a system problem in facilities, so if one is affected, you know more residients are also affected, but do not have the time to make all cases. There is a lot of verbage in the 329, and hard to get to the high points of the deficiency.
Very time consuming to evaluate during the survey, considering all of the otehr tasks that are required
None of the proferred, but rather too short survey timeframe and too many other tasks to accomplish as well.
Due to time contraints during the survey process as a team we may not have enough time to do a through job
F 329 is an entire survey on its own. With all the other triggered areas and tasks that are required to be investigated for each survey, it is difficult to devote the time necessary to thoroughly investigate F329 the way that CMS requires. Most surveys are "pick your battle" surveys and unfortunately that leaves little time for thorough investigations.
I think it is a system problem in facilities, so if one is affected, you know more residients are also affected, but do not have the time to make all cases.
Surveyors ask for more and different training:
I feel there is a need for more detailed education with all the regulations especially F329. It is to complicated. Upon hire we went to the CMS training. That was great. However, why dont we have a education session now that we have an idea of what we are doing. We need training to keep up with our clinical skill (that we are not using).
Need better training on the "how" not the what.
i think there are issues when we should be citing a G level however we are told it isn't harm and is especially hard to get a G level when there are psychological issues involed ie; decreased ambulation due to fear of falling due to being on psychotropics
Updated information could be put into place as alot of psychiatric residents now live in facilities.
Surveyors cite the downgrading of deficiencies by supervisor:
I feel we as surveyors are, especially with all the recent publicity of us being "Moody", being muzzled
Our office gerenally changes the scope/severity or the tag completely
all guidelines are subject to interpretation of local enforcement so that a problem is sometimes not viewed as a problem
In some ways it's too detailed so it's open to multiple persons' interpretations. Often the supervisor does not agree with the tag; suggests downgrading the S/S.
I believe I try to cite at the guidelines, but the regional office that I work for seems to require more and more to support a citation. It is never as simple enough as showing the facility failed to do something, our office has to fight and dig and dig to show a deficient practice while CMS says if you see a deficiency, site it, even if it is only for one resident. Not at our office.
Some Surveyors report that they never cite F329 for antipsychotic drug deficiencies:
I have never cited F329
F329 is not being cited in this area
Our TC does not let us cite things in this arena
I cannnot say I have had to cite this very often. I do believe if the State had a consultant pharmacist AND a doctor we could consult that it would be very beneficial. However, we do not have either of those.
Question 23: What would you propose to improve the consistent and accurate citing of F329 deficiencies according to CMS guidelines, with appropriate scope and severity?
Surveyors offered a number of recommendations for improving the consistency and accuracy of F329 deficiency citations.
The most common recommendation is that CMS revise guidance for surveyors. Most Surveyors recommend that the guidance be shortened or streamlined, although some ask for more detail:
Streamline the information to include the most commonly found problematic medications in the current LTC community. Eliminate extensive reading of one tag that exhausts too much onsite time.
Simplify guidelines, there is so much information in the guidance to surveyors related to antipsychotics use it is becomes confusing.
short consise guidance
Take out the subjectivity of citing this tag with regard to antipsychotic drug use. The facility either did or did not do what was needed to ensure the unnecessary antipsychotic was given, ie., appropriate DX for use of drug, they either did or did not conduct a GDR. Another idea is to only cite unnecessary antipsychotic under F222.
Shorter, simpler guidelines would be nice
The protocol could be more specific and broader.
there is still a wide variation in how each facility monitors their residents for the use of psychtropic medications. I think more uniform guidelines for psychotropic medications would be helpful. (ie Some facilities do AIMS testing while others do not and some facilities do monthly IDT meetings to review all residents who are recieving psychtropic medications to assess their need for continued use and others do not use such a formal process).
Make it short,specific and clearly defined.
Simplify guidance and the pathway.
Simple, direct guidelines for the investigation process and simple direct guide lines to the scope and severity determination.
The more simple this can be made the better.
shorter less wordy guidelines. also would like guidelines on how gradual; an attempted dose reduction should go. it seems they could taper REAL SLOW and they might would have a better chance of tapering. They go to the hospital and come back on everything the facility was trying to get them off ot. If they go to a psych hospital they really order the drugs and can't understand why the facility does not want to take them back. there are no examples about this in the guidelines. The guidelines seem to think that nursin homes are utopian.
what every surveyor would consider a universe, what the census is, what the stage 2 sample is
The guidelines could be black & white. There are gray areas, which can and are looked at differently depending who is reading the guidelines.
Require Physician and Pharmacy interveiws as well as assessment of facilty practice / policy.
Remove the subjective or inerpretive components; can be too easily manipulated and then residents are thrown out of the F329 tag by field office supervisor/or central office.
In particular, Surveyors ask for more specific guidance on scope or severity or both:
More detail of what the surveyor is to look for and clear guidance on scope and severity. Right now the Regional CMS office and the FOSS surveyors don't agree on scope and severity.
more specific definitions or examples of harm
clearer defined area of harm
More clarity on pattern and wide spread definitions
Examples supporting the actual harm level and negative outcome
I think that it needs to be clearly defined that surveyors need to look at the number of residents with negative findings. If it is an isolated number of residents then it would remain isolated. However, if it is the majority of residents on antipsychotic drugs then it would be a pattern.
More examples of well written violations that have survived the appeals process. We all want to be successful in defending the resident's rights to be free of unnecessary drugs, we need to know what facts to gather to be irrefutable.
Perhaps more examples of correct citing for various scenarios.
examples including scope and severity
Simple, direct guidelines for the investigation process and simple direct guide lines to the scope and severity determination.
Providing more examples under the different scope and severity levels may be beneficial.
it is difficult to prove harm from the resident's medications.
Continued clarifications, information on scopes and severities that were accurate or that did not meet the guidelines (from CMS)
Most F329 cites are either level 4 or level 2. Its hard to prove harm with F329. Was it the drug that cause the issues or was it disease? Ones that are usually IJ are warfarin, insulin etc where there is a direct timing correlation showing it was the drug that caused the harm.
Examples of what CMS would consider to be IJ/harm/potential for harm for deficiencies r/t antipsychotic drug use.
Clearly and concisely define pattern and widespread. Include multiple examples of each to make it clear for each case we review. Use clear language in the F tag. Define words like "excessive" and put the definition in the regulation not the interpretive guidelines.
more detailed guidelines regarding what scope and severity should be used in certain situations
Provide additional examples of Level II, III and IV citations.
Many surveyors request a checklist, a decision tree, or other type of clearer, more explicit protocol:
Have a protocol of what to look for and all the requirements of the GDR's for medications outlined in one area of the regulations, like a box.
Condense F329 to core functions for the surveyor to address. List them succinctly. (i.e., steps needed to determine
whether a concern exists that needs further investigation) Then provide the other information under the tag (which is all good information) for the surveyors' further consideration and investigation if a concern is found.
detailed protocol
A decision making tree would be helpful.
CMS revamps the QIS process to make it easier, quicker and more efficient
a bullit point list
Develop a chart of specific deficient practices with the criteria, and then when it would move up as far as severity goes.
Definite help would be a grid which shows steps that need to be taken. all too many times the interpretive guidelines are cumbersome and don't give a good systematic approach.
A detailed investigatory guideline
Maybe a quick step by step outline of what should be reviewed.
More specific information…a way to be more consistent is to give specific examples.
Additional guidance and a specific protocol on pychotropic medications.
A number of recommendations address surveyor training, including continuing education:
Trainings. Not just training on a computer screen but actual face to face training where we could ask questions, provided actual problems we have encountered etc. Not our supervisor. Actual CMS employees. Considering restructuring FOS surveys. Instead of waiting until the end wrap up with a "gottcha" approach. Maybe taking time during the survey to teach/guide. Opportunities for questions during the survey.
Training. Clear explanations of the requirement.
Everyone being on the same page with their understanding of medications and their uses. Additional training of all of the surveyors for consistency purposes.
more training for surveyors
Periodic continuing education or review with specific case studies and why the determination was appropriate or not.
training to get all field offices on the same page.
The new trainig films has been helpful. But more training on side affect of specific medicaitons would be great. I have been researching on my own becasue I have been seeing side affect of psy. meds. But would love more training.
More specific inservice on F 329 not just insevice on antipsychotic meds. We know they are being used even with black box label. When is use acceptable when all documentation is in place and rationale present in record. I do not cite when based on observation , interviews and record review a rationale is in place
Additional training by pharmacists
More training from CMS regarding how to cite the tag. Flow charts for if different situations.
Provide periodic and updated training other than computer generated.
Additional training for the newer team members- retraining with the older team members. I just do not see this as a "focus" area of our team.
Provide specific training for this tag, as it is very important\ Assure that the CMS trained surveyors are provided the support by their program managers and the time necessary to do more than a superficial job
Continuing education to surveyors regarding current recommendations for use of all psychoactive medications.
provide education and proactice exercises to survey staff to ensure understanding of the tag and its processes
continued education and encouragment from CMS
Training that is more specific to antipsyc meds, for non medical surveyors.
give states more specific training to those who are not up to date on medicaitons
Stronger guidelines related to physician involvement. More education specific to medication/terminology for surveyors who are not nurses.
The use of a pharmacist on survey. Further training for surveyors.
Provide ongoing training with examples of deficient practice at the State and Federal levels.
More trainings on what other field offices are finding and citing in nursing homes and knowledge of any IDR's that are granted.
Proper inservicing, one person from each office receives a training from a CMS person and then the training is shared with their coworkers. Webinars leave too much open for interpretation and then you find different offices doing different things to meet compliance.
provide training to surveyors and enforcement at the same time — from CMS trainers
Web based training, TA from RO's rather than the usual punative approach
CMS should offer inservicing to all states so that we all follow the same protocols.
Perhaps shorter, concise matrix with definitions. Some additional training would help. more training of the tag information– web based or short inservices that can be held at the office several times in one day.
Training video on CMS web site with CMS Team going through examples of situations that surveyors might encounter and how CMS Team handled (interviews, observations, record reviews), start to finish.
review quidelines periodcally and when cited send out to new employees 2 years and under.
More training on how to cite it, concrete information on what to look at , not merely suggestions.
further education to surveyors on current drug information and how to investigate, using F329 probes
MORE TRAINING. I wonder how the system got the way it is. We must do it CMS' way and only theIR way but even the FOSS people disagree on what that is …OFTEN
increased training of surveyors
I would like to propose some kind of FORMAL training on how we are suppose to implement the regulations in the survey setting. We do not get any good training on how to actually perform our jobs. It would also be nice if the FOSS survey was about helping us learn how to better do our jobs, but its not. FOSS survey is all about how they can catch us doing something wrong, then tell us about it at the end of the survey. That is not helpful. I would rather see the state use the CMS money to train/update us every year and actually go to good trainings.
Updates and education concerning psyc meds, there approved use and side effects. Both surveyors and facilities need education. We get the excuse all the time from facilities that their doctors "don't want the state" to tell them how and what to prescribe".
Many Surveyors identify a need for training for others as well as for Surveyors:
EDUCATION to providers, physicians, surveyors, and supervisors!!
More information to licensed staff, especially MD's and PA's. But also to us… I think we were not given enough information from anyone CMS, DOH, etc regarding what we are expected to do… Also, this informmation is ofeten left for Nurses to do and our team usually only consists of one. Our teams either need more time in facility or more bodies in order to get a more complete evaluation, and that is not happening.
Continual education of facilities, physicians (and surveyors), and outside agenicies such as Hospice (who often have residents on caseload for extended periods) to thoroughly understand F329 and the effect of unjustified and/or excessive medications on the resident. Continual education to be more detailed with "specific" behaviors instead of terms like anxiety, aggression, anxiousness being used to document behaviors. Reevaluate the amount of direct care staff are truly needed in facilities to provide a level of care to meet the residents' needs.
simplify expectations. Provide more opportunities to providers for training by CMS of intentions of the regs & interpretive guidelines.l
Surveyors make suggestions about state management and federal oversight:
Holding state surveyors management to what is being taught at state and federal training. There are so many things that are taught during training that you realize aren't really what is going on when trying to acutally cite a deficiency or hold a facility accountable for what the regulations say.
I think every case is different so it depends on the problem. It also depends on the state and their "terms". In [State J] our bosses tell us we are just fact finders……. so they control the scope and severity usually…. we as a team may determine it to be one thing and then when all is said and done it ends up something else……. usually less of a scope and severity.
Provide specific training for this tag, as it is very important\ Assure that the CMS trained surveyors are provided the support by their program managers and the time necessary to do more than a superficial job
Remove the subjective or inerpretive components; can be too easily manipulated and then residents are thrown out of the F329 tag by field office supervisor/or central office.
I think the CMS guidelines/Federal surveyors are not consistent with what the State Agency must follow. As a state surveyor we have to have more evidence to support our deficiency writing. State Agencies are more likely to have citations IDR.
MORE TRAINING. I wonder how the system got the way it is. We must do it CMS' way and only theIR way but even the FOSS people disagree on what that is …OFTEN
A better consistency between what the CMS surveyors can do and what the state surveyors have to prove and go through to cite/write a deficiency
Some Surveyors discuss the inherent complexity of antipsychotic drug prescribing:
Deficiencies related to F 329 are extremely subjective in many cases. The drugs themselves have side effects and adverse reactions which are expected with the use of the medications. To determine whether or not the resident is actually being helped by the medication or not is based on the residents beliefs and many times they are unable to accurately evaluate the benefits of care
I think F329 should be rewritten to address truly "unnecessary" drugs. The tag name implies that if a resident is on a psychoactive medication it's "unnecessary" which isn't always the case. You also have to have an extensive knowledge of pharmaceutical knowledge to truly digest this tag. If the main concern is the overuse of antipsychotic medications for behaviors associated with dementia, then I'd rewrite it to address that concern.
Some Surveyors describe the difficulties of challenging physicians who order antipsychotic (and other) drugs:
I think the major problem is that physician's order these medications. It is very difficult for most surveyors to go against the phsyician. Of course facilities can do alot to prevent asking the physican for the order in the first place…but again, the physician usually has the last word. Most surveyors will not go against a physician's advice in order to cite F329. I think the physician's must be educated along with everyone else.
Less stringent guidelines. If the doctor feels the medication is needed, I do not think it is up to CMS to disagree. I think it is cruel that if a resident is doing well on a medication, that CMS requires dose reductions.
There is a fine line between us practicing medicine when we dictate to physicians. "We walk on egg shells sometimes. Besides, if a resident is stable and not exhibiting any problems, why should we cite the facility for not attempting to reduce the use of a med?
Physicians become very insulted by our investigation that closely involves their orders. It would improve our numbers if we were not required to obtain a physician's interview.
Although the regulatory language gives guidelines, the difficulty arises when a psychiatrist states that the resident needs to remain on a medication despite clinical documentation suggesting otherwise. Legal concerns could be precipitated if a change is made based on the guidelines and there is detrimental outcome.
We need clearer guidelines from CMS because of the large number of psych-related drugs and large number of diagnoses. The doctor will almost always back the facility in a matter relating to psych medications.
I feel that the requirements for physicians being allowed to assigned diagnosis for the use of the medications needs to be examined. Residents who did not have a psychiatric diagnosis in their past are suddenly assigned diagnosis when their congnition declines.
Surveyors cite the need for more time to conduct surveys:
More information to licensed staff, especially MD's and [STATE J]'s. But also to us… I think we were not given enough information from anyone CMS, DOH, etc regarding what we are expected to do… Also, this informmation is ofeten left for Nurses to do and our team usually only consists of one. Our teams either need more time in facility or more bodies in order to get a more complete evaluation, and that is not happening.
Provide specific training for this tag, as it is very important\ Assure that the CMS trained surveyors are provided the support by their program managers and the time necessary to do more than a superficial job
Having the ability to spend more time focusing on 329 investigation during the survey process. Currently time is a factor.
Decrease the number of residents reviewed by a given surveyor
Increase the team size. Four individuals can not thoroughly do an effecient survey especially with this tag.
more survey time.
Honestly, we are asked to look at a large amount of material during a survey. We are given three days and the minimum number of surveyors while the survey tasks continue to expand. Our team sizes are smaller, we have a large turn over in staff that seems to be increasing. It takes a lot of time to train someone to do this job. Retention of employees would help. Also, time for training and accessibility to resources would help (i.e. a doctor and consultant pharmacist). Facility education with the mandatory participation of their medical director would also help.
Several surveyors recommend breaking F329 into several tags:
F329 is very detailed. I believe it would be easier to use if it was broken into different tags.
Some Surveyors report the appropriate use of antipsychotic drugs in some instances:
at what point can GDRs no longer be expected— not to cause harm to the resident and increase in negative behavior when the med is decreased. If the resident is stable on the meds—- med reviews are done—behavior monitoring is done—- psych C+T done—- the med should be left alone
i believe medications are necessary in some cases– i do not believe as a rule homes are deficient in antipsychotic use
Give the benifit of the doubt to facilitys who have good record related to psyc meds and not slam them with harm when there was no negative outcome to anyone.
Question 24: Is the assignment of scope and severity made by members of the survey team together?

Question 25: If you answered “no” or “sometimes” to question #24, above, does the team defer to the surveyor who conducted the observation/interview/record review who identified the deficiency?

Question 26: If you answered “no” to question #25, above, how is the assignment of scope and severity made?
When the determination is made by neither the team nor the individual surveyor, Surveyors frequently report that the supervisor/program manager makes the final assignment of scope and severity:
We all discuss what deficiencies we think we have and why. Once we determine what we think is wrong, we then discuss how "bad" it is or isn't. Maybe we saw one instance of bad peri care, but over all the peri care has been very efficient. We discuss this and come up with what we see the scope and severity is. Once we return to the office, our supervisor looks at that and if he/she feels it needs to be changed, he/she changes it.
In practice, the surveyor(s) who identified the deficient practice tells the team during decision-making the severity of the deficiency, who it affected, and who it could affect. The team then decides the scope and severity or the individual surveyor tells the team what he/she thinks the s/s is and the team corroborates. Sometimes the s/s changes depending on what the team decides. The proposed deficiency and s/s are then discussed with and approved by the program manager before the exit.
Enforcement
Sometimes with the team but often the supervisor assigns the scope/severity.
Final determination is made at supervisory level
it always goes to supervisory review
By supervisory stafaf.
In [State J] our bosses tell us we are just fact finders……. so they control the scope and severity usually…. we as a team may determine it to be one thing and then when all is said and done it ends up something else……. usually less of a scope and severity.
Final determination is made at supervisory level
See above. We usually take the more significant issues to our management. We may feel it's high level, but they may not, so we end up having to go
Discussion with lead surveyor, team, supervision and state consultants
In practice, the surveyor(s) who identified the deficient practice tells the team during decision-making the severity of the deficiency, who it affected, and who it could affect. The team then decides the scope and severity or the individual surveyor tells the team what he/she thinks the s/s is and the team corroborates. Sometimes the s/s changes depending on what the team decides. The proposed deficiency and s/s are then discussed with and approved by the program manager before the exit.
Again, the team discusses and gives it a scope and severity, if the supervisor doesn't feel it warrants that scope and severity will lower it in many cases or central office will.
Initially by the team, but final determination made by the supervisor.
Always a team consensus and, if needed, supervisory consultation.
Sometimes with the team but often the supervisor assigns the scope/severity.
During supervisory review – always.
We gather the information, the supervisors would determine the scope and severity. We could put our thoughts, but it would ultimately be the supervisor's decision.
Civil discourse, manipulation and exhaustion.
discussion with lead surveyor, team, supervision and state consultants
It is determined by the team and sometimes with assistance from the PSA
Question 27: When assigning scope to antipsychotic drug F329 deficiencies, do you (please check all that are relevant) and identified several factors used to assign scope to antipsychotic drug deficiencies.

Question 28: When assigning severity levels to antipsychotic drug F329 deficiencies, please indicate when you/your team cite at “no-harm” level (D, E, F), “harm” level (G, H, I), or ‘immediate jeopardy” level (J, K, L). (Check only one, the one that most often applies) and then identified a number of factors and asked whether, for each of them, Surveyors cited harm, no harm, jeopardy, or never cited. 354 Surveyors responded to this question as follows:

Question 29: Add any details or comments you have for the items from question #28, above:
Question 29 contains several subparts asking how Surveyors evaluate certain factors in assigning severity levels. Question 29 allows Surveyors to elaborate on their yes/no responses to Question 28.
A) [How Surveyors evaluate severity] If antipsychotic drugs are prescribed for wandering, yelling out, agitation, resisting care, or similar behaviors:
This might be a D all depends might be Harm or greater – have to look at details.
Inadequate amount of information. May not be harm to one person but may be to another
More investigation, how are these behaviors related to the resident's overall dxs.
It would depend on the circumstances.
depends on the specific circumstances
Some surveyors indicate that some injury to the resident would need to be shown before they would cite harm:
Would have to see negative outcome to cite
No harm unless there is injury.
was the resident acutally harmed, or is this just poor practice/care
Would site harm if had falls, or other adverse effects
Other surveyors do not cite the practice of using antipsychotic drugs under these circumstances as a deficiency if the facility has tried other interventions first:
not cited if the facility provides evidence of monitoring the behaviors and policy is followed
need more details is were other interventions tried first
Determine if other interventions used. Determine effect of behaviors on the resident.
look for quantative analysis of behaviors and other inteventions tried
Have other interventions been attempted.
depends on the outcome and whether other interventions were tried
Were other interventions attempted before drugs.
have they tried non-drug interventions?
CHECK TO SEE IF OTHWR METHODS HAVE BEEN ATTEMPTED TO ALLEVIATE THESE BEHAVIORS
Some Surveyors report that they might identify a harm or jeopardy level deficiency:
Yes if used just for safe wandering, non-problematic yelling or agitation. However, feel resisting care is justified.
This plus other findings could result in a Harm level or greater deficiency
could be harm if other factors in place
would be harm as chemical restraint, possible jepardy
Harm if the investigation shows actual harm and IJ if harm not acted upon
If this is resulting in harming the resident and the facility is doing nothing to rectify the situation, then it would be IJ
we look at pharmacy recommendations and psych notes and effect of meds
It depends on the presence of a dx, consult reccomendations etc. If only for these behaviors alone, then there is a problem which could result in a citation
Depends on the impact to the resident. If negative outcomes were present, we'd cite at a higher level. If the facility has a system but maybe they aren't following it the way they should, we would probably cite it at no harm, but again it would depend on the impact to the resident.
Could be IJ if serious harm is identified as a result
Some Surveyors identify a resident’s wandering, yelling out, agitation, resisting care, or similar behaviors as a common reason for the use of antipsychotic drugs:
It is done all the time. The poor nurses on 3-11 or 11-7 can't watch all these screaming residnets–there is very little staff
This is often the facility's excuse for the use of AP
medication used essentially to control behaviors that are detrimented to resident health
Some Surveyors see no harm or require other factors before citing harm:
The residents can wear themselves out pacing and many times will not be deterred from this behavior. This is not always a wrong thing or causes harm.
All of the above answers are dependent on how many residents are involved, could it harm others, how many, the extent of the outcome, etc. Difficult to answer in a what if situation.
depends on monitoring, reduction, other interventions
depends on severity of behaviors/non pharm. interventions
cited as no harm
if the med stopped the behavior – if it worked we probably wouldn't cite
are these behaviors impacting the residents life
in and of itself no harm has been demonstrated
f it is restricting a residents quality of life.
B) [How Surveyors evaluate severity] If the facility fails to monitor for side effects of antipsychotic drugs
Surveyors generally do not cite a harm-level deficiency unless the facility has documented side effects:
No harm unless documented side effects causes harm.
was the resident acutally displaying side effects or any documentation of side effects
Given the extensive medication regime of most LTC residents, I feel inadequate to attribute a symptom that could be from a medical diagnosis or another unrelated medication to one specific antipsychotic medication.
It all depends on if there are any side effects observed for any residents
Will cite at harm if the resident is having side effects from meds an is not being monitored.
also failure to assess
depends on outcome
we have to check for a negative outcome and see if it is a system problem
If no resident outcome, cited at no harm
a sig wt loss may not be related to psych meds
depends of if side effects are observed, then may be harm
potential for long term or permanent side effects due to lack of monitoring
Depending on individual could be no harm, harm or jeopardy
depends on the outcome as to whether there was actual harm or the potential
It would depend on the circumstances and whether they experience side effects.
Would site harm if had falls, or other adverse effects
would depend on observations and reveiw of the record as to what severity
This would be harm if the resident develops side effects that were not present on admission
See A above. If the resident is showing TD symptoms or other negative outcomes related to the use of such medications, we'd likely cite a higher level of severity, but it would depend on the outcome of the investigation.
the nurses may care plan for side effect–but they really do not pay attention–
Harm if the investigation shows actual harm and IJ if harm not acted upon
Look at the resident to see if there are any side effects noticable and interview the nurses and direct care staff about any changes in the resident.
Not unless there is a problem.
not always cited if on staff interview can determine resident was monitored
may be harm if side effects emerge and are not identified
depends on the details. If they failed to monitor and we determined resident's where continuing to receive the drug in the presence of adverse SE it could be harm.
if there are SE present and facility doesn't notice it is worse
Could be IJ if serious harm is identified as a result
If they are aware of the side effects and there are no adverse outcomes to the resident I would not consider it harm.
al of these below are subject to harm or jeopardy depending on resident response, # of res. involved, staff in response, system failure
with a negative outcome, at a harm level
can be harm if resident noted a decline in health contributed to the medication usage
If the side effects are disruptive to the resident's ADL's
C) [How Surveyors evaluate severity] If a resident(s) is (are) given an excessive dosage of an antipsychotic drug
Surveyors again report that they are unlikely to cite a harm-level deficiency unless harm is documented:
No harm unless harm is documented.
again to what consequence,
if o justification, no appro. diagnosis if negative outcome, than harm noted
This plus other findings could result in a Harm level or greater deficiency
could be lethal , for example, neuroleptic malignant syndrome
based on information would be non-harm
will cite at harm level if resident has a negative outcome from the medication.
Need to determine the effect of the dose on resident – whether potential or harm
Could cause a severe adverse effect –
excessive sedation may not be related to psych med
look for md justification for doses outside the range.
This would have to affect other ADLs to cite "Harm."
More investigation, falls, loss of appetite, LOC and level of participatin in Activities.
accidental (harm) or physician ordered and documented.
if there is no "negative outcome" then it is a d level
Have to dertmine if there was a negative outcome to cite at harm.
Jeopardy–could cause death
depends on the dose given the effects that the dose has had
Would site harm if had falls, or other adverse effects
if no side effects can not show harm
I would if they were harmed by it…had a bad reaction, severe ASE
Harm if the investigation shows actual harm and IJ if harm not acted upon
This is the same for any drug.
Depends on details. How much and for how long? Was there any actual harm? Was the facilty aware of the excess? It could be severe enough to be an IJ
Could be IJ if serious harm is identified as a result
Harm would be determined based on outcome and/or likelyhood harm could occur.
Depending on the outcome it could be harm or IJ
harm level, if a negative outcome present
INTERVIEW PHARMACIST, MD, NURSE, DON , CITE FACILITY
potential for serious harm could occur or serious harm occurs
this is the potential for more than minimum harm and high risk for harm
How was this dose determined? Was it the smallest dosage able to achieve desired effects?
usually harm
Immediate Jeopardy
harm when facility failed to administer the correct dosage and noted the resident change in health and causes harm
Probably harm but we would need to see changes in resident or physician/pharmcist corroboration
Could be an IJ depending on resident outcome
in and of itself no harm has been demonstrated
If there is no clinical reason to give the max dose
D) [How Surveyors evaluate severity] If a resident(s) is (are) given more than one antipsychotic drug
Most Surveyors report that they are unlikely to cite a harm-level deficiency unless harm is documented:
It would depend on circumstances, resident outcome.
we would need to see changes in resident or physician/pharmcist corroboration
depends on assessments, care plan, follow through
Is this what is necessary to achieve desired effects? GDR?
What is impact of multiple medications on Resident
more investigation required cannot make a severity determination based on this information
Harm would be determined based on outcome and/or likelyhood harm could occur.
Won't cite as a deficiency if there is jusitfication for use of med and no negative outcome.
duplicate medications are reviewed, and interviews are done
Have to dertmine if there was a negative outcome to cite at harm.
look for md justification for use of two.
was it harming the resident?
This really depends on each individual situation and can not be answered with a blanket statement of always being cited at a set level.
Some Surveyors report that polypharmacy is common and may be clinically appropriate:
many residents are on more than one psychotropic
That what the MD ordered–Who are you to question
could be harm, but MD still could use 2 in some circumstances but MD should document rationale
dual use of antipsychotic medications are acceptable if being monitor appropriately by the facilty, physican and pharmacy . Possible one medication is appropriate and attempted
Sometimes more than one is needed. I would leave the discretion up to the psychiatrist and pharmacist.
common practice-if appropriate diagnosis may be ok with GDR in place
May be clinically appropriate
depends, sometimes this is indicated
frequent occurence, no concern if documented reasoning and monitoring
more than 1 drug may be needed. resident needs to be assessed and followed
each individual is investigated. some drugs given together for better outconme
Sometimes combinations of other durgs work symbiotically.
This is pretty typical and increases the risk of side effects.
the use of the Texas algorythymn allows this leeway to prescribers, psychosis is very indiviualized and each med acts differently depending on what neurotransmitters are affected
A smaller number of Surveyors express more concern about polypharmacy and the need for further investigation:
does the psychiatrist validate the use of a second antipsychotic
Check for interaction,pharmacy review and residents condition.
needs to be monitored, may not be necessary
This should be cited possible higher level harder to prove
This plus other findings could result in a Harm level or greater deficiency
Why are they receiving poly pharmacy
this would take further evaluation related to the resident's well being and clinical condition
if not assessed would cite
duplicate therapy caould cause harm
Potential for harm has increased without significant justification
Would site harm if had falls, or other adverse effects
E) [How Surveyors evaluate severity] If a resident(s) stops participating in normal activities
Some Surveyors report that they are unlikely to cite a harm-level deficiency unless harm is specifically documented:
more investigation required cannot make a severity determination based on this information
it would depend on whether this was the result of medication.
Its just there overall declining condition–no one pays attention
need more details is were other interventions tried first
This really depends on each individual situation and can not be answered with a blanket statement of always being cited at a set level.
Some Surveyors question whether there is another cause of the resident’s declining participation in activities:
may be other reasons that AP use.
Is there another cause. UTI, etc?
depends on the situation; ie: was it over time or did the behavior suddently start. were other factors involved
must determine why, may not be due to the drug. must consider disease process
this is hard to corelate to a drug
check for other causes
could have many reasons, did facility investigate
One Surveyor suggests that survey teams focus on quality of care before quality of life:
We look at them phyysically for skin breakdown, etc. Care needs looked at first.
Another Surveyor suggests that declining participation in activities is not sufficient to cite harm:
This would have to affect other ADLs to cite "Harm."
A larger number of Surveyors see harm, or the need to investigate further, in the facts presented:
If significant decline in multiple areas, could be IJ
yes – if it is clear the drug was the cause of the activities stopping
If direct link to medication use its harm
would be harm
If determined to be caused from drugs or related would be considered harm.
has caused harm
if this is causing a decrease in Quality of Life will cite at harm level.
CHECK TO SEE IF MEDICATION IS BLOCKING HER FROM PSRTICIPATING IN ACTIVITIES
If this is related to medications, then it would be harm
Unless there is a specific diagnosis explaining the sudden change, this could be a harm.
Would require more investigation
If direct correlation between change in level of participation and use of antipsychotic
Places the resident at harm and decrease quality of life.
citation and the drug was to blame
Usually a sign of excessiveness, or could be a personal preference or personality conflict..
If the facility didn't recognize the changes or didn't do anything to try to correct the issue, then we'd cite higher…and it's possible, depending on how the facilty staff responded, that any/all of these issues could result in an immediate jeopardy. It just depends on the investigation and the outcomes noted.
Harm and investgate other adverse effects
This plus other findings could result in a Harm level or greater deficiency
this is harm if the facility has not identified and remedied
if functional decline is permanent, based on the drug's side effects
could be harm, sudden change in condition.
psychosocial harm
Potential for harm has increased
may be harm due to aviodable decline in function
One Surveyor reports that survey teams do not look for decline in activities of daily living, another, that he/she will look at this issue in future surveys:
I have never seen team explore this
Have not looked at this in the past but will going forward.
F) [How Surveyors evaluate severity] If a resident(s) is (are) extremely lethargic or sleepy
Some Surveyors describe the information provided as insufficient to make a determination of harm:
more investigation required cannot make a severity determination based on this information
could be other reasons for issues. not enough information to make a determination
This really depends on each individual situation and can not be answered with a blanket statement of always being cited at a set level.
Some Surveyors ask whether the physician was notified or suggest other areas for further Surveyor investigation:
Has GDR been attempted. Was MD notified.
Look at the resident as a whole have they wondered all night and when you obs them they are exhaused, look at the MAR, observing the resident during the short time we are in the facility is not nearly long enough. Interview the family sometimes that is helpful, do not make assumptions.
REVIEW OF MEDICAL RECORDS, ORDERS, NSG NOTES, MD PROGRESS NOTES TO SEE IF RESIDENT HAS BEEN EVALUATED AND WHAT WILL BE DONE TO ERADICATE THIS LETHARIC SEDATING ISSUES
May be adverse effect – need assessment physical and chemical (labs needed)
depends on doseages and whether there was a change in doseage
Usually warrents looking into all the meds the resident is on, not just antipsychotics.
observed look for weight loss incont and decline
Some Surveyors suggest medical reasons could be causing a resident’s lethargy:
Determine if other cause apparent.
Must also look at comorbidities
could be from other issues, for example cardiac, not psychotropic.
Three Surveyors cite the difficulty of correlating a resident’s lethargy to a specific medication:
Can't determine automatically that it's the psych. med.
this is also hard to prove resulting from a drug
to show this there must be good evidence they were not sleepy before the drug and now are….this evidence is very rare.
One Surveyor does not cite harm if lethargy or sleepiness is the only negative resident outcome:
no citation, if that is only outcome
Some Surveyors identify additional facts that could suggest a harm-level deficiency:
Depends on the details. If the sole cause of the lethargy was determined to be the meds and he was never alert and active while on them it could be actual harm; it would also depend on the length of time and had the facility attempted a dose change.
This plus other findings could result in a Harm level or greater deficiency
may be harm due to avoidable declines in ADLs, weight, incontinence, and their complications)
Depends on the details. If the sole cause of the lethargy was determined to be the meds and he was never alert and active while on them it could be actual harm; it would also depend on the length of time and had the facility attempted a dose change.
Some Surveyors see, or might see, harm in the facts presented:
If direct link to medication use its harm
If determined to be caused from drugs or related would be considered harm.
If this is r/t the medication and negetively impacting the resident than cite at harm.
Red Flag
If the result of the medications that are not assessed or evaluated, it would be harm.
may represent harm
may cite harm
citation if the drug was the problem
usually harm
this is a red flag if I see a resident that is overly sedated
Harm and investgate other adverse effects
this could be psychological harm
if side effects not monitored and functions decline is permanent
Potential for harm has increased
One Surveyor suggests that antipsychotic drugs are administered to keep residents “quiet and calm:’
It happens–but they are quiet and calm
G) [How Surveyors evaluate severity] If resident(s) has (have) involuntary physical movements or extreme restlessness
Some Surveyors say that more information is needed before a determination of harm can be made:
more investigation required cannot make a severity determination based on this information
Depends on the details
Would depend if developed in facility and not present on admission
Some Surveyors describe the difficulty of attributing harm to the medication that was given by the nursing facility:
hard to prove cause and effect that while in NH this happened
Possible related to medication use EPS,make physician aware and to assess
need more information could be parkinsons or other neurologic issue
look at other diseases
may be from long term use prior to admission or from another disease process
75 % of antipsychotics started somewhere else…this could be masked harm from before and unavoidable
One Surveyor describes experience with this exact situation:
I did seee one nurse one time at one facility repost this to a MD- and the meds were d/c
One Surveyor says no harm would be cited:
no harm if monitored and resident/POA aware of side effects medication
Some Surveyors see the outcome of involuntary physical movements as unavoidable:
sometimes this is unavoidable
Some Surveyors describe the additional information that would lead them to cite a harm-level deficiency, additional investigative steps they would take, or additional questions they would ask:
Look at AIMS and behavior monitoring. If EPS sx are present and facility does not ID will cite at harm level.
Investigate the length of the drug regimen (short or long) all should be considered.
need to find out if this was a behavior prior to the medication
CHECK TO SEE IF ADDRESSED BY PHARMACIST, NURSING, & MD AND EXPLANATION
I did not mention in earlier questions but I always look at / for tardive/AIMS assessments.
Are these new? What was the facility response?
may investigate may have those movements on admission
how long have they had the symptoms?
Clinical record review will determine caustive factors and severity.
have to be assessed to reason and if resident assessed for prior to… lowest dose
How long has resident been on the drug? Have MD assessed and changed order?
Some Surveyors have not seen their survey teams connect weight loss to the use of antipsychotic drug deficiencies:
I have not seen this investigated by team members
Some Surveyors identify harm on the facts presented:
Harm especially if they haven't been monitoring for side effects
Harm if due to medication.
would be harm
If determined to be caused from drugs or related would be considered harm.
If it is caused by medications without assessment and alternatives tried, then it is harm
If this is r/t the medication and negetively impacting the resident than cite at harm.
definite side effect of AP.
Evaluated for TD?
harm, if not being addressed
harm or jeopardy
To late to change probably Tardive Dyskinesia – someone did not do their job!
should be evaluated for systems failure at facility, se's should be picked up during routine care evaluations
usually harm unless the problem is due to medication that was stopped a long time ago or the resident really needs the medication in spite of the adverse effects. That is up to the physician and must be expalined in the record
possible harm if no assessments of possible side effects
will be very concerned and look into this drug regimen
Would have to determine how long the resident had such symptoms, and would depend on the findings of the investigation. Would definitely be high level harm if the facility didn't recognize the resident was having such s/s during the use of antipsychotic medications and it was apparent they didn't act, if /when they recognized the problems.
Harm and investgate other adverse effects
haven't neede ot cit this but see E
I have not had to cite this. Severity would depend on what was attempted to reduce or eliminate meds. Side effects are a risk of these medications. Would have to look at what the risks were to the individual if not taking the meds, etc.
Harm if the investigation shows actual harm and IJ if harm not acted upon
could be harm if these symptoms are new since admitted to the facility is a factor
could be IJ if on for long time with no GDR attempted
some side effects become permanent fwhich would indicate harm
Resident is experiencing harm
may be harm if new onset, not identified and reversible
H) [How Surveyors evaluate severity] If a resident(s) experiences significant weight loss
Some Surveyors say that additional details would determine if they cite a harm-level deficiency:
Depends on the details. If it was determined that the only reason for the weight loss was the antipsychotic medication than yes it could be cited at the actual harm level.
Depends was the resident 350 lbs and once mental health helped with medication and they are normalizing did the resident go down to 200 lbs. Big difference from an 120 lb resident who dropped to 80lbs
Some Surveyors identify additional issues they would investigate before citing a deficiency:
GDR or med changes? Is something else going on
Has Nutritionist evaluated resident to determine other causes.
Look at the onset was it before or after the antipsy began. Don,t close your mind to any possibility underlying causes could be meds or an undiagnosed medical condition.
need to ensure that the diagnoses, such as cancer, is not causing the weight loss
CHECK R/DIETITICIAN RECORDS, OBSERVE MEALS, REVIE % OF WT LOSS X6MOS TO 1 YR
does it coinside with the medication
Look to see what the facility had done to decrease weight loss.
Clinical record review to determine extent or other factors.
got to look at the whole picture. could be related to something else too
Some Surveyors point out different reasons for weight loss, unrelated to antipsychotic drugs:
Could be number of things. Bad teeth, doesn't like food served, maybe a cultural thing.
Some Surveyors describe the difficulty of proving that antipsychotic drugs caused weight loss and may cite weight loss under a different tag:
This is usually hard to prove. We may cite weight loss under 325 if the weight loss is unplanned.
Would require more investigation for other causes
could be other reasons realted to progressive dementia. not enough info
usually cited under weight loss tag
Would most likely cite harm at F325 because regardless of the use of the antipsychotic, it is the facility's responsibility to identify all risk factors for weight loss and implement interventions under this tag.
difficult to ensure it is just from antipsychotic use
can't assume psych med related
One Surveyor has never seen her team cite weight loss in connection to F329:
I have never seen team tie in weight loss with this tag
Some Surveyors identify harm or the potential for harm on the facts presented:
Could be IJ
Harm especially if they haven't been monitoring impact of med on food intake
harm and needs addressed
Harm if weight loss not preventable and connected to the medication.
side effect of AP use.harm
Harm If the weight loss can be proven to be the result of the antipsychotic.
yes but needs to be documented and has to be outside normal range of weight for that residents health
and the medication has the potential adverse reaction of wt loss and it was not assessed as a potential contributing factor
Harm associated possibly with psy. meds. Some cause anorexia
could be weight loss o weight gain due to the medication. possible harm if not monitored by the facility
See above. Would definitely run the risk of IJ, etc. because this would definitely support the lack of a system and follow-up by the facility staff. Can't say we have cited 329 at an IJ level from my team.
if pernament harm occurs, such as inability to swallow, based on failure to address possible side effects, such as decreased swallowing or lethargy
if related to starting a new drug without monitoring
Could be IJ if serious harm is identified as a result
harm due to side effects of meds
I) [How Surveyors evaluate severity] If the facility fails to attempt gradual dose reduction
Some Surveyors suggest that more investigation would be necessary:
more investigation required cannot make a severity determination based on this information
may be harm depending on its effect on the resident
depends on the effects
Some Surveyors identify additional issues they would investigate:
look for MD justification of no GDR. IF many residents not seeing GDR, problems with practice of physician
Must assess resident and document reason.
look for why
I would look at the physician's rationale.
This would be dependent on the resident's current condition, has there been a decline, etc
Look to see if there is a diagnosis to warrant no drug reduction.
the doctor may refuse to gradually reduce but must have a good reason documented.
Has the facility tried a reduction in the past and failed.
look at documnted behaviors
Not given all the facts here- did the MD know it was reduced without benefit in the past?
This would usually be a lower level tag, but again, it would depend on the outcome of the investigation and the impact on the resident. If there was no GDR recommendations from the Pharm or nsg staff or if the physician didn't make his/her own decisions in this area, it would definitely be cited.
Some Surveyors say they would generally cite only the potential for harm or no harm if a facility fails to attempt GDR:
potential only
cited at no harm
Usually not harm but could be and may relate to other deficencies
unless there is a pattern and negative outcome, then harm
usually D
If no other negative outcome would not assign harm
no harm (unless sideeffects occured without intervention) would be cited
not sure I would cite harm – especially if the Resident wasn' t showing any s/sx
Surveyors look for documentation of harm:
If the resident is having an outcome from it it is harm
Would cite higher if there was evidence of harm.
Surveyors report that physicians can reject pharmacists’ recommendations for GDR:
The MD can just say NO
that is a doctor decision,
Usually Dr. justifies why not.
One Surveyor identifies the importance of GDR, in light of side effects caused by antipsychotic drugs:
Would expect the facility to recommend GDR on all residents due to the side effects
Some Surveyors see harm or jeopardy in the facts presented:
This would be cited as immediate jeopardy if there was no system /policy in place for GDR and no evidence that this was being done.
this is cited, consider how many on the sample and carry over or expand the sample.
unless the rationale for lack of dose reduction is documented by the physician in the medical record
Would site harm if had falls, or other adverse effects
Unless there is justfication for no reduction trial
If the clinical record facilitates finding the onset of the medication and its history of use.
Harm if the investigation shows actual harm and IJ if harm not acted upon
maybe….. needs to be attempted at least 2-3 times
One Surveyor cites harm only if a resident experiences permanent side effects:
no harm, unless permanent side effects
J) [How Surveyors evaluate severity] If the only deficiency is perceived as paperwork (e.g., failure to document the consultant pharmacist’s recommendation for gradual dose reduction, failure to document care plan interventions for the behaviors)
Surveyors again focus on documentation of harm:
This really depends on each individual situation and can not be answered with a blanket statement of always being cited at a set level.
Depends. Contd failure could lead to a negative outcome for a resident
Could the paperwork failure result in harm to the resident?
Look at the resident to see how they are.
Depend on resident outcome if this is no harm or harm.
Some Surveyors identify additional information they would look for, particularly related to harm:
same as above. If don't follow consultant pharmacist rec. and the resident is harmed, harm would be cited, otherwise no harm
are these things being done, only not documented
are the drugs being decreased anyway and how are they figuring that out
would need proof and interview with MD
Would site harm if had falls, or other adverse effects
Look at failure in system and impact on resident could be higher scope/severity
No harm unless the symptoms indicative of a potentially life threatening side effect is not added to the care plan, if the pharmacist fails to communicate need for GDR and the physician fails to do it
Depends if it caused an outcome. For example, the pharmacist's rec could be very important, for example, if the resident was getting a dangerous combination of medication and the facility failed to notify the MD.
Some Surveyors cite no-harm deficiencies under these circumstances:
care plan may be cited at Grid D
no harm but deficient
We've had "customer service" state training to ease up on "paper compliance" tags.. especially if there is no harm to resident.
It would be highly unlikely that we'd cite a paper tag, unless the scope was extensive. That would show a system problem. Otherwise, if the findings of the investigation showed little impact, I don't think it would fly.
Usually cited at A-B-C depending on number
cited but no harm
Some Surveyors suggest citing a deficiency under a different tag:
cite for inaccurate records if no harm came to the resident
Would not cite under 329; Could cite under 514 accuracy of records; or the care planning tag
Apply the not documented, not done standard of practice.
Have cited lack of documentation of informed consent.
One Surveyor says that facilities do not meet to discuss residents’ care:
None of these teams get together and discuss the resident. If you do interview the MD and ask why he didn't follow the recommendations–he will just syay he did not see them.
One surveyor describes the noncompliance as significant:
cited,these are very important for the residents well being. This where it starts.
K) [How Surveyors evaluate severity] If no negative residents outcomes are identified
Surveyors look for evidence of harm:
Is there a potential for a negative outcome?
Depends on particular situation and perceived outcomes
Surveyors usually cite at a no-harm level:
Usually a D, E, F level cited.
Surveyors may not cite a deficiency at all if negative resident outcomes are not identified:
If there is no negative outcome–No deficiency is to be written–that the law.
probably would not be cited
will not cite due to our sup and P.M.
usually not cited
Don't usually cite.
Some Surveyors cite a deficiency or do additional investigations:
review again to be sure
Just because there are no negative outcomes yet does not mean there won't be
Still cite the facility.
still potential for serious harm
cite anyway
Could still cite at either no harm or jeopardy
but there could be a potential for an outcome if the situation continued
Can still have a potential for harm if P&P not followed and documentation is sketchy or non existant
but they have potential and hopefully will prevent a neg outcome in the future
cited if there is paperwork compliance in more than 1 resident
still cite because of the facility failure.
As long as it has the potential for a negative outcome.
Other
Some Surveyors reiterate that additional facts determine the severity of a deficiency:
IJ determinations require harm, culpabilty, immediacy, etc.
I don't think there is any clear cut answer to the above as the scope/severity always depends on how the deficient practice affected the resident.
Many of the above scenarios are no nearly detailed enought to give a congruent answer. Many of those situation might be scoped at a harm level depending on other issues derived from investigation.
I'd just comment that without specific examples the above questions are hard to answer.
cannot say that an area is always cited as harm, no harm, or never cited — depends on situation
Some Surveyors cite tardive dyskinesia, falls, failure to implement non-pharmacological interventions, or reduced participation in activities:
clear link between the medication and the outcome: ie tardive dyskinesia
fall occured as the result of increased sedation, lethargy
possibly frequent falls with injury
Falls
non-pharmacological interventions not implemented
reduced activity participation
Some Surveyors describe state practice:
I can't recall F329 except in level 2 without doing research that I have no time for
we rarely write anything except weight loss at actual harm because we are told we can't PROVE the harm
Several of these elements must be collected by surveyor for field office/team to support a deficiency for F329
One Surveyor says the facility should provide medication, if that is what the resident’s family wants:
medical staff should concede to family's demand for the medication.
Question 30: Please specify, to the best of your recollection, the percentage of your/your team’s F329 deficiencies, during the past year, at the following levels.

Potential Barriers to Citing Antipsychotic Drug Deficiencies and Assigning Scope and Severity
Question 31: Do you experience any challenges/barriers to citing and assigning scope and severity to antipsychotic drug F329 deficiencies?

Question 32: Which of the following challenges/barriers have you experienced (check all that apply)?

Question 33: For the challenges/barriers you specified in question #32, above, please estimate, in your opinion, what percentage of F329 citations are affected, and offer any further necessary explanation. Enter “0” if you have not experienced a given problems.
Question 33 contains multiple subparts asking about challenges or barriers that Surveyors face in citing antipsychotic drug deficiencies. Question 33 allows Surveyors to elaborate on their responses to Question 32.
A) [Surveyors cite] None
One hundred eleven (111) Surveyors report None.
B) [Surveyors cite] Insufficient CMS guidance
Surveyors report that 0 – 75% of F329 citations are affected by insufficient CMS guidance.
Surveyors provide additional comments:
Not enough training on how to cite F329. We know what to look for but how to prove it is different.
Many times somethings have too little explanation
more real life examples
the guidance is unclear in some areas
Unless our citation matches exactly the CMS guidance we can't cite it
To wordy, need examples
There are times when it seems appropriate if all componets are in place risk vs benefits etc Is it ever ok to use antipsychotic meds for a demented resident with behavioral issues
C) [Surveyors cite] Unclear CMS guidance
Unclear CMS guidance affects F329 deficiencies in a range of situations – 0 – 75%.
Surveyors write:
providers need to be aware of specific examples/guidance related to F329 citations
information given-no training
There are many examples, but there is so much "legal" jargon. It should be simplified. It does not need to be so complex.
Have criteria that need to be taken into consideration to for evaluate harm ex. comorbidity ?
how much time is facility expected to spend on resident with dementia/behaviors
Different persons give different scenarios. More should be written with examples.
Need more explicit clear examples.
need to make guidance more user friendly
investigating F329 is overwhelming and takes a great amount of time during the survey process. The guidelined are exhaustive. It would help to have more goal oriented and specific guidelines to help identify a concern
There are so many new medications every day that the guidelines need to be udpated more frequently.
D) [Surveyors cite] Contradictory CMS guidance
a little
Some guidelines seem unclear and muddled and also contradict
Not always clear
Guidance if very vague making determination difficult
policies and focus variable over the years
E) [Surveyors cite] Too much CMS guidance
Even the protocol is long with duplicative interview and observation guidance
RO has too much guidance
Try to encompass to many scenarios
spend too much time reviewing the lengthly guidance to assure compliance
we forget that at times medication may be needed
to hard to explore all possibilities
not enough time to go through guidance on all surveys
this happens at times
too long just get to the point in the guidlines.
F) [Surveyors cite] State policy
Too many times people in this state want to cite F309 for issues instead of F329.
We have a state code that talks about retaining residents who are a risk to self or others. I believe sometimes this causes facilities to each fo a dug to control a behavior too soon.
at times seems to emphasis on working things out with the facility instead of citing deficiency, difficult to get true picture of when to cite, can be subjective.
change in Gov appointed a Secretary very very very nursing home friendly that stated she hated nursing home surveyors before they started the job and has stated we have too many and need to be laid off. We are being crushed by political influence of thenursing home groups.
it is harder to cite actual harm
10 Feel need to justify to supervisor why am citing
G) [Surveyors cite] Insufficient time to conduct survey
Many Surveyors comment on the insufficient amount of time they have to conduct surveys:
I feel like we are short staffed, so there is pressure to get your survey done timely – plus I think it takes a good investigation to prove harm..
We have 4 days for an annual. 3 for full investigation & staff meetings 1 to write deficiencies
Smaller facility has same number of tasks but less days and less surveyors not enough time .
CMS hs not allowed additional survey time to complete all of the new tasks they are requiring this is one of the new tasks.
teams are short staffed and not enough days to do survey due to travel tims
too few surveyors too lillt on-site time
Limited to a 40 hour week effects our ability to throughly investiagate all aspects of the survey.
too few days too few Nurse surveyors
we are pressured by the regional direct to get out with in three days…sometimes it is possible other times not, again no past or current experience in the process of survey.
time constraints can hinder review
On occassion, when there are multiple deficiencies to investigate, time can be a problem. However, we have needed to expand the amount of time spent on surveys or have gotten additional help from other surveyors.
Pushed for time.
the survey teams are pressured to conduct surveys quickly, often leaving taskes incomplete
Added time for this focus area detracts from time spent on other areas.
we are really rushed and bashed for missing artificial deadlines, too many new surveyors
30 %- need to focus on other aspects of the survey to get in done in a timely manner.
Supervisors may give us moe days on a survey but no additonal help which makes getting all the tasks done just as difficult
It takes time to look into all aspects of one resident to do a good job and when you have more sample residents and not all surveyors are looking at the same concern we need to work as a team on the same criteria.
so many things to look at. residents take so much medicine and hard to tell if they were on it prior to admission. do not have time to look at entire medical record to evalaute. mainly look for diagnosis, behaviors, if seen by psychiatrist, weight loss, falls, can and if followed by consultant pharmacist.
We are pressed for time during some surveys. Also, we don't have enough surveyors!
at times due to other tasks
residents with mutiple concerns not alsways time to fully address
Less staff available therefore time for surveys
15% I want to make sure it is a true citation…takes time
always time frames
adding specific anti psychotic number of sample is hard especially in small facilities
too rushed. not enough staffing
often times more time is needed
We are often rushed to do surveys in 3 days this is too little time to investigate anything in depth
If every task is assessed/reviewed throughly there is not enough time to investigate antipsychotic medications throughly. We are expected to complete surveys in 3 days. In the area our team surveys distance to a facility is a factor. Driving time is included into our 8 hour day and a large number of facilities are over one hour away from the office. This results in 6 hour a day surveys for three days.
I am a new surveyor and it takes more time for me to review and understand
big time
small team with heavy workload need to get survey done and move on
Difficult to do samole selection and meet all requirements with newdirective for selecting residents on AP meds. Rosters do not match QM'sYou keep CMS and the State keeping adding tasks like education and discussions with Administration on entrance etc. that takes up time and you loose almost the first day of the survey out on the units or reviewing records etc.
not sure about percentage, but the amount of surveyors assigned to the team can result in less observation time
the schedule is very tight, usually a week, sometimes all of the interviews cannot get finished
Insufficient time for the length and number observations as demonstrated on Pscyh med webinar
The entrance conference is becoming very time consuming. The process is much more involved with picking a Phase one sample that includes the anti-psychotics and a WHP, and to include interviews. Also the CMS roster does not match the guidelines and what we are looking for in Phase 1
We have a huge amount of care to evaluate on each survey withing our staffing constraints and they must be completed within 4-5 days unless immediate jepardy is identified.
this happens at times
The survey process is time intensive and to appropriately investigate takes time away from other tasks.
our surveys are 4 days only at a max. number of people don't matter
assigned complaint ivestigations in addition to standard survey tasks
H) [Surveyors cite] Too much focus on process, too little time to investigate/interview
Process sometimes gets in way of investigating.
the process is so long that it is difficult to complete everything & have enough time to focus on the needed areas. too many Unnecessary Drug reviews
It takes time to investigate an incident if something happened because of a mediation
some yes
sometimes need more time for interviews or investigation,
process is so stream lined and time consuming that surveyors have little time to survey initiate other residents and investigate .
Limited to a 40 hour week effects our ability to throughly investiagate all aspects of the survey. Especially if the survey team going in is small and the facility has many issues.
To many tasks and reviews to complete
sometimes unable to get enough time with observations and review all paper-work
Spending too much time in the clinical record, or MAR, and not doing observations.
Lots of areas to cover. Availability of physician. Interviews can be time consuming.
demand billing, closed records, QA interviews
Difficult to complete all the CE when you have many triggered areas.
Each surveyor has their own area they are investigating and when targeting psy. meds everyone has to stop and help the lead surveyor or at least should stop to help the lead surveyor.
To much time is spent filling in boxes and blanks
Some sub-tasks should be optional based on history of the facility
I think more recent staff are really focused on completing all tasks and not ralizing when to drop something and really analyzie the issue thats a problem area,
Processes take a large amount of time but is not the sole factor in our area not citing F329.
due to too many repetitive allegations to be investigated.
More time to investigate as guidance expects.
I am a new surveyor and it takes more time for me to review and understand
Through my time as a surveyor (7 years) additional tasks have been added to the survey process without the addition of more surveyors or time to complete the survey process
More time to observe behavior and non-medication interventions would help
50%; F329 is only one of numerous other care regulations that must be investigated. It is almost unbelievable that all facets of a facility from the garbage disposal to qualifications of the activities director is expected in less than a normal work week. I believe it would be beneficial to limit onsite surveys to strictly resident only centered requirements.
It takes alot of time to do all the interviews that they say we need in order to cite this. When you are also looking at other areas of concern also.
Interviews often need to be short and to the point which does not allow for time to really get to know the siutaiton. Many families and residents often ask to talk to surveyors duing the on-site survey which becomes very time consuming. Or complaints are called in and extra work is done to accomodate the complaints.
too many surveyors spend too much time on process.
One Surveyor finds no problem with the survey process:
No. This sounds more like a personal organizational issue vs. anything to do with the rules/regs.
Surveyors have special concerns about QIS:
Especially with the QIS process. It's seems all process and interviews and little investigation
I believe that the QIS
I think QIS has taken away my ability to observe more and interview more just due to the high number of residents and care areas I have to investigate from the traditional process
In QIS first two days are spent "collecting" data that yield very little useful informaiton
I) [Surveyors cite] More training needed in how to cite antipsychotic drug deficiencies
Surveyors support additional training for all surveyors (new surveyors, experienced surveyors, nurse surveyors, non-nurse surveyors):
Even the RNs are taxed when looking into this tag not all have extensive experience with antipsychotropic medications
the training i received for medications was not very specific, it was very general and did not not increase my knowledge about antipsyc meds
I received little ttraiing on the appropriate use of antipsychotics.
Many of the tenured surveyors have not received the training of the newer surveyors and are resistant to change and citing.
I am a new surveyor and it takes more time for me to review and understand
More education is always a good idea.
as new surveyor just learning how to apply the guidelines
to any one who has no experience as a nurse in long term care. they need training
The guidelines are very specific to the investigation protocol – more training is always a plus.
Surveyors would like practical training by current surveyors:
The "how to" not the tag. How do you cite a facility that has electronic documentation indicating interventions prior to medication, doctors that write no GDR dose required, and no other information.
yes, we need training by current surveyors, most of the trainers have not surveyed hands on for years very out of tounch with the process.
more training will hepl to have a clear understanding of the issue at hand.
would like more examples
Takes a lot of time to research so more training would be helpful on side affects of the different psy . medicaitons
if you see symptoms that might indicate harm, how do you prove that it is a result of antipsychotic medication use as opposed to progression of dementia or other health issues?
yes, want to see successful cites
More training is always helpful, but there should be more trainings on all the new medications that are released and in use. We should also be provided with updated drug books and guidelines on black box warnings etc.
more objectivity instead of subjectivity needed
One Surveyor recommends state-based training, while another Surveyor sees poor state staff development in this area:
We could use a refresher but just on certain points. Sometimes CMS' training are boring and use too many power point slides. The states ahould be able to submit a training outline for CMS approval in reagrds to F329 training. Once apporved, the states should implement the training.
Poor state staff development in this area
One Surveyor supports the new federal videos on antipsychotic drugs:
the new videos were helpful
J) [Surveyors cite] State supervisors reversing your decision to cite antipsychotic drug deficiency
Many Surveyors express concern about supervisors reversing their deficiencies:
I remember one instance where a team in this office wante dto cite F329 at an IJ level and it was downgraded to a D level.
some times the surveyor on the field can see/understand the concern better
To worried about taq not meeting POD and QA measures
Not too often for this tag Staff usually have clear support documentation when citing
very hard for them to understand psychological harm
This was most prevalent in past supervisors. The new ones are too new to evaluate.
told no proof or did not gather specific MDS information
They don't seem to have a good understanding and if they don't think they can argue it they throw it out
Sometimes they seek or ask for information that may not be available.
This is a big concern of mine. In addition, my current supervisor hasn't done a LTC survey since she statrted with the state agency over 10 years ago.
we give into providers easily–the resident counts
sometimes, but usually it's because we maybe don't have enough info or they don't feel the outcome was there
I included information regarding giving haldol to a resident with only dementia as a diagnoses. The supervisor asked, "what else are they suppose to use. The doctor prescribed it anyway"
not trusting the surveyor's judgement and requiring an abundance of evidence
90% most supervisors are none nursing and do not understand process
Challenging a physician ordered medication when you are not a physician.
based on amount of evidence to show problem was soley due to antipsychotics
This has happened on more than one occasion where the team felt they had the citation, and supervisors dropped F329
K) [Surveyors cite] State attorney guidance on citing antipsychotic drug deficiency
No Surveyor commented on this issue.
L) [Surveyors cite]Difficult for non-physician surveyors to challenge physician order
Interactions with physicians are a common concern of Surveyors:
Even with nurses, physicians take offense when we question them and report to higher level staff we are trying to tell them how to practice medicine
BIG TIME
Physician's get very defensive and think you are questioning their authority and knowledge
Non nurses have limited knoweledge base of medications.
argumentative physicians, challenging findings
I have no problem with this. if I identify the concern I try to the best I can to communicate with the DR.-if I need to.
A lot of times, there is fear the surveyor will cause the resident to have a break, or miss medication and cause more harm.
Many doctors refuse to discuss medication reductions or reasons with surveyors
can be challenging at times, use guidance
physicians at times feel as if they are not required to jusitify theri decisions for med choices
75% I think this is the biggest problem
yes, all the time the physicians challenge us.
most surveyors who are non nursing don't understand and focus mostly on their profession
The facility has paper work in order even if we do not " believe" what the physician wrote.
Little support given to surveyor
Some physicians don't want to reduce the medication because they do not want to be responsible when a resident decompensates
the physicians are not usually receptive to questions about why the ordered something and usually say the staff wanted it.
Physician's may resist non MD surveyors questioning their orders and authority
Physicians sometimes will not return your call or will tell you they are the physician and you are just a surveyor.
Physician's become angry any time I question their orders even when I am very tactful.
100 — a barrier does not mean we don't cite. We have to have evidence that something is wrong or done wrong.
doctors don't call you back in time when in facility
Some Surveyors believe nurses cannot challenge physician orders:
don't have a psych degree, how can a nurse challenge
MD has the extensive training–nurinsg limited
Hard to challeng a physician and that is normally the concensus of the team.
I am not a pjhysician so how am I to challeneng and tell him what to do. Thatis like an NA telling a Nurse what to do .
M) [Surveyors cite]Pressure from nursing home not to cite
Surveyors cite some pressure from nursing facilities, but suggest that it motivates them to write convincing deficiencies:
Nursing homesand associtaions are trying to convince us not to cite, they do what is required.
If it needs to be cited it will be.
not considered. Although too many opportunities are give to fix the problems after we enter
they do whine and carry on about how difficult their jobs are
nursing home opinions of the survey team can be biased by the number of deficiencies cited.
some nursing homes are resistive to surveyors by changing records of documentation/staffing/interviews
NO. If they fell to do what they supposed to do they I heave no problem citing them.
N) [Surveyors cite] pressure from other members of the survey team not to cite
Surveyors report that fellow teams members sometimes pressure them not to cite deficiencies, but the primary pressure they report comes from supervisors:
sometimes feel team is not looking at if a practice is deficient but will it get thrown out
They felt the facility gave a reasonable explaination for the use of the medication that was from a drug book but it was not meeting the criteria listed in the SOM for the use of the medicaiton. They felt that I should not cite for unnecessary use of medication.
Some times the tean creats unnecessary pressure on the surveyor. But if I have the evidence I will wright the citation and leave it upto the suppervisor.
Non-nurses frequently question nursing judgement and findings, and are hesitant to cite, stating it won't stand up in court.
Many would rather not have deficencies to write but if I feel strongly it is all mine.
Most discourage you because they have to help you look into this area. Many non-nurse surveyors put up barriers or do not help or understand.
Rare…
other team members have stated "when i'm in a nursing home I want these meds
because it is of the mind set of the survey team that the supervisor will drop the citation
O) [Surveyors cite] Concern that facility will file informal dispute resolution (IDR) or an appeal
Supervisors are particularly concerned about facility appeals:
25% per supervisiors reversing the citation
It is concerning all the time it takes to gather information and write a deficiency only to have it deleted
not the surveyors concern, but enforcement concern.
I realy do not care about IDR- I try to wight strong tag – so far it has been working.
Want everything "IDR" proof
from state supervisors
They have the right to IDR. It does not stop me from citing. It is important that my citation is well written and contains the details to support the citation.
sometimes I don't feel like the diagnoses are documented well and the physician will have additional documentation to consider
We talk about the possiblity of IDR, but we have never NOT written such a tag just because IDR might be a possibility. I think keeping that in mind helps us work this issue more thoroughly…want to have our ducks in a row when we cite it.
All the time, and it seems that we are not well supported as curveyors with these informal disputes, even when we have the documentation.
supervisors do not like IDR's and fear an IDR which plays a part in initially letting the defic be cited
because they say the do have interventions and the physician and psychiatrist say the medications are necessary
This is always a concern with certain corporations which makes interviews and finding facts essential to each case.
this is always a concern for any tag
P) [Surveyors cite] Concern that state will lose IDR or appeal
Surveyors do not want to spend time writing a deficiency, only to have it deleted in IDR or a formal appeal, although some do not think about IDR or appeal:
again, It is concerning all the time it takes to gather information and write a deficiency only to have it deleted
Do you have enoughinformation to withstand an appeal if there was one? usually not.
do not wish to spend time writing citation for IDR to throw it out
Well I try to do the best I can when I cit it. After that I do not think about IDR or any other process
Surveyors report that supervisors are the survey staff who are most concerned about IDR and appeals:
Department does not want to "look bad"
from state supervisors
our regional administrative staff thinks it looks bad for us to lose so they would prefer for us not to cite at all
This is always the excuse used to discourage you from writing tags.
do not want to go through the IDR and cite a deficiency when there is not solid evidence to cite.
One Surveyor reports that supervisors do not support the survey team in IDR:
not supported on IDRs, facilities produce information after the survey that did not exist during the survey
Q) [Surveyors cite] Other
Physician education for correct diagnosis is a big obstacle
we surveyors out in the field don't worry about IDR or monetary fines like ouR Program MGRs and state central office. It seems there is inconsistency and certain homes can be cited and other homes, especially corporate ones are not cited.
Some residents have serious psyche issues that facities are not able to deal with. Especially if they have a history of psyche issues.
I wish we could call our FOSS surveyors directly for guidance.
I think state agencies should have more clincal people who routinely survey reviewing these IDRs
No explanation of why enforcement deletes
State office seems to not support citing the pharmacists for their responsibilities in the process
not enough time allotted to write deficiencies at times, team members rarely cite deficiencies of any kind which taints the true S/S
Changes to Federal Requirements for Facilities and Federal Guidance for Surveyors
Question 34: Do you recommend that CMS revise the federal Requirements of Participation for nursing facilities with respect to antipsychotic drugs?

Question 35: If you answered “yes” to question #34, above, please identify the specific changes you would like to see made to the Requirements of Participation listed below. Explain why, note anticipated impact(s) on health, safety and welfare, and note efficiencies and effectiveness to be gained.
The Questionnaire identified several proposed changes to the Requirements.
A) Revise Requirements of Participation to require physicians to see residents in person before prescribing an antipsychotic drug
The overwhelming majority of Surveyors submitting additional comments support the proposal.
Many Surveyors report that physicians often rely on the reports of facility staff and do not see their patients in person before prescribing an antipsychotic drug:
sometimes physician's rely on reports from staff and do not see the residents themselves.
So many meds started when resident had bad day outbursts.
I think MD's go by what they're being TOLD happens
Too much reliance on nurses who may just want rt to stop behaviors.
Often drugs prescribed by telephone without physician seeing/evaluating resident.
Physicians just order whatever nurses request.
yes, Physicians often take facility at their word without reviewing documentation of behaviors.
Surveyors suggest that physician involvement prior to writing a prescription could provide valuable insight into medical causes for a resident’s behavior:
Needs to see the behavior – behavior may be due to something else.
the MD would see the behavior is not causing the resident harm
To see not just once. If the physician can get a better personal picture of the resident, then maybe that avenue would not be taken so easily.
This would get the physician more involved and make him/her to think about their decision and not just base the decision off of a busy nurse who doesn't have the time to deal wtih the resident. I would hope it would decrease the suage of antipsychotics.
The lack of an in-person evaluation by the physician is even more troublesome when the physician is not the resident’s primary care physician:
How can a physican prescribe AP's when they may or may not even know the resident since many are not the residents PCP prior to admission to the facility. I do not think that theyb should go on just the word of the nursing staff. as many times the nursing staff are not in tune to what may or maynot be causing the behaviors or what behaviors etc. warrant the use of the AP medication. I think all to often staff call the physican and obtain an order for an AP med because a resident is acing out because of other resons such as pain, need for toileting etc.
Some Surveyors want to tighten the requirement for physician visit by placing time limits:
This is a great requirement, but it is loosely used. If the physician sees them on day one and prescribes the medication on day 16, several things could change for the resident. The physician should see the resident within two to three days, before or after the med was ordered and note in progress note specifics to the use and need of the drug.
Surveyors are willing to recognize a limited exception in an emergency.
Surveyors express concern about the common situation where residents are admitted to facilities with prescriptions for antipsychotic drugs. Surveyors offer recommendations for this group of residents:
This may be difficult for new admissions admitted on anti-psychotics. Matbe physicians should have to see residents before changing the doses or initiating new medications. Physicians should be required to review behavior logs. (19)
most often a resident is admitted from the hospital with antipsychotic drugs. The admitting physician only reviews the orders and does not physically see the resident until their "rounds"
most come in on antipsychotics and physicians just continue use
A few Surveyors oppose the recommendation, describing it as “not practical,” “a hardship” on facilities in rural areas, and “impossible to prove.”
One Surveyor comments:
OMG, they don't already?
B) Revise Requirements of Participation to prohibit PRN antipsychotic drugs, or allow only in cases of emergency
Most Surveyors writing a comment support the recommendation, with one Surveyor suggesting that “prn antipsychotics are most likely a chemical restraint.” Some Surveyors discuss emergency situations and several Surveyors oppose the recommendation.
Surveyors supporting this recommendation describe the overuse of PRNs without trying other interventions first:
yes, primary care Drs are most times the prescribing mds. Antipsychotic meds are often prescribed as prns to control behavior when other meds or activities could be used. Meds are often the "easiest way out"
PRN medications should be given under specific guidelines by determining how the resident manifests the behaviors. Now the facilities write "for anxiety or agitation" and that is accepted.
PRN allows facility too much opportunity to use instead of trying other interventions
PRN medications are frequently given to residents without attempting behavioral interventions convenient and fast solution. They are often a duplicate of a prescribed antipsychotic medication and are often used for staff convenience and relate to shortage of staff.
Surveyors suggest that any PRN use that is permitted be carefully circumscribed:
PRN medications should be given under specific guidelines by determining how the resident manifests the behaviors. Now the facilities write "for anxiety or agitation" and that is accepted.
unless facility can provide thorough assessment of why the antipsychotic is needed with specifics not generalized behaviors
If prn needed a physician should be contacted first, not a nursing decision
Although many Surveyors support use of an “emergency” exception, one Surveyor expressed concern, “because everything will be an emergency.” Another Surveyor suggests “certain medications should not be used prn and they are.”
One Surveyor expresses concern that physicians write a diagnosis “just to get state surveyors off their backs.”
Several Surveyors oppose the recommendation, reporting that PRN antipsychotics are necessary in some cases for the health and safety of residents and that PRN use “is not a black/white issue.”
C) Require that survey agencies have pharmacists available to consult with surveyors during survey
Some Surveyors report that their State already has pharmacists available. Other Surveyors enthusiastically support the recommendation, with some going further, and recommending that pharmacists be assigned to each survey team:
Absolutely, this would be extremely helpful
Yes, I think this would be the biggest most helpful solution.
I think this would be the most important and effective approach.
This would save a great deal of time for the surveyors.
It would be beneficial to have a pharmacist on each survey team as they have so much medication knowledge and can provide the survey team with a lot of guidance.
Several Surveyors discussing the recommendation note that, at present, their only, but potentially biased, resource is the facility’s pharmacist:
We always call and discuss concerns with the facility's contracted service, they are pretty straight forward most of the time.
Would be helpful to have access to state pharmacist rather than facility's.
Would be nice to speak to an unbiased pharmacist instead of one who consults with the facility
unbiased opinion would be nice we call facility pharmacy and sure facility alerts them
Some Surveyors support the recommendation but express concern about the cost or think the proposal is not realistic:
added cost who will cover this ? new care regulations ??
nice thought wont be cost effective tho
wow, what a concept, but who can afford it?
Several Surveyors oppose the recommendation as unnecessary:
no. the prescribers do what they want
no, that would drive up the nursing facility costs and pharmacy consultants would not hire out to be confined so long at one particular facility.
not needed. would not benefit surveyors in making compliance decisions
D) Require every facility to have a Performance Improvement Project on antipsychotic drug use, as part of Quality Assurance and Performance Improvement (QAPI)[1]
Most Surveyors strongly support the recommendation to require that all facilities have PIPs addressing antipsychotic drug use. In their view, requiring facilities to focus on the issue and to identify solutions to inappropriate antipsychotic drug use in their buildings could help reduce such use:
If you make facilities look at this, they will see the problem and likely work on it
Yes, if you can get the facilities on board for the reduction and the medical director then maybe the rest of the physicians would follow suit and we would see antipsychotic usage decrease.
This would force Nursing facility to be more focused on this area
Witout a requirement or initiative very few facilities will focus on a reduction of antipsychotic medications
Yes, this would force them to look at AP use and the possible reduction, or inappropratness of the use of the medication.
would really put a spotlight on it for the facilities and hopefully help remove some residents from receiving these meds
One Surveyor recognizes Surveyors’ limited ability, under current regulations, to review facilities’ quality assurance activities:
This is fine but we are not permitted to look at their QA so we have to go by what the facilities tell us. Change the SOM/Regulation to allow us look at the QA.
Some Surveyors express skepticism about QAPI in general:
Not sure of this. Some facilities will address this the correct way others will only hire consultants which will take away money from resident care. We should be stressing common sense and individualized care.
Facilities need training first or this would be paper compliance and not result in positive change
This would be paper compliance which will not help the residents
Paper exercise
only if active3 program not just more paperwork
Two Surveyors oppose the recommendation. One suggests that development of a PIP should be “facility choice” and another comments, “Either they value QAPI or they don’t requiring this would not help.”
This would be a good practice considering the number of medications admisistered and residents affected.
would really put a spotlight on it for the facilities and hopefully help remove some residents from receiving these meds
That would be a very good idea. Facilities need to be educated further.
One surveyor did not know what the QAPI was.
E) Require mandatory staffing levels
This recommendation elicited the most impassioned responses of all the questions on the Questionnaire by many Surveyors who believe strongly in the need for improved staffing levels. They contend that higher staffing levels are critical to improving care for residents, in general, and for reducing inappropriate use of antipsychotic drugs, in particular.
I have thought this for years, especially as a DON, we have the levels for life safety codes why not for nursing? These facilities are making good money off of Medicare and therefore CMS should set mandatory staffing levels.
YES! It scares me how little staff is in facilities at night.
Residents on antipsychotic meds require closer monitoring therefore properly educated staff should be readily available and 15 to one ratio is not adequate.
Yes. There should be some kind of staffing guideline because that is the first cut for proprietary homes
Would help prevent facilities from pulling staff from sister facilities during survey time. Overall would provide better care, more consistent care to residents. Staff would have more opportunity to get to know and understand their resident needs and better able to apply non-pharmacological interventions. Also help prevent staff turnover related to burnout.
This is needed in more that is area. It would also be easier to cite this tag. Many facilities try to cut staff so low to bare minium to save money that it makes resident feel that they have to wait along time for help which impacts their psychosocial well-being.
There should be a higher mandate for direct care staff. Current staffing levels include professional staff who are often too busy with medication pass, treatments, and paperwork to be out with the residents. The staffing levels are acceptable based on the nursing staff who are not performing direct care. More direct care staff would benefit the residents in so many ways as there would be more time for each resident to receive care and services. As it is currently, direct care staff are rushed to get everyone washed, dressed, fed, taken to activities and rarely have any time left to just spend quality time with their residents.
this is really the heart of the problem. There are not enough trained staff to address the residents with advanced dementia or are agressive, frightened or for the psychiatric residents who have no where else to go. If the facility at least increased the number of trained activity staff who could engage residents ythe nursing staff could then care for sicker residents.
THIS WOULD SOLVE EVERYTHING……..THE NURSE TO RESIDENT RATIO IS WAY WAY TOO LOW FOR THEIR ACCUITY. ALSO THEY ARE REALLY SICK THESE DAYS AND THEY ARE GIVING IV'S, TRACHS, AND THEY HAVE NOT INCREASED THE STAFFING LEVEL. FACILITIES DO MUCH BETTER WITH THE RATIO BUT EACH CNA WHOULD ONLY HAVE SO MANY RESIDENTS TO CARE FOR. ONE CNA CAN NOT MANAGE 10 INCONTINENT TOTAL CARE DEMENTED RESIDENTS.
YES! When there is not enough staff to only do the bare minimal care needs of the residents then the team enters for the survey the facilites call everyone from all shifts so it appears that staff is good. The teams leave and so does the additional help. During the survey it appears there is plenty of staff. Staff will be tripping over each other to assist the residents. When the team leaves then they go back to counting administration nursing staff as hands on care staff for the residents. Direct care staff should be counted separated from the nursing staff not working at a hands with residents. CNA's should not care for more than 5-6 resident's per shift and one nurse to give medications per 25-30 residents.
Several Surveyors want to go further and to mandate staffing ratios by shift:
mandatory staffing levels should be divided to include each shift requirements
Required a nurse to resident ration of at least 1:14, 1:18, and 1:20 for day, evening and night respectively
Several Surveyors note that their state has staffing ratios but that the ratios are either too low or are considered the ceiling by facilities:
there already are Pa state mandatory staffing levels. The problem comes in when accuity levels are higher in the facility do yu put your staff with the behavior "problem"residents or with the residents who need higher levels of needed medical care?
Our state has a mandatory staffing level and we find that we cite the federal requirement more frequently as we are able to look at the acuity level of the facility and determine if the residents needs are met. This appears to be more indivudualized.
We do require minimal staffing levels on the state level however I do not think it is high wenough for the acuity of the residents being atmittwed to facililties in todays world. However, I understand the finacial pressure this would put on facilities and am unsure how they would be able to operate with increased staffing costs.
[State C] state has minimum levels, and facilities think if they staff to the minimum they're covered
A number of Surveyors express skepticism that mandating staffing ratios is an effective strategy:
sounds good but not effective More staff does not equal improved care
no, because the condition of residents depends upon the number of staffing levels that are needed
What ever level you mandate facilities will fight it or consider it a "maximum" rather than "minimum" level. They just won't staff to acuity!
they tend to staff according to mandatory levels and not to needs of resident population.
Some Surveyors support acuity-based staffing:
implement a different level of staffing, based on acutity, versus number of residents
Some Surveyors question whether increased staffing levels are affordable or realistic in the current financial climate:
We have a mandatory staffing level in Pa. but is not high enough. But soon nursing homes will not be able to afford to stay open.
how with all $$$ cutbacks coming ??
Is this realistic?
One Surveyor opposes the recommendation, finding current staffing standards sufficient.
Question 36: Do you recommend that CMS change federal guidance for surveyors for F329?

Question 37: If you answered yes to #36, above, please identify which specific changes to surveyor guidance you would like CMS to make (please explain why, note anticipated impact(s) on health, safety and welfare, and note efficiencies and effectiveness to be gained):
Follow-up questions asked Surveyors’ opinions of specific revisions to federal surveyor guidance. By overwhelming majorities, Surveyors support all of the proposed changes and also offer some additional suggestions.
A) Require all state survey agencies/CMS have a pharmacist available to consult with surveyors during surveys
Most Surveyors responding to this recommendation are supportive. A few Surveyors report that their states already have pharmacists serving in this capacity, while several others think the recommendation is impractical, unrealistic, not needed, or that there is no money in the state budget to hire such a person. Several Surveyors indicate that a state pharmacist would be preferable to their current practice of relying on the facility’s pharmacist:
Would be helpful rather than facility's pharmacist who could compromise.
Would like an independent pharmacist instead of the facility consultant
B) Re-establish a separate F-tag for antipsychotic drugs (i.e., unbundle antipsychotics from F329, unnecessary drugs)
More than 100 surveyors support re-establishing a separate F-tag for antipsychotic drugs. They suggest that a separate tag would add specificity, clarity, efficiency, and focus. In addition, Surveyors suggest:
It was easier when we had F330 but the same requirements are actually there.
I find myself investigating the other drugs less than I used to before antipsychotics were bundled in with F329.
Yes. This tag can be cited for a lot of issues. Separating the two issues listed here would be more clear.
yes because sometimes they are necessary but maybe not the appropriate choice
yes, i think this would be better, in that the antipsychotics could be a separate focus
This might simplify some of the issues involved the difficulty of citing F329.
It was easier to cite a tag specific to antipsychotic drugs – did not get lost in the mix
yes, if it is just a matter of paperwork not done but the resident benefits then it's not an unnecessary drug.
Given our population in [State J] this may be more benefical as we have a tremendous amount of former mental instution residnets in our nursing homes
This would help to better assess these medications when they are prescribed for other ureasons than what they are intended. Will provide for more effective assessment of unnecessary meds..
Yes these medications when they are prescribed for other ureasons than what they are intended. Will provide for more effective assessment of unnecessary meds..
yes, the guidelines would need to be more directed at the reason for the tag relevant to the desire to reduce meds as opposed to meds that are considered unnecessary
The review of unnecessary drugs is not as extensive a review as antipsychotic
yes – will highlight and clarify facility responsibilities. Will streamline the surveyor investigative protocols and identify when not being followed.
A small number of Surveyors do not believe unbundling is necessary:
It might help but shouldn't really matter if unnecessary what drug type.
No. Guidelines just need to be more specific
D) Provide more links to research literature on antipsychotic drugs
Some Surveyors support additional links:
That would be nice but surveyors are using personal cell phones to get info while on surveys on the internet.
Yes. Provide reference manuals to state survey offices
yes in leiu if mandatory pharmacist
yes to provide extra guidance and to incorporate into the tag writing
Any resource is valuable especially when it comes to drugs and the elderly
new drugs are being utilized and we are not familiar with them
This would be helpful for references on the ineffectivness of the commonly used seroquel and risperdal
Yes, related to research which would be used as ENFORCEABLE references to cite deficiencies related to unnecessary drugs.
Would definitly provide education to surveyors who are not nurses and would increase our knowledge thus helping us to be more effective in our evaluation of these meds.
Make more information more easily accessible
Surveyors need more how to apply and cliff notes of the research….don't have time to evaluate the research
Would assist with knowing what CMS considers "official".
Some Surveyors report that they do not have the time to read the research literature they already have:
No. Never realized that is what those references were for. Never used them.
and make it more confusing than it already is?
literature is great but no time during business hrs to read the literature
Don't have enough time in the office to read what is already in system
We are not provided internet access when out of the field office. Also, research literature is not regulation.
E) Reduce and simplify surveyor guidance in the State Operations Manual
Many Surveyors strongly support reducing and simplifying surveyor guidance. Virtually no surveyors oppose the proposal.
Please. Stream line obseration,interviews and record reviews. The protocol is 13.5 pages long. Again remember size it for field use not text book
Give more information regarding how to cite not more resaons to why to cite.
always be specific to what the surveyor looks for and how the interpretation of the language is meant.
please please please do this. This is so freaking complicated.
This could be done by breaking it into more tags
Yes – clear and concise
I think the process is simplified but too many other folks get involved in the reviewing of the citation
simplify for easier referencing
Guidance is very vague If it were more specific all surveyors would evaluate med use effectively
simplification is always needed to be able to accomplish the task in as little time as needed
I think the guidelines are often vaque and make it difficult to back a citation. They are also very cumbersome in the current state in requard to being able to review or pick out a deficiant practice in a short amount of time.
Carving out a specific section for antipsychotic use in dementia would be helpful
This would be helpful in gaining clarification to the guidance to properly cite
simple and direct with practical examples
F-329 is a lengthly tag and reading through all the guidance can be very time consuming depending on the issue.
F) Specify that a facility must be cited with, at a minimum, a harm-level deficiency when
Question 37 identified five specific situations. Some Surveyors responded to the preliminary part of the question, presumably answering whether any situation should leave to automatic harm-level deficiencies. Surveyors who support the proposal recognize that it would lead to “better consistency” and a more standardized survey and would help when their supervisors are inclined to delete the F-tag.
This would provide a black and white guidance for better consistency.
May help for those situations that supervisors drop tags.
this would be a powerful motivator since it would drasticaly impact their 5 star raiting
definitely would standardize the survey
yes, this would help surveyors have backing to wirte the deficieny
yes, cms expectations would be helpful to us as well as the facilities would be less likely to argue/IDR
we would certainly cite Harm more often
It would force the facilities that are not conducting thorough review of antipsychotics and establishing a system to evaluate resident behaviors
If the facilities knew this could happen, there would probably be less use of drugs. However, documentation can be written to justify anything a facility does but it doesn't mean that what was written was fact. It is often hard for a surveyor to prove that.
Surveyors opposing the recommendation suggest that harm must be found before a deficiency can be cited:
no. there isn't always harm involved
The length of time and side effects should be the main criteria for harm or potential for harm..
no- if the resident is not experiencing a negative effect, requiring this level of citation seems inappropriate. Citing a level 2 seems to be more appropriate- it identifies an issue and requires a plan of correction.
I would not be in objection but I theorize that written content to deficiencies will be deleted to lessen the level
no there needs to be flexiblity
no need to eval case by case
No, there is deificent practice but not always harm present. But, I dont' see how this could be cited at a A, B, or C level ever.
you'd have to prove that harm occured
No. We need to look at each individual resident/situation.
The Questionnaire identifies five specific situations and asks whether a harm-level deficiency should be automatically cited. Fewer Surveyors support each of the specific examples. Excluding those Surveyors who said the automatic citing of harm-level deficiencies should never occur, Surveyors respond to the five situations as follows:
1) [Should harm be automatically cited when] A facility gives an antipsychotic drug to resident who does not have a documented history of psychosis
By a three-to-one margin (33-11), Surveyors support the proposal to cite a harm-level deficiency under these circumstances.
yes this would help surveyors have backing to write the deficiency
The physician should explain the purpose for the medication not just with a diagnosis or symptom.
yes, this should not be allowed, but falls back under the category of not wanting to stand up to the physician
if there is no pschosis why is the drug necessary
Surveyors opposing the proposal cite physician prescribing practices and the need to show harm to the resident:
No. If the physician wants it it's not for us to argue.
No, still need to assess that there was harm
This may prompt unwarrented dx
But has an MD order that is a problem for the surveyor
this is what complicates it because some drugs cs be used for other diagnoses
2) [Should harm be automatically cited when] A facility gives a resident an antipsychotic drug without first evaluating whether there is a medical or physical or environmental cause of the resident’s “behavior”
Many Surveyors (52-9) identify the importance of evaluating a resident before using drugs:
This should be the first thing that should be done is to assess if a medical, physical or environmental cause is the reason for the behavior
the facility needs to determine if there is an underlying cause for the behaviors
Yes, they need to evaluate first not medicate first.
Alternatives should be considered prior to prescribing antipsychotics as long as the resident or others are not placed at risk.
would cause nursing facility to be accountable
yes cite if no proper eval was done
yes, there should be minimum specific assessment requirements to guide the facility
Yes, otherwise facilities will not reduce antipsychotic medications without consequences.
Other Surveyors identify physician orders as a barrier and the need to see harm before citing a deficiency:
this is a prescriber issue. The facility follows orders
not always a harm
Only if there was a medical condition that ws missed
3) [Should harm be automatically cited when] A facility gives a resident an antipsychotic drug but does not monitor for side effects
Surveyors supporting the recommendation (44 yes, 10 no) believe the proposal would establish facility accountability for failure to monitor for side effects; opponents cite physician orders and the need for harm to be found. A couple of Surveyors identify facilities’ practice of documentation by exception.
Many medication aides and nurses know what the side effects are. Some of the side effects include weight loss, agitation, insomnia, etc. are not known by non-nurse surveyors. If these are listed we all would be more efficient in our assessments. Many of these meds in combination with other medications can be a problem for some residents who do not have psychiatric conditions. Being senile does not constiture psychotic!
This is deficient practice but many times will say they chart by exception.
Due to the amount of side effects from other drugs that may or may not produce the same side effect this would be difficult to say which drug actually may have cause the side effect
Yes, they need monitor for side effects. Most the time they document by exception so there is no follow through for monitoring unless the facility uses a Behavior Monitoring Sheet.
4) [Should harm be automatically cited when] A facility does not try gradual dose reduction for a resident who is appropriately receiving an antipsychotic drug
Some Surveyors identify the importance of monitoring drugs and support this recommendation (34 yes, 14 no, 11 maybe).
The resident may not maintain his/her highest level of functioning and/or quality of life if effects of medications are not closely monitored.
Many medication aides and nurses know what the side effects are. Some of the side effects include weight loss, agitation, insomnia, etc. are not known by non-nurse surveyors. If these are listed we all would be more efficient in our assessments. Many of these meds in combination with other medications can be a problem for some residents who do not have psychiatric conditions. Being senile does not constiture psychotic!
otherwise facilities will not reduce antipsychotic medications without consequences
Too many physician's saying that residents "are stable so no change at this time.
Yes-especially as a resident overall health declines, some medications are just not necessary anymore. But a med like Depressive medications, should be looked at further before discontinueing it.
yes, at least once and if no adverse effect must continue to lowest dose possible one failure of GDR does not mean the facility does not try again!
yes and a needed explanation from the physician/behavioral management physician as to why there should not be a reduction.
Surveyors identify a barrier when facilities document by exception:
Yes, they need monitor for side effects. Most the time they document by exception so there is no follow through for monitoring unless the facility uses a Behavior Monitoring Sheet.
This is deficient practice but many times will say they chart by exception.
Other Surveyors point to the need to identify a negative resident outcome, the difficulty of attributing the negative outcome to the antipsychotic drug, and no need for gradual dose reduction when prior attempts have failed or the drug is “working” for the resident:
Only if the resident has outcome in this case.
No unless the resident is showing outcome-lethary etc.
no-if documented reason why no GDR appropriate
Without a negative outcome to the resident?
If side effects were missed
The facilities depend on the pharmacist for this to be recommended and many times the pharmacist does not even assess or knows the resident. The pharmaciest should indicate why dose reduction should be recommended.
Due to the amount of side effects from other drugs that may or may not produce the same side effect this would be difficult to say which drug actually may have cause the side effect
The physician may not want the GDR which is up to him/her
sometimes if results are positive then GDR could be negative
No, not if there is documentation as to why a doese reduction was not attempted.
Sometimes it is not good to require a reduction in a medication when previous reduction attempts were not successful. At least that's what psych physicians are saying where I survey.
WAS IT COMMUNICATED TO PHYSICIAN AND DID THE PHYSICIAN GIVE GOOD REASON FOR NOT DECREASEING IT
more info needed if the resident is doing well on the medication and no side effects noted it seems to be working
Surveyors offer additional comments and recommendations. Some Surveyors reiterate the need to see evidence of harm. Others are concerned about the increasing number of residents in nursing facilities who have behavioral health issues:
nothing should be an automatic harm level that should be left up to team
Again, scope and severity is always resident specific.
Each area above would require evaluation to determine harm
need guidelines for our younger behavioral health SNF facilities. This includes all our regulations due to psychiatric diagnoses. Many of our homes have these residents now since Dept. of Mental Health stopped services.
Require residents to see a psychiatrist prior to odering the medications
I find it amazing that for a subject deemed this critical to have additional surveys and trainings, CMS saw fit to remove this percentage from the QI/QMs and CMS-802 form. Now, the survey team is delayed while waiting for the "end-of-tour" list (almost laughable) to select Phase I residents, when, these residents could have already been incorporated in to the off-site sample. And, now, the surveyor must use one of the end columns to identify this focus area that is supposed to be reviewed on EVERY survey??? This is the most fragmented way to review one focus area.
get makers of behavior monitoring sheets to make them more user-friendly and not so subjective
is it a little soon to use a "bigger stick" method of change? Could we not wait to see if change will occur with focus on education and QAA?
It is difficult to know when a side effect started on a residnet and it may have been present prior to being started on an antipsychotic.
For DX of psychosis how will you prove that …to difficult. GDRs have a lot of history so harm is difficult for 75% that are started outside of nursing home.
more training more real training with a live person not some video where you watch it and can't ask question or clarify an answer
Additional Thoughts and Opinions on Citing Antipsychotic Drug Deficiencies
Question 38: What else should be done to enhance your ability to investigate F329 antipsychotic deficiencies, to cite them, and to assign the appropriate scope and severity? Please include suggestions, anticipated impact, and how/when to implement.
Surveyors reiterate many points made before – the need for more surveyor staff or time to complete surveys, more training, clearer, more specific guidance from CMS, clarification of surveyor focus:
More surveyor staff/more time to conduct surveys:
Sufficient surveyors on team to begin with.
More time during survey
more time. we have 2-3 days to complete a survey
More surveyors or more time being allotted during survey.
allow more time for OBSERVATION
more time on surveys
Allocate more time for a recertification survey. Our team is consistently told by our supervisor that we have more than enough time to complete the survey. The team does not feel that way. Many of us put in 12-15 hr days in ordre to do a thorough investigation when we are scheduled for 10 hrs.
Increase lenghth of survey, when excess travel is required, which shortens time onsite to adequately investigate.
More survey staff. Make it mandatory that there are a minimal number of surveyors on a team. This would force our state to hire.
More time alloted on surveys to conduct the whole survey process effectively. Especially in places where surveys are only scheduled for three days.
adjust survey in smaller facility that are only 3 days to have less tasks or more days. It does no justice to the residents or to the facility as the team rushes like crazy just to get done on time.
More training for surveyors (e.g., how to question a physician order, examples of successful deficiencies, in-person training):
Face to face training with opportunities for questions-consistency-now
Better steps on how to challenge a physician
More formal trainings
Main problem is that most surveyors will not challenge a physician's order
Provide consistent training with what really happens at the state and regional level.
Definitely more education with examples We have had education on antpsychotics not being appropriate but show us clinically how to get to a deficiency when you have psych documenting the need and improvemnets in their quality of life
More training and specific guidelines to deter IDR
More training on non-pharmacological strategies for dealing with dementia
dealing with how to handle the physician
Give us examples cited at federal level to review to see what we need
Education/seminars with up to date pharmaceutical information.
Give more suggestions, instructions how survey team can cite when facility gets by with minimal documentation.
continuous updates on new medications, their usage and side effects, and precribed dosage for elderly
Yearly training
again training with a live person from CMS and they should all be on the same page amongst themselves it is very frustrating to be told on one survey you must do or cite something one way and on the next told that is wrong VERY FRUSTRATING
more ability to question a physicians order
Training on investigative techniques
person to person direct inservicing, no webinars
Question and answer session to ensure are information is understood and clarification is offered if needed
Provide samples of how other surveyors address and investigate concerns
Further training of what is commonly missed and how we should evaluate those areas.
Institute CMS seminars out of the office and not online. Online is wasted when you are rushing just to "get things done" Maybe refresher course or advanced level surveyor courses. How about CEUs ? Our state does not even give us tuition reimbursement so education is no priority at all. Unlesss it is state related: ie computer safety, or travel vouchers.
Clearer, more specific surveyor guidance (e.g., scope and severity):
Provide more specifications for what you want citations to be based upon, most of what is suggested is very subjective in its scope
Clear Guidance from CMS regarding the requirements and CMS expectations.
more education on psyc meds, understanding the use and possible downfalls
more examples and more guidance to scope and severity
clear scope & severity guidance
A checklist to go by to see that everything was in place before initiating a psychotropic medication with time frames for ongoing evaluations to see if it is justified why the medication continued.
Clearer guidance
Create a users tool to assist surveyors in process
Need better definations for assignment of harm for 329
We need updated information on all of the newer psychotic medications and anti-anxietys and the hypnotics that are on the market
Clear consise guidelines
Clearly defined guidance as to when to cite and all associated tags to cite in addition
If there is a belief that we are under citing at "Harm" level then we need more education about what consitutes a G versus a D. Obvious is the person who developes EPS or is face down in their oatmeal and it can all be traced neatly back to the Rx of antipsychotic. A bit hard when the only issue is no diagnosis but the person is still functioning just with fewer BH. Implement sooner than later.
simplify F329 and guidance
more specific information in SOM
Scope should be based on the definition in the SOM and not based on this generalization of the "Universe".
List the common antipsychotic drugs in drop down box again
Condense the investigative protocol to be more managable
There should be clear black and white requirements under F-329.
Give very specific examples of what would constitute harm.
Make criteria for actual harm as opposed to simple procedural events
Guidance in the form of an updated manual, not by letter only outside of the manual
Provide a tool that onlines the steps we follow to evaluate this citiation. That is easy and straight forward to understand.
Maybe having an investigative outline to guide us – like a list of interview questions to ask… but I guess this is already in the CE pathway
Training on scope and severity determination of F329
more guidence in the GDR process
more guidance/links to resources for non-medical interventions – when compiled, all LTC facilities would be notified and then have access on the cms website
Decision making tree.
Clarification of surveyor responsibility:
Stop implying that surveyors are for educating facilities.
Look at state central office for inconsistencies. Otherwise our residents are at risk for substandard cares.
supervisors to be more supportive
Training supervisors:
Educate the team leaders and supervisors of the importance citing F329 as well as F222
Team members and enforcement member not be so quick to decline someone wanting to cite the tag.
Make it mandatory for the Supervisors to survey occasionally so they understand what we have to do to cite this deficiency
More training for physicians and facility staff:
Give education to physicians.
Have all disciplines educated on medications
Provide the facilities advance guidance, especially regarding the physician education of expectations.
More training for the facilities and especially the physicians as to the appropriateness of ordering an antipsychotic
More training for the facilities that includes all members of the IDC teams. I think facilities are still too quick to start psych drugs. When the facilities understand the requirements clearly and fully understand the impact of failure to follow the reqwuirements, there will be less use of psych drugs.
More education to Prescribers. If the meds are used appropriately it doesn't take much time to review them. Educate through professional organizations, journals, medical office "freebies" like the drug reps offer…
Allow us to teach (more) the care givers provide better care for the residents.
CMS needs to get experts to educate facilities. Surveyors are experts at investigating.
We can't consult with the facilities and then turn around and then cite them. They need expert consultants if they want to be in complaince with 329.
Changes in Requirements for facilities:
Require that physcians indicate a specific reason for the lack of a GDR
hold the psychiatric services accountable because the PCP always takes the recs due to not understanding antipsychotic medications
That the facilities have documentation in the active clinical record of the GDRs and the physician documentation of it not to be done.
More clearly define terms and expectations especially in the regulation itself.
make it mandatory for physician response to GDR's and cite if not done or risk/benefits explored
I would also change guidance that when admitted to the facility that GDR occurs much sooner…..current guidance could let the resident be on the drug for 9 months before one attempt is needed.
mandated reductions at certain intervals.
more specifics as to what should be done prior to tryng medicaiton
Provide guidance for residents who may have been on the medication for years, or even decades, and then find themselves having the medication changed to accommodate a regulation.
Changes in survey rules:
Having a pharmacist on the team.
simplify the CE pathway
Review of other tasks to simplify them to take less time and concentrate on the importance of tags like this so that there is time to do a thorough job
If one surveyor finds a deficiency, the reminder of the team initiates at least 2 other residents using drugs for dementia or behaviors during stage II
If focus is to stop iniitation in nursing homes….that is a low percent. You can do that but then sample should select people not yet on antipsychotics and evaluate if the facility is providing dementia care. This really addresses the prevention.
Revise the roster matrix-category for antipsychotic meds.-now
Separate tag for antipsychotics
Relationship with CMS:
Use FOSS as a resource, not as police.
Let the Federal surveyors teach State surveyors rather than just rate our work.
Miscellaneous:
Limit the mentally ill population from being admitted to long term facilities for the elderly
The entire survey process could be helped if we could retain experienced surveyors.
hire/train better candidates as surveyors. many don't care, aren't interested or have a lack of understanding
mandate that SA and RO office have same inservice info and same literature to reference. Ereryone has different background and experiences. The intpretation of this tag and many others is very individualized based on those factors
look at short term stay versus long term stay residents
Define IDR requirements and what is not allowed
Coumadin still needs attention
Put a financial incentive in place for facilities than do a good job(all areas).
I feel facilities are currently making attempt to reduce antipsychotics. have not experienced any recent needs to cite this tag for antipsychotic use
Question 39: Do you believe that your State Job as a survey makes a difference in improving care? Why, Why not?
More than 300 Surveyors answered Question 39.
Many Surveyors, particularly those with more than 10 years of service, identify specific improvements in care that they have witnessed over time:
Yes, year after year we go back to facilitys and see fewer side rails, fewer inappropriate psyc meds, more homelike and resident centered.
Yes. Even if we meet resistance or fail to "prove failed practice" we still raise awareness. in the pst 10 years we have made a difference in restraint use, use of alarms, prevalnce of side rail use. We are seeing fewer facility aquired pressure ulcers. Our State has mandated higher minimum staffing levels (although, as I said before, facilities will use it as "max" rather than "minimum")
There is no brief answer. Lots of observation of the resident's alertness, interaction with staff, any behaviors exhibited. Record review of the facility's system to reduce psych meds; documentatoion of monitoring, documentation of non-pharmacy interventions.
Been a surveyor for almost 14 years. Personal grooming, attitudes of nursing aides, and activities for residents have improved greatly, and I believe it is because of frequent citations issued for dignity, abuse/neglect, and lack of worthwhile activities for residents. I have seen a lot of improvement over my tenure as an HFQE, however, the facilities have a way of addressing only what is frequently cited. Some surveyors cite only the obvious and don't delve into root causes such as understaffing. I think that the PPD for [State J] is woefully inadequate and needs to be adState Justed especially as more and more residents are diagnosed with dementia. Staff need to be trained to be more interactive with residents as opposed to being task oriented in their approach.
yes, I believe that the quality of care in long term facilities has improved in the past decade. We cite falls less and less, medication administration has improved, presssure ulcers have improved. we rarely cite abuse tags.
Absolutely! Have had numerous experiences related to F329 – resident's experienced weight loss, no interest in everyday life, frequent falls, etc. and after surveyor has cited F329 drug was assessed, perhaps reduced or changed. Have seen resident's later and they don't even look like the same person.
Yes – compared to what was observed from 1994 to the year of 2013 it is clear and unmistakeable, especially for restratints, drugs, pressure sores and nutrition
I have been a surveyor since before OBRA. We have made wonderful strides in eliminating physical restraints, decreasing pressure sores and malnutrition. In the past we focused more on quality ot life and less on the medical model which unfortunately has been gradually changing. I can give multiple examples of things we have been involved in as surveyors which improved residents quality ot care and life.
yes, I believe that the quality of care in long term facilities has improved in the past decade. We cite falls less and less, medication administration has improved, presssure ulcers have improved. we rarely cite abuse tags.
yes. Over the last 14 years I have seen tremendous improvement with critical thinking and assessments. Improved pressure sore care and management. I used to cite weight loss and now I rarely fing a deficiency with F325.
Surveyors provide examples of administrators and staff thanking them:
Yes, I even had a facility administrator call after I cite F329 and thanked me. They could not get the pysician to do the recommended dose reduction for the resident and within two weeks the resident started talking again and interacting with others. It was a WIN WIN.
Yes… Alot of staff thank us because if we didn't cite it, nothing would get done alot of times…from corporate levels
Yes because I have seen positive changes sustained after memorable surveys. I can't say all facilities sustain changes, but those that do, often mention how much better things are for them. Residents seem happier and families do too.
absolutely. what we do makes a difference in the day to day quality of care the patient recieve. We improve the safety and quality of care at every institution we visit. I have seen facilities inprove over the many years I have visited them as a direct result of the survey process. Many of them have told me this directly.
Surveyors also describe the thanks they receive from residents and families:
The surveyor is the obState Jective person that comes into the facility to look at all aspects provided by the business to the residents living there. We have legal guidelines to support us if the care provided by the facility is deficient or the services provided inefficient. We look at items that the staff may ignore by intent or ignorance. The residents who are able have said they appreciate our yearly visits. Residents and families have also indicated that they appreciate an organization to turn to when the facility does not listen. In each individual discipline, surveyors are resident advocates!
Yes. I have spoken with family members and residents that have told me so.
YES. For me before I walk out of the facility I try to the best I can to make a difference even if it is for one resident- It gives me personal satisfaction to say to the residents I am here to make sure they are taking care of you and they are doing what they are supposed to do. Some times I get to hear it from the residents/family members and it gives me great satisfaction.
Many Surveyors answer that their work affirmatively makes a difference. But two different perspectives are apparent. The larger group of surveyors describes some variant of being a new set of eyes and ears for facilities, serving as external quality assurance, or teaching facilities how to provide better care. In contrast to their facility-focused perspective, a smaller group of Surveyors who describe their work as making a difference focus on residents and describe their advocacy on residents’ behalf. Some Surveyors combine both perspectives in their responses.
Facility-focused perspective:
Yes. Our oversight of facilities encourages good care. Also, we are another set of eyes reviewing care and providing guidance.
Yes, we identify areas that facilities need to improve to ensure that the resident's receive the best care possible. Often as "outsiders" we see things that the facility does not see or becomes used to or overlooks.
Yes. Facility can get so focused on hands on care if no problems identified they can miss problems/desensitized to issue.
Absolutely. I think we provide a third party type approach and help clarify the regulations to facility staff, in turn doing what is best for the resident.
Yes. Please it is an extra set of eyes to come in and watch for residents' interest. Often a process breaks down and the facility does not see the processing breaking down because they are too close to it and see it happening in small steps
yes, because we are the outside obState Jective eyes that provide facilities with insight into deficient practice that they may not realize as they are focused on everyday tasks.
Yes it allows us the oppurtunity to educate staff and residents and work with facility's in improving the quality of care. Some facilities are resistant and there main goal is to cover up any issues But there are more facilities that want to learn and improve care.
Yes, sometimes facilities State Just need a second pair of eyes to look at situations.
Yes, the survey team is made up of different disciplines who serve as an outside set of eyes to he facility to help identify concerns so that plans can be put in place to improve the quality of life for those who require nursing home placement.
Yes, facilities have State d to me that there is always room for improvement and appreciate the education we provide and would like more clarification and guidence themselves from CMS
Sometimes State Just for the week that I am present in the building, sometimes longer if the facility needed information on best practices and a different set of eyes to point out concerns
yes. I think that facility's have a tendencies to become complacent with resident care over time. I believe that the surveyors bring a fresh perspective and assist facilities in seeing residents as individuals rather than a group of residents as a whole in their facilities.
Yes. I am another set of eyes and ears coming in from the outside. I have not become complacent in the care for a certain indivdual or have become bogged down in the everyday goings and comings of the facility schedule. I can look, review, and interview and see what care is or is not being provided to improve the quality of life for a resident.
Yes, because of my experience in LTC I know what the facility should be doing to care for the residents. I always tell the facility that I'm not there to be their enemy I'm there to be an extra set of eyes for them.
I'm a newer surveyor, I would like to believe that what I do makes a difference in improving care. At the same time, many of the facility staff perceive the surveyor as an adversary that is there to criticize their work, rather than an ally there to identify their deficiencies in practice, so that they can provide the best possible care to their residents.
Yes – in a way, we are their outside QA
Yes. Helping the people that provide direct care to learn and change is more rewarding than simply writing citations for something that needs to be changed.
Yes. Helps the facility identify areas that need improvement, and requires them to improve them via Plan of Correction for deficiencies.
Absolutely – I believe that State Just by questioning processes and determining whether the facility is or is not in compliance, it assists the facility to relook at their own policies and system
Yes, to some extent. We provide a neutral, hopefully, view as to the care provided. When we talk with the facility staff about our findings it provides the opportunity for them to understand how an outside source "sees" the facility. This provides the opportunity for learning and, therefore, change. Change rarely happens when we State Just cite without letting the facility know why we see it the way we do.
yes for the most part. Sometimes facilities do not recognize the survey process as partnership to improve the quality of care and life for residents.
Resident-focused perspective:
yes, even if it is a small change. The resident has an advocate. We are holding the facility accountable. It is the best decision i have made in my career, advocating for people without a voice versus being a paper pusher.
Yes- We are a voice for the residents which allows improvements to be made in their home and their life based on our findings.
Yes I do. I believe I save lives every day. I make a difference in the lives of the residents, even in a small way.
I definitely believe I make a difference. My focus is on the resident, and if I've/we've found something that could make thier lives better, then I'm happy.
yes, sometimes we are the last voice that residents have
Most diffenently! Love my State Job! We improve lives for residents. This is not a State Job this is a calling.
RN more than 10 years traditional State F
Yes. The survey teams are an advocate for the residents. We assess and intervene when an area of deficient practice is identified.
overall,yes. Ibelieve believe stongly in all of the Requirements of Participation and serving as a surveyor gives me the opportunity to identify and advocate for people, protecting their rights as human beings, citizens of the United State s and recipients of appropriate care and services to meet their needs.
yes, I believe that everytime I go into a facility, I make a difference in the lives of the residents, I took this State Job to help and ensure that residents would be cared for and treated with dignity and respect, and I believe that is what we do, as a team, when we enter a building, we look after the residents, and their homes, and their rights. I feel that our State Job is an important one.
Combined response:
Most definitely! In my short time here, I have seen so many changes in the homes, which help improve resident care. I have been to so many places where the residents and their families thank me for what we do for them. Some families and residents tell me how helpless they feel and how they need a stronger voice. Most of these homes get so busy and go through so many staff members, they lose sight of what's right and what's wrong. It is our State Job to help protect the residents and encourage growth in these homes to bring a better life to these residents.
Some Surveyors focused on their authority to enforce standards of care and on the importance of the survey process:
Yes. Routine monitoring and unannounced surveys require facilities to achieve compliance with all regulations.
I think so…without our oversite I could very easily see facilities using inapproprite medications for residents for inappropriate reasons.
absolutely- my ability to cite deficiencies forces facility to make changes that improve care. My authority as surveyor gives me the ability to oversee resident care and give guidance to facility on providing good care
Most definitiely
Facilities are very in tuned to deficiencies and many will not improve care until forced to by a deficiency. Some think that if they were not cited for it on survey, then they do not really have a problem or need ot improve on anything
Yes, I see change made during the survey process and feel like it is partly because of the annual surveys and the facilities desire to be in compliance
Yes, faciltiy's become lax if not held accountable
Yes, I would hope we make a difference, I would hate to know what would go on in the facilities if we were not there overlooking at least the 9-15 mth. Period
Yes, having worked in facilities for 15 years, I think facilities will not always do the right thing if "rules" do not have some consequences.
Believe that a surveyor's role is very significant in having impact on the quality of care in LTC Facilities. Have seen the positive impact over the years of how qualtiy of life has improved in this setting. There needs to be regulatory oversight otherwise it would be too easy to take shortcuts at the expense of the elderly population.
Yes. I do. Without the survey process I believe the overall care would be much worse, in all respects. I think we'd see more incontinence, more falls, more restraints and more drug use
Oversight of the care provided to nursing home residents is essential to achieving positive outcomes.
Yes. Facilities change processes and make resident friendly improvements in response to federal and State requirements, surveys and citations. If regulations are not enforced, they may not be followed.
Yes I feel that the oversight is necessary in the facilities to ensure that residents are receiving adequate care and are not harmed. It is good for the facilities to be accountable for their actions.
Yes, if nursing homes were not routinely inspected, the bad performers would continue and even get worse.
Yes, it definately does make a difference because especially with staffing and corporate changes it seems to require a deficiency Tag to get things done
Yes, We continue to monitor the care that is performed. If no one is observing care then the faciity can do what they want.
yes, often by what we investigate or cite, facilities and staff are more aware and educated about the regulations. They think they are following the regulations because some issue has never came up, not because they State Just do not want to do it. As in antipsychoactive medications, until we inquire what interventions were attempted before beginning the medication then they may think because the physician ordered it then it meets the regulation and not what is best for the individual.
I believe the survey process helps hold the facilities accountable for providing appropriate care for the residents. Without the regulations and surveys, there are countless areas where the facilities could become "lax" and substandard in providing care to maintain the highest physical and mental well-being and quality of life for its residents.
Absolutely? if facilities not monitored would be a free for all
Yes, We cannot leave the facility to regulate themselves it is not feasible
Some Surveyors express skepticism that the regulatory system makes a difference for some nursing homes, particularly for owners who are more focused on making money than on providing high quality care:
Rarely. The bottom line in nursing homes is cost reduction and that often means care suffers, since staff is the largest expense in a nursing home
Sometimes can make a difference but it is rare. Usually direct care staff is passionate about their resident care but need the owners and/or administrative staff to invest financially in them: including salaries and education. Adm. staff too quick to point fingers and terminate dedicated staff when mistakes are made rather than taking the time and money to educate.
Yes, I think there are many fine providers out in the field, who would do a good State Job and would look at things (like medication) without us. I also believe that there are a number of providers who chose to meet the bare minimum of the regulation. They would not provide enough staff or do more than basic to less than basic care without the regs. Some providers would not put the money back into the facility for improvements to the physical plant, activities, maintaining enough supplies, etc. Surveyors act as an outside set of eyes for the facility and if we are doing our State Job well, can lead to improvements in the facility with their own process.
Yes, I do. I have seen many poor facilities and sometimes the only way these facilities will wake up and change for the betterment of the people they care for is to fine them. They are money hungery and only listen when that portion of their life is affected. I also get discouraged when we go into a facility with a hx of many issues, have several complaints to accomplished along with the fullbook survey, have a smaller team and expected to have all this accomplished in 32 hours. I feel at that point I am ineffective to do a good State Job and leave completly exhausted and wondered how much of a difference I made for these residents.t is more than fixing F329 to solve the challegenes surveyors face out in the field.
In over 20 years I will say 'sometimes'. Facilities that take public health seriously will change and improve. Facilties that budget line items for survey fines do not appear interested.They State Just plan for it in operating costs. I have facilities improve and decline depending on administration and ownership. I do believe when we identify serious situations we have the ability to force change but its sad that an Immediate STATE Jeopardy is needed to do so.
Surveyors who think their work does not make a difference or only sometimes makes a difference cite the recurrence of deficiencies from year to year:
It seems like I go into the same facilities year after year and the facilities State STATE Just take the 329 tag. They often State that the attending Dr.s don't want to be told by the State what to order, despite yearly explanations to the facilities. It also dosen't help that we get only 1 to 2 day look back period for a follow up survey. This is not an adequate time frame to evaluate the facilities plan of correction.
Sometimes. Being in this State Job almost 10 years, the whole survey process is State Just a circle of paperwork. There have been times where my findings and/or observations helped a resident, but that is few and far between. Most of the time, its State Just a vicious circle. We do a survey, the facility gets cited, the facility does a plan of correction, the facility gets back in compliance. Then the whole thing starts over.
Not really, the facility goes back to the same "bad" practices after the revisit is over.
To some degree I do, however, we go in cite, and the next year we go back and see the same situations.
Maybe for the short term, but we site same things year after year. Their imrovements are not consistent.
Yes, although I believe complaint investigation to have more impact on care, because you can more thoroughly investigate, make a determination and then the plan of correction is specific and well thought out. Sometimes however, facilities correct State Just long enough to get through their revisit and then do the same thing again. I have seen that at one facility over and over again- one that uses many antipsychotic meds and has lots of behavior.
Some Surveyors describe the sheer rush to get surveys completed:
Back when OBRA 87 was first implemented, surveyors' knowledge helped facilities improve resident care. Now, surveyors don't have the time to survey thoroughly and facilities know this. They're getting good at hiding problems. Unless more thorough surveys can be completed, a surveyor's State Job will make less and less of a difference to improving care.
Some Surveyors believe that the Quality Indicator Survey (QIS) hinders regulatory oversight:
Most of teh time I feel I do make a differnce, However since the QIS process was started in our State , I feel we do not cite as many deficiencies and we spend all our time on the computer as opposed to looking at the residents.
I use to, but since QIS I not sure we survey anymore, State Just ask and type in answers and State Jump through hoops and miss the more important issues.
I usually deal with complaint investigations more that annual surveys, but it seems the complaint investigators find multiple problems, whereas the team completing the annual survey hasn't found issues. Sometimes the same resident's are sampled. But the computer is telling the surveyors what has to be looked at and answered and there is no reason the surveyor's have to look into other areas, as it already is a too time consuming survey process.
Yes, but I believe the QIS process has taken away the art and skill of surveying. Now we spend most of our time looking at records and not at residents.
I especially dislike all of the MDS-triggered tasks on Stage 2.
Yes. There needs to be a process in place to ensure residents are not placed on Antipsychotic drugs for convenience of the facility. The survey process is used to identify this. However, the QIS proces in the first Stage does not allow time to observe more. There is too much time used in data collection.
Some Surveyors describe the enforcement system as too weak:
Yes, for the most part. I State Just feel the enforcement process sometimes does not make it worth it due to the fact that $ penalties arent always given and when they are, they end up being reduced. The facility knows they wont have to pay big money so they are not as likely to hold their standards.
Some Surveyors express concern that resident care will not substantially improve until staffing standards are improved:
I do; in that I believe we serve as a deterrent to the facility to not fall back to the barbaric days of restraints and resident abuse. I do not, however, believe we alone can improve day-to-day resident care by rules. Until the most important rule of resident-to-staff ratios are enacted, it is not possible to implement the most beautifully written plans of care.
Sometimes. More often I feel as though the issues that are indentified can't be solved within the current framework of staff in a facility. One can't expect the highest level of quality of care to be delivered by a staff with bare minimum education, skill, and numbers.
Other Surveyors who have doubts or no longer think they are effective identify lack of support from state supervisors and their States’ perspective and approach and oversight of survey activities:
I used to think so and liked the State Job for that reason. I now beleive that as a State we are being told to be kinder and gentler to the provider. I always approached the State Job from a team perspective with the provider and told the provider this was to make everything better for the resident. I never in all my 8 years had any issues with providers. I feel like we are now being presurred to side with the provider when they identify why they have or have not done something.
On my better days, yes! especially when the facility takes accountability for the failure to provide the good care!
When I work hard on a deficiency and then it gets thrown out by central office or the supervisor this is disheartening and frustrating. I don't always see the loyality is being given to the residents.
No. I work very hard and always place the patients first and foremost in order of importance and priority. I have been a patient advocate most of my adult life. It is very disheartening when management says that my State Job is that of a fact finder and my role is not to make decisions. It takes the function of the team away from the team. I do not think it is helpful to the team function if managers or others on thier behalf, who do not know the surveyors, are calling facilities to find out if surveyors were helpful, friendly, giving suggestions, wanting to know what the surveyors could do to make the survey process better. This could make some surveyors hesitant to question staff, to ruffle feathers.
no. I would like to think so. But there are so many times when I feel like my investigation shows a deficiency. It seems that if there is not a negative outcome or if it only affected one resident then it is not good enough. We are trained to try to make your citation as short and simple as possible. With my region, I feel like if we don't have a ton of evidence then the deficiency isn't good enough. It doesn't matter if it only affects one resident. And, if there is not a negative outcome, then forget it. It makes me mad because the regulations have a "potential for a negative outcome" in the literature, but that is not how deficiencies are looked at. I also don't understand why we do revisits with a plan of correction if, when the things are not in place that were addressed in plan of correction and State d they would be put in place, then why can't we as State surveyors, hold them to that. I feel like it is all a waste of time and tax dollars quite often. I get very discouraged.
I would hope, but there has been too many times where as a surveyor, I wanted to cite a deficiency and was told I had not enough interviews with this person, or that person. VERY FRUSTRATING!! Federal training and State training needs to go together. We are taught one thing at federal and then when we get in the real world are told go by supervisors rules.
Sometimes, some facilities are more resistive to change and surveyor findings, recommendations, some facilities are still not accepting of surveyors who are non-white, some facilities put pressure on surveyor supervisors to change findings and supervisors then override surveyors.
Politics is also having a bigger impact on surveys, according to some Surveyors:
Yes and no. I don't care whose name is on the outside of the building nor do I listen to what others say about the facility. I like to look at each one individually and without preState Judice, and I try to apply the rules equitably. It's disheartening when the politics dictate what gets cited. I almost quit when I was told a citation may "go away" because of political baloney. Luckily, my citation was supported via the IDR process. The concern I have is we are not holding everyone to the same rules, but I guess that's State Just the way it goes….
I used to believe one had to follow the rules in order to remain open, but that is NOT the case, and that is MOST disheartening. We try to do what we are supposed to do, but what difference does it make? There are a number of facilities in our area that consistently either do not measure up or fail to correct their deficiencies and yet they remain open. It makes you wonder what you are doing here?!! I've worked in the industry as staff and as a DON. I have been a surveyor for two years. I try to be open, friendly, and as informative as I might be in an effort to have a positive impact.
Yes, but has gone down with political attacks from appointees. They speak at all the nursing home confrences and call out surveyors negatively by name…this is our secretary's office. You guys are in Baltimore; we live here, daily. Nobody has our backs, so why should I stick out my neck–especially when other State s don't cite a single ISTATE J on a complaint in a year?!
yes. have seen a positive change in the years that I have been a surveyor. But have also seen much more political game playing.
Some Surveyors express mixed feelings:
At times I feel I make a difference when I know at least one individual's life will be a little bit better after I leave a facility. Other times I feel it is State Just a State Job and I get tired of the fight. There are 522 deficient practicies and most surveys it is State Just a fight to get surveyors to write one deficiency.
Not always. It is sometimes a game that is played. The facility trying to put only the best in front and not communicating with surveyors openly. Facilities see surveyors as "the enemy" and not as working towards the same goals
Question 40: Do you believe that enhanced enforcement citing F329 will contribute to reducing the percentage of long-stay nursing home residents who are given antipsychotic drugs? Why, why not?
Many Surveyors believe that enhanced enforcement will reduce antipsychotic drug use in nursing homes. Most Surveyors cite the increased focus on antipsychotic drug use as leading to reductions. Some Surveyors describe various facility motivations; others point to the success in reducing physical restraints; and still others report they have already seen reductions in antipsychotic drug use already.
Increased surveyor focus makes a difference:
It will improve some but like children who are spanked too often, facilities just keep on doing what they think is right
Yes – typically what gets measured gets done.
Absolutely, knowledge is power, enforcement empowers surveyors and facilities to take active roll in change
Yes- if you start to question the physician on why -what did he see, examine or asses to write the order- and continue to make the MD accountable–you might see a change. But the faciity must also change in the culture that old people shoul be sleeping or quiet and never cause a problem. Staffing has got to be increase-training must be done for the aides and nurses to cope and handle psych residents.
Yes. I have seen residents given medications. psychotropics in years past for staff convenience. Today's practices are better because of the regulations and enforcement of those regulations.
Yes, as stated above, all too often these drugs are used for convenience, and in the absence of identifying behavior triggers and formulating a true behavior plan with resident centered individualized interventions. Often these drugs are used due to lack of staff, such as for wandering residents. Staff are also undereducated in dealing with dementia care, even though facilities indicate that training is provided. Dementia care is a specialty, and some of the staff in facilities providing care are really quite rough, and not trained to deal with these types of residents, which can lead to abuse, which probably does occur because of these reasons. Fortunately we do have regulations to address abuse and abuse prevention and investigation, but you have to wonder how much goes under-reported or under-investigated.
yes-i think they need to be held to very strict standards r/t the use of these drugs especially in the elderly
Properly scoped… yes.
Yes..because the facilities do not try other interventions often enough but instead rely on the use of drugs to control behaviors. They do not assess the residents for other reasons that could be causing the behaviors such as UTIs, abnormal sodium or electrolyte levels, fear and depression.
Yes, if facilities and physicians are accountable then usage will decrease.
yes. It will force facilities to think about staffing patterns and resident care.
yes, the facilities will work harded to find other ways to manage behaviors, will lead to more individualized care palns and care and will ultimately lead to increased staffing ratios
Yes because once the physcians are on board with trying to do GDR's and proper documentation then at least they will be looking at this issue and doing whats best for the residents involved
yes, making facilities more aware and more accountable for watching and actng on this will make a difference.
I do believe that enhanced enforcement of antipsychotic drugs will help to reduce these drugs, which in my opinion, are given for the convenience of staff, and not the enhancement of resident's quality of life and comfort.
Yes, facilities will begin to more effectively examine the use of these drugs to prevent citations and enforcement
yes,facilities will become more responsible toward the use of these medications and will strat to consult with the md and pharmacist to enure compliance
Yes. The facilities know that they will be held accountable, and with the survey results published online, families are now looking closer at facilities before putting family members in them.
Yes, if nursing homes understand there are consequences to using antipsychotics they will find more alternatives to them.
Yes, because it will make facility staff more aware and receptive to finding ways to reduce the medications.
yes because facilities would put pressure on the physician
Absolutely!! It is too easy for facilities to put someone on an anti-psychotic to control behaviors that may be caused by something else. They don't have the staffing to address so they push a pill.
Yes, It just makes the facility more aware of psyc meds , gradual dose reduction attempts, side effects, other med pharm interventions.
Yes. With the recent initiative r/t to the use of anti-psychotic medications in resident with a diagnosis of dementia, facilities are starting to review their use of psych drugs more so than before this came out. Not all of them but some definitely. More enforcement will only improve resident outcomes.
Yes, until they leave and go to a lower level of care or the hospital where antipsyc meds are used way beyond reason. then they return to the facility who has to stay on top of antipsyc meds from the get go.
It could, I think since the start of having facilities look at antipsychotic drugs, they have become more aware and our cutting back on antipsychotics.
I do believe that if this is investigated as directed, it should definitely decrease over use.
Yes, I hope so. Will reduce the number of residents who recieve antipsychotics as a convienence for facilities
Yes. The idea of giving them to the dementia residents was never really thought out or supported by research.
IT SHOULD. THEY ARE AWARE THAT TOO MANY PSYCHOTROPIC CAUSES PROBLEMS. ALSO RESIDENTS DO NOT NEED TO APPEAR DRUGGED. ONLY THOSE WHO NEED THE ANTIPSHOTICS SHOULD BE PRESCRIBED THEM.
yes, as the enforcement spreads so goes the nation. The more the facility understands the more likely the idea will be accepted.
Yes. Some facilities don't do anything unless forced.
yes because facilities can no longer give medications to make it convient for the staff.
Yes, Through increased staff understanding and awareness.
Yes it will because citing brings change.
Yes, hold facilities accountable
Yes I believe enhanced enforcement will help residents because I truely believe that some facilities even though they have documentation on behaviors and non pharm interventions still medicate for staff convienience. Even though they have paper documentation, doesn't mean the interventions are being attempted….. it just means they are documented.
Would prompt facilities to look more closely at their practices
yes, because facilities communicate with each other
Yes. Facilities will not want the bad publicity or pay the fines. It will affect their finances.
Yes, because whether or not it is in the resident's best interests, facilities will be afraid of being cited and not administer them when necessary.
Yes, but I think it will take a while – especially as long as facilities have sketchy staffing.
yes If they know there is monitering there will be better care
I do not think it will change the numbers very much. I think it will improve the overall care of the people that need this type of treatment.
Yes. It is a comprehensive approach to decreasing antipsychotics.
Yes because it refocuses the issue. This was tried several years ago, them CMS changed the regs and took the focus off of antipshchotics.
Yes. The facilities will put more pressure on physicians to reduce use of antipsychotics. Encourage facilities to incorporate more non-pharmaceutical interventions.
Yes- as I said in #39, the homes have lost sight of the big picture. The enforcement starts a chain reaction of thought and ideas to improve the situation of the resident so the antipsychotic drugs may not have to be used or may be reduced. If the homes are not cited and encouraged to find ways around the use of these drugs, the homes would continue to use the drugs for convenience. The use of other activities and interventions for the resident can be found, if the homes are encouraged to look.
Yes. I think people are often inclined to leave well enough alone, and the current regulations mandate dose reduction, or at least to consider it.
Yes of course, we will look at it closer and so will the facilities. It significantly impacts residents to be treating "behavior" with medication instead of finding non pharmaceutical interventions to help them throughout their day.
yes, because for right now the surveyors are putting pressures on the facilities to train staff, document behaviors, encourage physicians to change the way they prescribe, develope better care plans, increasing citations.
Yes, the industry is more aware of this issue.
It will take time but I think they will look harder at their drug use. I feel the physicians are the ones that need more education.
I think this is just like side rail use After a couple of years they are used less and more thought goes into their process
Yes, more awareness on the part of the facilities is always positive
yes I have already seen changes from when I first came in 19191 when residents were automatically given Haldol when they were admitted to facility.
yes, like everything, when emphasis is placed on something and all work towards a common goal change is inevitable
Yes. Based on CMS's Initiative we have seen signifcant reductions so far with antipsychotic drug usage. Pharmaceutical industry has too strong lobbying impact therefore it is critical that enhanced enforcement takes place.
Yes, because bringing it to the attention of those involved will make them have to look at the problem and fix it, hence bringing the reduction down.
Yes, facilities put residents on medications then are afraid to take them off. They need to be more educated to find out why the resident is having the behavior. All behavior has meaning.
Yes, some facilities become very complacent about the use of antipsychotic drugs. Staff aren't well educated and if a resident exhibits one episode of negative behavior, instead of assessing the resident, they contact the physician/psychiatrist for a medication order.
yes, clear direction and enforcement of the issues will translate into compliance
Yes, it already has reduced the instances of antipsychotics but has increased the use of Depakote
Psych meds for geriatrics is long standing and potentially hard to break habit by the medical community-we have to continue to try and be the voice that contributes to the change.
yes. i think that nursing facilities need to focus on behavioral interventions….no pill will cure all behaviors….its takes a little time and effort and may need more staffing something that i know facilities dont like to hear.
It will influence, but to make a difference in reducing we have to influence the hospitals, physicians, medical directors, and pharmacists in working together toward that reduction.
Yes. Brings attention to need for increased supervision/monitoring.
yes. it makes the facility and thier staff more aware of the requlation and the negative effects antipsychotic meds can have on residents
Yes because the more we focus on an area and teach facilities what is the best outcome for the resident, the more they comply resulting in improvement for residents.
yes, wil make facilities more aware of this and hopefully will try to train staff to find other ways to deal with residents instead of drugs.
Yes. They only look at what we look at if we are watching they are always more careful
Yes I do believe that antipsychotic drugs will be used less to control behavior. We are now seeing specific programs to enhance lives of people with dementia and Alzheimers. Facilities have listened to, and attempted declining and elimination of antipsychotic drug dosage.Mental health has long been ignored, however I believe attention and guidance can reap favorable results in treatment beyond drugs.
Yes, as physicians become more willing to accept pharmacist input, use of these drugs will gradually be reduced.
For those facilities that take resident care as something more than providing a bed and meals but enhancing the quality of life of its residents they'll appreciate the clarification and direction if done correctly.
It will and can impact residents who are started on antipsychotics in nursing homes. It may not impact too much those that come into the facility already on the drug.
Yes. If the physicians and facilities are made to be more responsible prior to just adding a drug there should be fewer antipsychotics ordered.
Absolutely. As people age and have more medical age associated problems, they may not need as many drugs. You don't know until you try to reduce medications. Families need to be educated not to dictate care in long term care. Facilities are definately afraid of lawsuits from families in long term care. Staffing levels need to be approriate to provide care. Too much paperwork for nursing and less time with the residents is often what happens with all these regulations.
yes. Hopefully it will have the same positive effect as the restraint reduction initiative in the 1990's. It will enable both surveyors and facilities to become stronger advocates and result in the improved health and well being of the residents we serve.
Yes,because I believe that alternative measures should be used that requires thorough teaching of managing residents with Dementia and behaviors.
In some cases I believe it will reduce residents receiving the medications. But I also believe it might lower their dosages, ensure they are receiving the right medication for the right reasons and have less adverse reactions. I also believe it will improve the assessing and monitoring for use of the medicaitons.
Facility motivations:
yes, because nursing homes want to stay in business and continue to attract medicare residents.
Yes- Facilities want to be in compliance and will strive to not have deficiencies.
Yes – Nursing Facilities Do Not Want The Deficiency. Same affect as when we started looking at restraints.
Yes – I believe that if this becomes a priority focus, facilities would be more closely scrutinized and in knowing this, be more inclined to look at other interventions before ordering the med and would require them to tighten up on their process to evaluate. Maybe something that should be added is that antipsychotics and dementia medications require signatures and written justification by two physicians.
Sure, if they know we are looking for it, the facilities will concentrate even more on it. I just hope we don't go the other way too far and people end up getting hurt by a resident who was medicated correctly but was taken off of a medication which was working for them, because the facility knows the "STATE" is looking at anti-psychotics
Yes. Facilities are very aware of possible citations and appear to be making efforts to reduce psychoactive drug usage. I have observed this over the past few months while doing surveys
probably. Medications cost money.
Most facilities strive to be in compliance with the regulations and strive to provide the best care tothere residents. Through education as well as enforcement, facilities will likely attempt to minimize the use of antipsychotic drugs and increase effective behavior management programs.
Yes, when facilities lose money or status over an issue, they change their behavior.
yes, the facilities don't want to be cited so they will change their practices if they have no other option.
yes, because facilities understand the risks of non-compliance,i.e., paying fines
Success in reducing physical restraints:
Yes. Because I was involved in the past when we focused on physical restraint reduction. Unforunately some of the facilities eliminated physica restraints and turned to chemical restraints.
Yes. I feel it will be like restraints. Facilities know this is a focus and will concentrate on the reduction.
yes, from what i understand it worked for restraints and i think the same thing can be done here, right now giving anti-psychotics is an easy answer, if we make them look at other interventions more closely then the psychotropics will decrease.
Yes. Just as the restraint reduction initiative helped to reduce the use of restraints in facility's dramatically, enhanced enforcement will eventually reduce the use of anti-psychotic drugs.
Reductions already seen in antipsychotic drug use:
Yes, because I think this number has already begun to decrease.
I think the numbers have decreased significantly already and will continue with the current requirements.
Yes, I can already tell that most facilities are focusing more on appropriate antipsychotic use.
I have already seen a decline in the use of the medications in our state
Yes, because even now, with the CMS focus, I have had facility tell me they have stepped up there overview and are more closely monitoring the use of these drugs
Some Surveyors identify the need for additional strategies, such as educational efforts for facilities and physicians, to reduce antipsychotic drug use:
Yes. But more training for facilities will help as well. They still think that all they need is a diagnosis to use antipsychotic medication. Until they catch on to assessment and non-medication interventions, citing F329 may make little improvement.
Yes, but you have to educate the MDs and get them on board, otherwise we are wasting our time.
Somewhat. Enforcement is not the only factor. More education for facility staff, physicians and medical directors may help.
Yes. However, consistency and continual education of the need to reduce is needed. The survey process helps to ensure that steps are being taken to reduce antipsychotics in nursing home residents. For the most part facilities have been receptive.
Some Surveyors identify mixed motives:
Yes, I believe the facility wants to do the best for the resident just like we do. It is the difficult task of changing the culture and what is accepted by physicians and nurses as normal treatment of dementia. The more it is cited, the more the process will change if the facility has the education to know what to do instead and how to change their process
Some Surveyors qualify their expectation of change:
Yes, I think it will highlight the need to decrease the use and attach more awareness to the use of antipsychotic drugs.
HOWEVER – when a resident has been taking "x" medication for 30 years why do we try and remove them? If it works and the resident still has quality of life why do we try and change that?
Yes. But what we found in our region was the most difficult issue was getting the medical directors' to comply. They took HUGE issue and did not want to be told what to do. It was quite a struggle for the facilities to get them on board even with repeated tags.
Perhaps. More attention to an issue does seem to get some facilities to focus on making improvements in an area.
Hopefully. I see a problem with getting physician's on board.
Maybe because of increased education, awareness and that it is a current focus. Maybe not because physician's will add diagnoses and documentation to support use. Ultimately it is the physician who orders the medications and determines the dosages and whether or not a reduction is made. Physicians are not always receptive to having their decisions questioned.
Maybe- am not privy to how well enforcement has worked out- seems to have worked to decrease the use of physical restraints, pressure sores, etc.
May or may not depending on the circumstances surrounding the type of care for the resident's identified medical problems and what is feasible for the resident's condition that will maintaine the resident at their highest level of practicable well being given their diagnoses and prognosisi of their medical problems; what is achievable to improve to just to maintian without further decline in condition that would be avoidable.
Maybe. some facilities are geared to those with behaviors and so the usage will be higher
It may be possible. Some residents may be able to improve with therapy if they are not sedated. and have a quicker discharge. Some therapy plateus and discharges from therapy may be due to a resident being sedated and not able to participate fully, which is not a real accurate reason why they met there maximum potential. They may eat more and prevent weight loss and weakness, which could lead to shorter stays. They could prevent falls and fractures which lengthen stays.
Other Surveyors who believe enhanced enforcement of F329 will not make a difference cite resistance by physicians and facilities or facility efforts to learn ways around the requirements:
No. Most physicians that I have talked to are aware of the new CMS initiative but they will make the decision whether or not they feel a resident needs a psychotropic medication or not and whether a reduction should be considered. If they do not feel it is appropriate they will not do it. They know their patients better than us and if they think it is in their best interest they will continue to do what they think is right.
No facilities are struggling with what else can they do questions.
No. the drug companies will not allow it
no… i think , unless surveyors are given more time/ more staff, facilities will continue to "hide" their use like they try now.
No because of the increase in elderly population with dementia.
No, the LTC side has to be on board with the benefit of unnecessary medications. It may reduce the percentage.
The PA's and Dr.'s have to be educated and willing to taking responibility for administrating, monitoring and decreasing doses.
no physician's will continue to order what they want
no…phy/fam/staffother resident will not tolerate behaviors that can not be controlled and faciities do not have the staff /facilities to accomodate the needs of behavioral residents…reimbursement in the state of Texas is too low
No, because the physician will always take care of himself and any staff involved with an incident. Hard to argue with a doctor.
no- most of the residents I survey have a history of mental illness with complex physical disabilities that require a long-stay nursing home care.
No. Residents in the nursing homes are sicker both physically and mentally today. The residents of today almost always need medications to enhance the quality of life they and their loved ones experience. If we are making sure pain is being addressed today why not the resident who needs an antipsychotic drug.
No, it may reduce the increase of unnecessary medications but it wont reduce the # of residents who receive them.
No. I do not observe residents being overly-sedated unnecessarily. Many of the drugs are needed for the residents to have imroved quality of life
no – physicians will continue prescribing unless they are educated
Not really the physicians are going to do what they think is best
no, they will find a way-have physician orders stating-needed or GDR not recommended, or resident on medication regimen effective
No, we are just training the facility on how to document enough information to make us move on to something else.
No. I believe the facilities will just work harder to have evidence for why the medications are needed.
I do not believe we will see a major reduction. One of the reasons will be the cut back in programs available for the mentally ill. As the mentally ill become more common in SNF it stands to reason the use of anti-psychotic medication will also be more common. Another unfortunate aspect of our aging population is the prevelance of dementia, many with psychotic features which might also require anti-psychotic medications.
No, as the life expectency increases, so does the aging population and the onset for mental health concerns or the risk for associated neurological disease susceptibility.
No. There are a great percentage of psych residents living in LTC facilities
No. The physicians and facilities often just learn how to word things or how to document things so they are just good enough to not get cited.
no—- not all residents are of the "normal" mind. There are the residents with psychosis— behavioral problems—- schizophrenia— where anti-psychotic meds are needed for the resident to function or to keep the resident and other residents safe
No. Until there is a medication that can effectively treat the symptoms of dementia so that a resident is not a harm to himself or others, or can live a reasonable lifestyle in a faciltiy, the use of antipsychotic medications will continue. There are very few pharmacoligic options for treatment presently. Also, nursing home staff require more support (money, training, etc) to adequately use behavioral treatments. It is a known fact that reimbursement is dwindling, yet staff needs are increasing. This alone precludes that medicatiions will be used in lieu of staff treatment.
NO, I feel that if we enforce F 329 and can lead to weakening actual F 329
No, unnecessary antispsychotics are usually given due to behaviors staff are not wanting to deal with, enhanced enforcement will not necessarily change that
Some Surveyors are unsure whether enhanced enforcement of F329 will make a difference:
Maybe. It depends on whether there is a fundamental shift in the nursing home staff's line of thinking as it relates to antipsychotics. Antipsychotics should be used but only as NECESSARY that is why the regulation is called Unnecessary Medications
I don't know if all facilities can be evaluated on the same level. Some facilities have a higher percentage of residents with psych issues and behaviors, while other facilities do not accept these residents. It may be hard for those facilities accepting these residents to reduce their percentages.
Maybe. Unfortunately, many current residents are former long term psychiatric hospital residents and dose reductions do not work
Maybe. From what I have seen since returning to surveying is that the pharmacists and psychiatrists having been doing pretty good at recommending dose reductions. The emergence of more dementia specialty units also seem to have reduced the use of antipsychotics.
Probably. However, as in the example that I gave about my own mother during the time she received Depakote, I truly believe that no one has enough information to determine the side effects from the medication, only anecdotal information. The pharmaceutical lobby continues to find other non-approved uses for these medications. Also, families of dementia residents would opt for medication even if it only appears to act briefly. No one can attribute one factor as to why dementia residents slowly decline.
Some Surveyors believe that antipsychotic drugs are used appropriately and express concern that the Initiative could result in needed drugs being stopped:
I believe that antipsychotic medications when used appopriately are an effective intervention to be used. I believe some of our facilities are content to care for the "cute little grandmas and grandpas. " And are afraid to take in residents who may have difficult behavios or diagnoses.
Yes, but that may not be for the benefit of the residents. Some do benefit from the use of the meds, and if the facilities stop using them in order to avoid being cited, that could do harm to some residents who really need them. Use or nonuse should be on a case by case basis.
No. Some residents need some of the medications and because the regualtion is not totally understood bby the facilities, they remove the residents from the medications and thereby lowers their quality of life because their psychoses or behaviors return.
Possibly. Some residents do live better lives on these types of medications.
no Most that are on them appear to need them
Yes, for certain populations. There are some residents in long term care facilities with know psychiatric conditions that require medication management. For those residents the lowest possible dose must be respected. We do not want to harm the resident by making them endure symptoms that are problematic for them.
It may. Though it may also be that residents who truly need antipsychotic medications could end up without them due to fear of getting cited.
Yes, it will lead to a reduction, will that be a positive thing? Will residents suffering from psychosis not be adequately medicated out of fear of violating the new enhanced enforcement? Are there adequate safe guards to ensure this? What is worse, to be hallucinating and delusional or to have side effects? These are all very subjective
No but I believe there will be an increase in resident abuse when facilities are not allowed to prevent or decrease yelling, wandering etc behaviors.
That would depend on the facilities. There are facilities that have a high percentage of psychiatric residents that would not benefit from medication reductions.
Some Surveyors express skepticism about the nursing home industry:
For some yes. But for most no because the facilities are very good coming up with ways to get around regulatioins. A whole industry has been built on how to get through the survey process and they will be addressing any changes that are made. Electronic MARS indicate that interventions are done prior to PRN medications now. I often wonder how they have the time to do all the interventions they are saying they do.
No. I feel like as long as we have staffing issues (which all aides will say their facility does), we will have issues with inappropriately prescribed antipsychotics. Facilities would just as soon have a medication tag cited which potentially won't cost them much more than a few hours of staff time for inservice and training than face a much increased budget because they have to increase the amount of staff on duty per shift. They all run on shoestring staffing which barely meets standards. Additional staff could be utilized for not just dealing with dementia-related behaviors, but also other hot-topic issues like pressure sores.
It really depends on the facilities. Some are very good, and want to correct. Others don't seem to care as long as they can get into compliance until the next survey. Unless survey intervals are shortened i don't see anything changing much. With complaints we frequently go into facilities right after their revisit and find some of the same areas out of compliance. Sometimes at harm. It really makes one wonder, what the survey team looked at.
Yes. I think an initiative is necesary and will enact a more proactive approach. However there are always facilities who will "work" the regs to make it work for them.
unfortunately someone will find a way to get around the citation, but the hope is to help each resident, each facility because we know we could also someday find ourselves in the same shoes.
Yes. If there is an increased understanding of these drugs and alternative interventions are implemented, the quality of ife of these folks will be improved. However, the bottom line (profit) of the corporations don't allow for additional activity staff or increased dementia apropriate activities an an alternative.
No. Facilities will do what they do, and as noted above, their lack of compliance doesn't seem to make much difference…and won't until they are actually held ACCOUNTABLE to make changes….and citing the tags just doesn't seem to do the trick….
Perhaps – because facilities have learned how to manipulate the regualtion
No. The nursing homes would rather medicate away behaivors rather than hire additional staff for diversional activities
Unfortunately long term care facilities do seem to respond to enhanced enforecement and without it quality of care will decline
Some Surveyors identify particular problems with QIS surveys:
Yes. Some residents do receive antipsychotics with out adequate indications, etc. However, it is hard, in the context of a QIS survey, to do the appropriate follow-up to determine if a problem does, or does not ,exist. So much time is spent chasing all sorts of issues, doing interviews, observations, etc., on issues that don't turn out to be a problem at all, that there is far to little time to follow up and to do the significant foot work necessary to gain the necessary documentation to support a citation of F329. There is much wasted time.
Some Surveyors see staffing levels in nursing facilities as a critical issue:
I dont see that many residents now on antipsychotics. Without legislation requiring better staffing levels, you will never see real improvement in care
Yes. If resident are not oversedated they will be more active. This will decrease their rate of decline in their ADL's and side effects of the medications. There needs to be more staff required for residents who need antipsychotic drugs especially in the activity department.
No, behavior therapies and alternative methods of dealing with behaviors are directly connected to staffing levels and this is one of the weakest areas in the survey process. Either the facility meets the staffing guidelines or not and trying to associate lack of staff with behavior outcomes is difficult.
Yes if more nursing interventions were used rather than medications. A quick solution to management in the LTC nsg. facilities is to medicate the resident when all that person may need is to have more one-to-one personnal contact, a little TLC goes a long way to calm a person down and to provide reassurance or to solve a behavior concern. What is needed is more educated nursing staff. One licensed nurse and two nursing assistants are not enough to provide the personal contact needed to provide that extra TLC that could benefit these residents.
Some Surveyors predict little improvement without more meaningful penalties:
Depends on the facility, the make up of the facility and the residents who have behaviors. There is no financial incentive to keep from getting repeat deficiencies and facility improvement.
I feel F329 is fine, it just need to be enforced. The providers and especially the physician need to be educated – just like we did with physical restraints. We need to take the emphasis off of antidepressants and anatianxiety meds and spend out time and money on antipsychotics.
Only if it is a financial penalty, as this seems to be what gets the facility/corporations attention
Some Surveyors see factors other than enforcement as important to improving quality of care, including Culture Change and rewards:
If by enhanced enforcement you mean citations at level 2 as well as level 3, then yes. When everyone was cited for lack of sufficient assessment or potential accident hazzard for side rails facilities started to get rid of their side rails. However, we also saw facilities just work harder to justify their use. Culture Change activites in our facilities have just as much impact as citations in changing practice – proving that positive reinforcement works. We don't have to beat every facility with a big stick to realize change.
I would like to see rewards offered for homes who improve their QM numbers or other ways to improve LTC and regulatory compliance. Because of the enforcement penalties, staff fear us and the survey process. This leads to interviews that are untruthful and the surveyor as being viewed as the enemy. However, in many cases, I agree the penalties were deserved. I just wish there was another way to get what we want.
One Surveyor proposes an experiment to increase staffing and see its effect on antipsychotic drug use:
Depends. There will be an initial drop but what will happen is that residents will have the medications discontinued for a short term basis in an attempt to avoid citation. The meds will be restarted because the IDT believes them to have been necessary all along. We are a culture that expects a pill to make change. Perhaps CMS could try an experiment; pick a facility with a high percentage of residents that are on anti-psychotic medications, give the facility a grant to hire twice as many staff, reduce/eliminate the medications, and see if there is no change in behavioral issues.
Some Surveyors see no problem with the current use of antipsychotic drugs:
No. I don't believe the nursing homes assigned to the field office I work in are over drugging their residents or misusing psych meds. I was actually surprised that this was the new focus for CMS. Call the AMA if doctors are misusing drugs on their residents.
Question 41: Are you inhibited/discouraged in the fulfillment of your survey responsibilities by any policies or procedures or persons or other factors. If so, please explain, without providing names or positions.
The primary issue cited by Surveyors is the lack of sufficient time to conduct surveys and write deficiencies. Sometimes, the concern reflects travel time, but more frequently, the concern reflects the number of tasks required during a survey (including complaint investigations) and supervisors’ insistence that the survey be completed in pre-determined numbers of days – i.e., four days.
Yes. I have been told that an issue that I identified "is not one of our priorities right now" or that "it's not really important." I have also experienced time shortages on surveys where I could not investigate potential problems because I had no more time to investigate.
The survey responsibility that bothers me the most is the 1 to 2 day target date revisit window. 2 days is not enough time to evaluate the facilities compliance.
No…Just wish there was more time to do the survey process
Time is the issue. As the years have went by additional tasks have been added and the job has become more complex rirght along with the acuity of the resident. It is no one's fault. It is the reality.
Time is always an issue. Lot to do in a short period of time.
short staffed, don't have enough time often to complete tasks thoroughly.
The one thing that bothers me is the lack of team work and consultation concerning the survey process.
There is so much emphasis on getting the surveys completed "timely" that the care of the residents are often neglected by us, the surveyor.
Yes, managemnt locally and at state level, it seems unreasonable expectations as to job constraints, ie get in and get out expectations for survey process. Have been told it is a "small facility it is easy" Management doesn't recognize the size of a facility, or the census is not the only driiving force for the survey. Have actually had team be told by program manager under the prompting of their boss that after third day we are to get in and get out "day four go back and exit by noon regardless"
We need larger survey teams – too few of us to do a good job accomplishing all of the required survey tasks
The survey time allowance (too short) for the most part, followed by our central office practice regarding identification of harm, versus the FOSS threshold/perception regarding determination of harm. Even the FOSS personnel vary greatly over the years.
At times I feel there is not always enough elotted time to investigate complaints with several allegations. If you took the time you would be in the facility all week and then not have the office time to complete your reports or deficiencies if written.
At times we feel somewhat discouraged as it is the policy to base a survey's timeframe on the bed capacity of a facility. For example, a bed capacity of 60 results in a sample of 15 residents (13 without the closed records). It is generally expected that the survey should last 4 days. We sometimes find the facility staff to be difficult and not forth-coming with information which makes it very tedious to determine the facility's compliance. With most survey teams having 4 surveyors it seems as if that should be an easy job to accomplish in 4 days. That is often not the case. Also when the survey team's caseload has mulitple facilities that are a distance from their homes, alot of time is spent in the car rather than in the facility. It would be really nice if 7 of the 8 hours/day was spent in the facility. Caseloads are not always developed based on the location of the surveyors in relation to the facility's location.
I feel there is not enough write up time, so we rush through the survey in hopes of getting the write up done before we go out again. I do not know if there is a set number of hours to write up. I have done 329s and they take a long time to write, with all the behavior documentaion, nurses notes, interviews etc. I think some surveyors avoid citing it for that reason. We are not allowed any comp time or overtime, if we go over we take it back the next week and get behind even further, regardless of the difficulty of the survey.
No. Only lack of time and the expectation of surveys to finished in 4 days
At times the time contraints of getting done with the survey, the write up and so we can be ready to go out to the next survey. There are a lot of tasks required as part of the survey process. Following the investigative protocols as established are very time consuming.
No -other than time constraints – need to spend time on big outcome issues such as antipsychotics instead of nickle and diming the facility for smaller issues and citing all the assoicated tags.
The second issue most often cited by Surveyors is the decision of supervisors, management, or enforcement staff to downgrade or eliminate deficiencies that are identified by Surveyors:
Yes, a lot of times the head people want to be 100% correct before citing or they won't cite.
Yes I think at time the IDR process that is used in our state is not always consistant i.e., When at the facility and they are unable to provide us with appropriate documentation at the time of survey but then after the deficient practice is cited the facility will IDR the citation and when submitting their information will have the information they were unable to supply at time of survey…..this is frustrating because at times the deficiency is then dropped????? Why when they were unable to provide at survey and was not able to be produced by the facility.
yes at times but I'm out spoken the Regional Director is dictorial and wants enforcement to determine what can be written or not written before we leave the facilities….we don't listen..gets us in trouble but oh well
This is difficult to answer due to the passion I have in protecting the residents. Most of my career has been in the hospital setting and not the long-term care setting. I see, sometimes, how people who's background was from the long-term may have brought with them the attitude of "out of convenience." Some information gathered, during a survey, are down played to hurry the survey along. One particular time, after finding some significant problems on a survey, one surveyor clutched her chest when I asked if we were going to extend the survey time for another day. Needless to say, things all of a sudden were packaged neatly in a 5 day survey. I ended up in the complaint unit. Even here, I had written an SOD for abuse. I was told that my writing was too strong and it sounded like an IJ. My supervisor took several items of information out to make it "look not so bad". Another supervisor later told me it was because the supervisor missed the allegations and passed it to the program manager who was very upset that the IJ was not caught earlier. The perp did not do any interventions before calling the physician for an IM injection of Ativan for behaviors for two residents. The psychiatrist was not called, just the facility's physician who ordered IM Ativan for one resident and IM Haldol for the other. No interventions were done prior to these injections in a locked unit. I was still able to write up the EDL for the perpetrator, who had a past license suspension for abuse. I am still a so-called young surveyor and may need more time for trimming to be able to distinguish significant from not so significant. But I love what I do and I love protecting these residents.
Yes, we are told many things by our supervisors that make our position frustrating. Supervisors are not the ones that are out in the facilities, but yet they are quick to want to delete citations. I know there are facilities in our state that has never had a federal survey, yet other facilities have had numerous federal surveys, how is that fair? We have 5-6 facilities that take a lot of behavioral residents and have yet to have federal surveyors in their buildings, these facilities have a lot of problems and yet we are told not to cite much, because where would all these residents go? Again is that fair? Many of these residents are on antipsychotics and numerous ones at that, many have not had gradual dose reductions tried or even suggested and yet we can't cite.
It seems that we are "permitted" to cite certain citations and even if it belongs at 329 it is changed to something less severe ar cited at somehting that makes the problem apppear less than it is
In my region only certain cites are allowed.
Many times we as nurse surveyors identify concerns such as those discussed in #40 but due to the fact that we are addressing "minimum standards" we are discouraged to persue violations or deficiencies because we can not convience our peers or supervisors to a better standard of care. The enforcement process questions the source reference which is nothing more than basic nursing experience but they want specific reference material.
yes. I walk on egg shells in obtaining sufficient evidence to convince a tough compliance reviewer and then enforment team. I wrote a G level on a F-319 a few years ago and it was reduced to a D. I almost lost the citation, but my PM supported me. CMS reviewed the tag and recommended a G level
Sometimes seeing that enforcement throws out things you work so hard on can be discouraging.
yes, there is alot of pressure to decrease the scope and severity of deficiencies from harm or IJ to non-harm deficiencies
Sometimes deficiencies that were written simply disappear or if it clearly meets the harm level it evolves into a D level with no explanation to surveyor. In last 6 mnths survey team defined two facilities w/ meeting criteria for imediate jeopardy and somebody worked their magic to avoid immediate jeopardy. What is up with the definition of PA changing the definition of neglect and also not submitting PB22 for neglect unless if serious injury befalls the resident? I was informed by central office attorney that we wouldn't have any aides working in facilities if we were always submitting a PB22 for neglect and no serious harm resulted in the neglect.
yes, many times you do a thorough investigation, cite deficiencies only to have them thrown out. This makes you wonder why should you work so hard to get to the bottom of situations. Surveyors all have different work ethics which make the process difficult.
Sometimes discouraged from citing by supervisor.
Too many times people who have not been on site with us make deicisions that affecet our writing. We are not just writing. We are writing for a person or an office and not just writing a citation. There are too many in our agency with an outdated mindset.
Supervisors who are not on survey are deleting or changing the body of the deficiency. This is a dangerous practice. I have all of my original work in case it comes back to haunt me in an IDR etc.
I am discouraged that upper management does not see the job of the survey process as being done by healthcare professionals who have many years of experience and education as capable to make a decision, and are most likey more informed to make a reasoned and fair decision. It is difficult to understand how someone could confuse patient advocates as a just fact finders. I also do not agree that we should be going to facilities and giving out awards for being deficiency free. The facility is supposed to follow the regulations. Why do they get a reward for following the regulations? Our job is to insure that is what they do.
Yes, I feel as though I am micro managed by supervisors I am told often what to write and how to write including sentence structure. I am told to delete information I find necessary if the supervisor does not feel it is so, how when I am the eyes and ears out in the facility. Surveyors are not treated as professionals.
Occasionally, I feel hindered by the state agency. The philosophy is that the facility is our customer and the state agency will cater to their request. I feel that the residents are our customers and the regulations should be followed and enforced to protect the residents and to make things better for them in their homes.
I've found that SA hasn't always supported surveyors deficiencies when challenged by physicians in the past. Hopefully that will change.
I am discouraged that upper management does not see the job of the survey process as being done by healthcare professionals who have many years of experience and education as capable to make a decision, and are most likey more informed to make a reasoned and fair decision. It is difficult to understand how someone could confuse patient advocates as a just fact finders. I also do not agree that we should be going to facilities and giving out awards for being deficiency free. The facility is supposed to follow the regulations. Why do they get a reward for following the regulations? Our job is to insure that is what they do.
Management and reviewers do not always understand the reasons behind why we cite tags because they have limited field experience.
We are loosing surveyors because our State is unable to provide competitive wages.
Regional supervisiors delete citations before adequate QA.. Once the team have analysis and decision are made by the team to cite the faciltity, Western region supervisor are call and reviewed the potential citations.. during this call the RD have team to delete a citation based on conversations without QA and the appropriate documentations. Team is very upset about the decision especially after the work up of the citation and not given a change to prove the citation validity
Yes, travel time is not taken into consideration when scheduling surveys. Some surveyors drive back and forth to their survey which takes about one and a half days away from the survey for that one person depending on the distance. Some surveys there are over three and a half hours travel time one way and then the last day the same travel (again taking time away). Also accessing the computers at the facility is a very time consuming process.
team assigments and caseload assigments don't make sense all the time. we have surveyors on the wrong teams, driving hours a day when this is not necessary. more time in the car means less time in the facility observing, interviewing and reviewing records. It's a waste of my time when I have a team much closer to home. The good surveyors are shuffled all around and bad surveyors are allowed to stay bad. We have some who never cite anything and haven't for years. Nothing is done about it. So if I have a problem with meds on my unit and a do-nothing surveyor has no problems on their unit, that is suspect and I'm sure the facility is getting away with it because that surveyor doesn't know what to do or doesn't care. It's very frustrating.
yes, many times you do a thorough investigation, cite deficiencies only to have them thrown out. This makes you wonder why should you work so hard to get to the bottom of situations. Surveyors all have different work ethics which make the process difficult.
Feel sometimes have to argue for a cite that you feel strongly about.
No one person specifically but I believe that the Civil Money Penalty Enforcement is not getting the desired resulte. Instead of collecting money, why not mandate the facility spend the money to fix the broken systems that are the heart of the problem, the biggest of which is staffing. Must hire 2 more CNAs and 1 RN for day and evening shift… Since 1999 I have not seen a great improvement in care. We have focused on areas such as restraints and pressure sores and reduced numbers but the problem has not been erradicated.
Yes, I feel as though I am micro managed by supervisors I am told often what to write and how to write including sentence structure. I am told to delete information I find necessary if the supervisor does not feel it is so, how when I am the eyes and ears out in the facility. Surveyors are not treated as professionals.
Surveyors cite their states’ pro-facility attitudes and industry power at the state level:
Yes, I feel we are currently under pressure to be on the side of the facility by our state system. It used to be that the
resident was who we looked out for and now I feel like we are being told to be kinder to the provider. I feel as a surveyor who was always fair to the provider that this is inappropriate. You can survey and cite in a very professional manner and have a very good understanding with the provider. The state should not make such judgements on the whole. If they are concerned that some surveyors are too harsh in their approach then they should manage those people individually with some education about the process.
State's attitude of cooperation with nursing home facilities and using less enforcement
yes often the resident is not the focus but the provider is the customer in PA
One thing in [State J] that bothers me is that we are told that we are just "FACT FINDERS" and we need to be "KINDER AND GENTLER" to the facilities because they are our customers. I feel sometimes the things I cite don't mean anything because it gets tossed out at the state level or they determine it not to be as severe as we saw it in the facility. Sometimes it makes you wonder why we spin our wheels on a problem, waste time and it gets tossed out later down the road.
Generally, some facilities seem to carry a lot of weight with the state office and citations are overturned on this basis. Several staff at state office (who are in position of power to overturn citations) have never surveyed and don't have a complete understanding of process. In regard to Abuse/Neglect state office has reversed position of definiitions several times. Neglect policy now interpreted by state office as having to have actual harm from failure to provide goods and services–not failure to provide goods and services to AVOID physical harm.
Occasionally, I feel hindered by the state agency. The philosophy is that the facility is our customer and the state agency will cater to their request. I feel that the residents are our customers and the regulations should be followed and enforced to protect the residents and to make things better for them in their homes.
As noted above. I have worked in different states and have never seen the LTC industry have such an impact on what the state does like here in Missouri!!! It's almost like the industry tell US what we can and can't do. It's crazy!!! And those facilities who have horrific issues but never get closed make ya wonder why we do what we do…it doesn't make a difference!!! Those residents are just "stuck" with what they have because "where would they go if they didn't live there?" If the facility is bad, the processes need to be implemented to either help them turn around or they need to be closed down!
Yes. The industry associations attack us full blast with the full support of the departments (state) political appointees. If we try and leave, we are black listed from private sector employment. No one defends us.
Surveyors raise questions about various components of the survey protocol:
I would prefer to have less structured survey hours; or, allow surveyors to work 10-12 hr. days. There are several occasions where it would benefit having a longer work day (i.e. if a family interview is more accessible, or, a medication pass extends longer). It is also more conducive to continue an investigative thread until completion (i.e. observation, record review, staff/resident/family interview, and policy review). These things cannot always be scheduled ahead of time and the freedom to complete tasks as they avail themselves might be more effective. Although the survey is completed by a, "team," the majority of the work is assigned individually and, therefore, an individual's schedule should be allowed flexibility. Entrance and exit times would remain consistent with all members.
No- my coworkers and those in charge over me all seem to be very dedicated to promoting good care of nursing home residents. The survey process itself is what limits my effectiveness. Much too much paerwork- the protocols, the "dumbing down" of the survey process, in the name of "consistency". why do you not ensure that all the surveyors are truly capable and knowledgeable enough about long term care to make good decisions?
Surveyors raise concerns about survey teams:
During the time that I was on our Survey Team, I was VERY discouraged with the performance of the surveyors…most surveyors would look the other way or not cite the facility because "they fixed it right away" after a deficient practice was identified by the surveyor, or the deficient practice was "no big deal."
Sometimes the team does not work as a team
Although not discouraged, but inhibited at times. Many of the team members were trained long ago. Refresher training on regulation interpretation and citations would place new and seasoned surveyors on equal understanding of regulations.
I do feel that other surveyors inhibit and discourage my findings and that boundaries between the survey team and the facilities are sometimes broken.
Discouraged by the high rate of turnover in surveyors. It really takes about 3 years to feel comfortable in this job. People coming and going after only giving it a week or a month or just long enough to get SMQT makes it very difficult on those who believe in what we are doing and want the best for the residents.
Surveyors cite components of the survey process that make their work more difficult:
yes, increasingly so. Teams are being forced to do multiple complaint investigations during the LTC survey, which inhibits our ability to fully perform the other survey tasks. The Program management is now full of micro-managers which is very difficult when you work in the field. Our telecommuting program for deficiency writing has most recently come under fire, with supervisors now dictating how much time we will be permitted to write our deficiencies, which causes surveyors to be discouraged from citing for fear that there will not be enough time to write.
YES!!!! I am very discouraged as a surveyor due to social workers and dieticians are limited to a 40 hour work week. Depending on the type of facilities we survey and the size of the team we enter with this does not leave us enough time to follow every last protocol complete all task of the survey without rushing through the process. Then since we are on a strict time line we get asked why we missed something or why we do not have certain information in our deficiencies. In addtion, can not our regulations be computerize instead of taking several manuals. This can be hard on the older members of our team lifing all this books all the time. If we could have them on tablets with a hyperlinked index to the tags it would help greatly. In addtion, have a drug program or book on that tablet as it is now we only have one drug book per team. This would benefit the non nurses. Many surveyors create their 807's into tools that help them survrey easier and faster. If there are certain questions such as on disaster we must ask the staff than why cannot we have those questions already be on a form where there is much easier to reference. I think our documents need to be revampt to make it more efficient for the surveyors to survey with. We would not be needed to create our own tools if are documents included these items already.
New matrix/QMs are not helpful to the survey process. Too many categories to attempt to meet in Phase I- ie. WHPs, psych meds, all selected areas, interviews, etc…
We have a laundry list of tasks and so little time for observations. Decisions have to be made quickly and we have alot of evidence to gather. I would like to just concentrate on the categories flagged. Adapting to each facilities electronic records takes extra time.
I think we'd sometimes have better samples if we didn't have so much criteria. We may have to remove a resident that should be seem to fulfill a WHP or interview requirement. It's very hard with a small sample in particular to meet the WHP, interview and antipsychotic criteria. No with the QMs, it really limits your flexibility. I understand we can substitute and soforth, but it can still be quite challenging. When you have a heavy dementia population, 5 or more interviews can be difficult, and you sometimes have to make adjustments that may not result in the best sample.
Time is always a constraint. The use of a multitude of electronic record formats at different facilities often makes information retrieval difficult.
yes I think group does not need to be done. most of the time it is the only people in the facility that can give you an interview that come to group or they bring everyone just to put people in the room likes its an activity some times the council president does not even come and it is the same questions we ask everyone all the time
TOO MUCH FOCUS is spent on filling out the CMS forms, especially CMS-805 related to MDS. If one part of this sheet isn't filled out and there's a problem down the road, the first thing shared with us is, "Why isn't this filled out?" It's BUSYWORK and PAPERWORK when we could be observing!
Time constraints can often be a factor in some situations. Not all facilities are fast with retrieving paperwork and information when it is requested. Team leadership is becoming more time consuming with the continued expansion of the entrance conference list.
The Quality Indicator Survey (QIS) raises many concerns for Surveyors, chiefly related to what they see as its rigidity:
QIS is very limiting for new surveyors by keeping them too focused and as experienced surveyors it is very frustrating to input all those weights when you can look at them and see if the resident has had any loss
I am not certain that the QIS process is the best use of surveyor time – I spend more time investigating with no more citations – I am working harder for the same product and feel like I have the less knowledge base when making compliance issues.
Hard to say. We are behind in our survey intervals as are many states who have implemented QIS. We receive mixed messages all the time. "The survey takes the time it takes…" versus, "Get in there, get done and get on to your next survey!" Some facilities are ahead of the curve in doing what they can to reduce uneccessary use of antipsychotics. Others, not so much. Rural MD's can be very stubborn. The problem is complex. Or maybe not. If physicians prescribe appropriately there is NO PROBLEM.
It does seem that the QIS process is so focused and structured that it makes investigating any other areas without spending a lot of time. Given that surveys on an annual timeline, the luxury of time is not there.
The QIS survey process often selects care area investigations for stage two that could have easily been ruled out for investigation in stage one. For example: observations of bruises- a coherent resident could be asked how the bruises occured but the tool does not guide the surveyor to do a preliminary investigation. It only directs that the observation be documented. The "non-pressure skin issue" will then trigger for investigation when perhaps the coherent resident could have told the surveyor how the bruise occurred, such as a lab draw. An investigation for stage two would not be necessary.
The QIS survey process often selects care area investigations for stage two that could have easily been ruled out for investigation in stage one. For example: observations of bruises- a coherent resident could be asked how the bruises occured but the tool does not guide the surveyor to do a preliminary investigation. It only directs that the observation be documented. The "non-pressure skin issue" will then trigger for investigation when perhaps the coherent resident could have told the surveyor how the bruise occurred, such as a lab draw. An investigation for stage two would not be necessary.
Surveyors raise concerns about facility practices – bringing in consultants to intimidate surveyors, producing documents at Informal Dispute Resolution that were not provided during survey, attacking surveyors’ credentials:
Discouraged with facility's using all of their resources to get out of a cite rather that just fixing it. Also, several of the facility's have consultants that can interfere with normal routine and when survey is happening all of the managers are on the floor answering lights.
Facility's administration at times will attack the surveyors professionalisim to deflect from any wrong doing on their part; also facilities challenge surveyors qualifications to evaluate medications, as they are not physicians
I am not inhibited or discouraged, but some of the corporations must believe that by bringing in their "Corporate" people on the first day of the survey will intimidate us. This is not the case for most HFQE. We are simply not impressed and do our survey as if they are not there.
just the facilities who only care about money
Physicians are a particular problem for Surveyors when they write antipsychotic drug deficiencies:
Some of the physicians say the surveyors are taking away their ability to treat their patients.
mainly physicians they will tell us not to questions their orders
hard to say a doctor is wrong when you are not a doctor
Some Surveyors identify multiple challenges:
time is a constraint, especially when team members are ready to leave before you are. Sometimes workload is unequal. some members are not nurses and cannot investigate "nursey things". There is always the question of do you have enough or the right evidence. There are times when you know something is wrong but cannot prove it. Then you work yourself to death and have it deleted.
One manager recently ruled with an iron hand… every survey was to last for 5 days and every report was to be done in 5 days. Survey teams were scheduled to go out again whether they were done or not. We also have been working short staffed for years, and yet are pushed to do more in less time. QIS has really slowed down the survey process, and many of the areas seem unimportant to care and services to residents. (I only follow behind surveys with complaint investigations, but often wonder what the survey team reviewed, due to the severity of the complaint.)
One Surveyor used the question to describe her positive experience as a surveyor:
No, even after doing this job 23 years, I see the difference that the process makes. Just last week I cited a Facility for not getting dental care for a resident suffering extreme pain and Lymphadenopathy. The Facility somehow found a dentist to treat him that very day. The next morning he came to me with tears in his eyes, thanked me and told me that he knew it was due to my presence in the Facility. Sort of like the policeman with the radar gun – people slow down when they see them!
Your Observations Concerning Implementation of the “Partnership to Improve Dementia Care in Nursing Homes” Initiative
The project inquired whether Surveyors had observed both positive and questionable provider responses to CMS’s Partnership to Improve Dementia Care in Nursing Homes.
Question 43: Your observations concerning implementation of the “Partnership to Improve Dementia Care in Nursing Homes” Initiative.

Question 44: Add any details or comments you have for the items from question #43, above.
Question 44 contains several subparts asking whether Surveyors identify positive provider responses to the CMS Partnership Initiative.
A) [Do you observe providers] Doing better resident assessments (to understand residents’ customary routines, preferences, etc.)
Surveyors report that use of MDS 3.0 improved resident assessments and some surveyors, that some facilities, but not the majority, have improved assessments. Many surveyors see no change at all, expressing concern that assessment is, too often, an exercise of paper compliance:
they don't care about customary routines. It is about documenting to pass survey
they still are focused on filling out the form, not the answers
They are only doing the paperwork compliance
Still do not assess previous preferences for life prior to being admitted to the facility, such as bathing.
A common concern is that assessment information, even if better, is not shared with nursing staff:
Yes, however, this information is not shared from activity directors to the nuring staff
The informtion is obtained initally by the social worker but the SW is not involved in the day to day care of the resident and the staff providing day to day care do not read the assessment nor are they aware of the residents' customary routines or preferences.
Social has been doing these but I am not sure if the other staff are aware of these previous routines.
They are doing better assessments, but I don't always see this incorporated in the overall plan of care.
it is completed but not followed
B) [Do you observe providers] Doing better care planning
Although 206 Surveyors indicate that facilities are doing better care planning, most of those who expanded on their answers report either that care plans are “canned,” computerized, and not individualized or that direct care staff are not informed of what the care plans say:
again, only do it to pass survey. no one looks at careplans.
they are often computer generated and generic
Alot of facilities use the "canned" care plans, where they indicate the concern and the computer fillsin the rest. Not individualized.
still see mostly canned care plans
Yes, but this information is not readily shared with the CNA's who provide the care.
Care planning has declined in the past few years with many facilities using care plan programs
Facilities seem to be all about paper compliance
still see non-personalized care plans
Care planning is done by non-direct care licensed staff. Care Plans are usually done by the MDS coordinator or ADONs who do not give the day to day care. Many are non-individualized care plans out of a text book or company program.
cookie cutter care plans – do non usually address non-pharm approaches or individualize
care plans are still cookie cutter and lack individualization
Care planning is an area of improvement. Most of its just paper compliance, and it's not used as a working tool
remains a paperwork issue
care plans have not gotten very much better overall in some facilities care plans are not reviewed by staff that provide the direct care.
Care Plans are better. CNAs often still do not know what the care plans say for each individual resident.
A small number of Surveyors describe significant improvements in care planning:
Some facilties are doing better care planning but it is rare
have noticed some improvement in this area at some facilities
More individulalized care plans.
C) [Do you observe providers] Involving resident and families in decision-making about the use of antipsychotic drugs
Although 209 Surveyors see more family involvement in decision-making about the use of antipsychotic drugs, most of those who wrote detailed responses do not. Surveyors see signed consent forms, but little evidence of meaningful family participation.
Most families I have talked to are not aware of any of the side effects or indications for the emd. They just figure if the doctor ordered them they must be necessary
The facility usually calls doctor with S/S and then facility calls and gets consent from families. There is very little pre-planing with families on when to call the doctor for a S/S that an antipsychotic may be needed.As with dementing illness with associated behavior symptoms, there is very little non-pharmallogical intervention tried before the doctor is called.
ive seen more consents from family about the use of antipsychotic med use
yes – consent forms are signed
Many times the resident is not cognitively alert enough to make those decisions and the family or responsible party is not knowledgeable enough and accepts whatever the staff tell them. Examples include statements such as "The doctor ordered Ativan for anxiety" when the residents just needs one-to-one contact from staff or family to adjust to a strange enviornment..
Usually just inform that it will be done. Rarely have I seen a RP deny the use
Starting to see more evidence of this (not just the near meaningless "informed consents")
Have not seen where a resdient or family member is involved about the use of antipsychotic drug. It is addressed in care plan usually after the medication has been started.
I think this is lacking. Some places will have consents, but it's my understanding that this isn't required. I think consents for such medication use should be required. At least that way you know the family/resident/DPOA, etc. received some information r/t the impact of the use of these meds.
not enough participation
This is probably the biggest thing I see lacking.
D) [Do you observe providers] Making consistent assignment of staff to residents
Again, although 206 Surveyors report use of consistent assignment, most of those who wrote detailed responses describe staff rotation as the predominant facility method of assigning staff. Some Surveyors comment on the inadequate staffing of facilities. Surveyors who see consistent assignment report on the positive effects for resident care.
Staff rotation the norm:
Most facilities still rotate the staff, especially if there is a call-off in another unit. They go by seniority, not experience dealing with dementia cases.
Many facilities still rotate staff
Many facilities rotate staff and the direct care staff do not know the residents likes and dislikes. Staff are not knowledgeable enough about dementia or mental problems.
Some facilities still rotate staff to prevent burn-out
Inadequate staffing levels:
There is such a staffing shortage, this is all but impossible
The staffing and turnover is a statewide problem, very few places have consistent staff because of this.
to them I think a body is a body
Soem facilities do not have adequate staffing and utilized pool or agency staffing. So there is limited consistency in staffing.
Due to staff shortages this is not routinely possible.
They usually are short staffed as it is so consistency is not a priority.
Positive benefits of consistent assignment:
Have seen this in many of the homes and it seems to help with those residents with dementia, seeing those familiar faces.
More facilities are trying to do this and I do believe is has a positive impact
do like to see this. These staff know their residents then. Do see more turmoil and complaints when facilities switch staff around to different halls.
more facilities are doing this which is helpful especially with dementia residents
this would greatly improve resident care
helps residents familiarity with staff and lessens anxiety
consistency helps staff and res know each other better
E) [Do you observe providers] Responding to Consultant Pharmacists’ Recommendations
Two Hundred seventy two (272) Surveyors see facilities as responding to consultant pharmacists’ recommendations, 67 do not. Many report that they cite this issue and that it is an area of improvement. However, physicians are still often a problem.
this is difficult as the doctors still feel that we are telling them what meds to order
There is some evaluation and response by the physician, but rarely
facilites don't seem to track the physician response, and don't seem to question the physician if no rational for no GDR indicated.
getting MDs to response to pharmacists a problem
Yes, this is being done; however, PCP's and psychiatrists are not doing this themselves to the extent they need to do.
most physicians will not take recommentations
Appears that facilities' consultant pharm. taking a more proactive role.
needs to be more timely response from physicians
Many facilities do not advocate for the recommendations. Once the pharmacist makes a recommendation, the recommendation is faxed to the physician and that is it. Many staff are not even aware of the recommendations.
For anything that does not require a MD order – good. A few of the newer MDs are more receptive to pharmacist's requests
Physicians simply write "benefits outweigh risks"
Usually not all doctors comply sometimes there is a system breakdown within the facility.
they have been getting better about this for several years
Most have had DRR…the problem is in the follow-through…facilities ether do this well, or they don't
Many homes try and then a physician is the one who is disagreeable. Would like to see physicians trained with this too.
doctors need to be held to the regulation and actually document why a medication can not be considered for GDR
Still some resistance from MD's but most acknowledge the recommendations.
Physicians are slow learners.(slow to change would be more polite).
nursing is taking a more active role in supporting the pharmacist requests.
F) [Do you observe providers] Addressing antipsychotic drug use in quality assurance or QAPI
Two hundred twenty four (224) Surveyors answered that they see facilities addressing antipsychotic drug use in quality assurance or QAPI, although some question the effectiveness of those mechanisms. In their additional comments, some Surveyors note, correctly, that they are unable to review facility QAA committee notes. Some think that QAPI could be a good review mechanism.
Using QAA or QAPI
In my opinion, most QAC's do not have a goal of reducing antipsychotics except through GDR in pharmacy consultant review.
Most QI committees review the number of residents on the meds and if there have been any additions, etc. Again, facilities have always looked at the numbers on the MDS, I see very little result from these meetings
routine quarterly reviews just to meet requirements
more QAA on falls and not enough on drugs
Yes. Incorporated into QA meetings.
In fact, just a week ago I did see where a facility had taken it upon themselves to do a complete review of their antipsychotic drug use.
most already do b/c of the initative
Unable to review facility QAA notes
we are not able to see the minutes of the QA meetings and can only go on what the facility chooses to tell us
Don't ask this specifically in the QA task unless there is a problem r/t antipsychotic use.
They tell me that they discuss it but if I can't look at their program……
G) [Do you observe providers] Increased staffing/training
One hundred thirty three (133) Surveyors answered yes, 210 no. Surveyors who explained their responses were most likely to report more training, rarely, if ever, more staffing. Some Surveyors reiterate the need for more staffing and others express concern about facilities’ reimbursement rates.
More training, not more staffing:
Increased training r/t CMS initiative. Questionable impact on staffing numbers.
Increased training, but not really staffing.
Seldom have seen in-services for psychoactives and staffing does not take into account extra needs of resdients.
training-yes, staffing -no
Training increased in some facilities.
still seeing the "minimum" for both
training increase but not staffing
I have seen increased staff training. Not increased staff numbers.
Increased training, but still resist increased staffing/budgeting
Increased training for dementia because they "had" to.
Reimbursement:
In my opinion, budgetary restraints are reducing staffing, not increasing it.
It doesn't happen–profit is the bottom line
training yes, but c/o about less medicaid funds.
More staffing needed:
all facilities need to increase staffing and i feel that the Feds need to dictate # of staff
it should be an actual requirement
a body is a body… need higher staffing levels
staff is and will always be an issue in LTC. the families and the resident expect more and then call in complaints because they don't understand how the facilities staff.
Not going to happen unless minimal staffing requirements are enforced by CMS.
STILL NEED TWICE THE NUMBER THEY HAVE
Staffing will never be a premium with Illinois.
H) [Do you observe providers] Other
CMS has no dementia regulations. That's all surveyors can hold facilities to is meeting the minimum standards. We have no dementia regulations. CMS needs to get some dementia regulations if they want to hold facilities to dementia care standards.
one of the above will occur even sporadically unless pressure is placed on the homes and survey agencies.
With all of the above, some facilties are doing a better job but some still are not. I feel there still needs to be more training and an increase in the mandatory staffing requirement for direct care staff.
Question 45: Have you observed questionable provider responses to the Initiative.

Question 46: Add any details or comments you have for the items from question #45, above.
Question 46 contains subparts asking Surveyors to elaborate on whether they observe questionable provider responses to the Initiative.
A) [Do you observe providers] Performing inaccurate assessments
Surveyors generally do not describe the Initiative as the cause of the inaccurate assessments they see:
sometimes assessments are done only for MDS purposes and are not "ongoing" with the resident
in depth assessments just recite MDS. CAA summaries are not in depth.
Only one person, sitting behind the desk using the chart to do the assessment
documentation of behaviors is lacking. How can they assess if they are not monitoring
Assessments are done qucikly and mistakes are made
More like poor or no assessments
nursing staff are not as prepared to asess differences between psychosis and dementia.
To fit they need they desire
Many times the assessments are not documented just the diganosis.
At times they are incomplete and do not truly reflect the whole history of the resident including diagnoses and reasons for GDR's or no GDR's
assessemnts are not always accuarate
More incomplete or assessment by LPN and RN signs
The assessments are cookie cutter
out of haste more than deceit
B) [Do you observe] Falsification of records
Several Surveyors report that it is difficult to prove falsification that they suspect; others identify specific methods of falsification and the absence of consequences to facilities:
There is no deterrent; a facility suffers more from a quality of care deficiency with harm than from the potential risk of a documentation citation. There should be mandatory monetary and licensure ramifications when the altering of medical records can be proven (i.e. pre-/post- copies).
Methods of records falsification
Yes especially when they are cited for it and then IDR it and provide false info.
sometimes the documentation doesn't match the behavior
Unfortunately, we have seen a lot more of flagrant falsifying lately.
Finding documentation after the fact . Changing dates of forms after we have them copied or adding information after we have already reviewed the forms. Also having forms signed and backdating like on authorizations to give psy. medicaitons.
Behaviors not documented by staff "he always does that"
This occurs on occasion for different aspects of care in some facilites. it is important to make copies beforehand of documentation in order to support deficiencies.
adding interventions
Have known there to be no behavior documentation only to turn around and have it miraculously found…..
We are forced to make copies early on as some have changed medication documentation according to original surveyor notes
Difficult to prove falsification of records
This is hard to prove but if we question something the physician will side on the facility's defense.
C) [Do you observe providers] Switching residents to other (non-antipsychotic) psychoactive medications
Surveyors most frequently identify Depakote, followed by anti-anxiety drugs and others. Surveyors again describe challenging physician behaviors.
Other drugs:
Everyone's on Depakote now.
Vistaril, phenergan, and benadryl are frequently used for sleep property S/E when an antipsychotic or hypnotic may have been used in the past. CMS used to be really into curbing hypnotics. Why not put more emphasis on defining parameters in which doctors can prescribe hypnotics/anxiolytics medications in the elderly?
use of more antianxiety medications
Yes, usually the anti depressants are tried
see more mood stabalizers
depakote, anyone?
Some switching has occurred in the past to items like depakote and lorazepam. Some new ones now are nudexta of namenda/aricept
anti-anxiety and hypnotics
yes, like Ativan or antidepressant med
off label use, (phenergan, neurontin, anticonvulsants)
wean off a medication too soon then start another then back; hard on the resident
depakote has been used extensively in place of antipsychotic meds
Most often anti anxiety meds
SNFs try mood stabilizers such as depakote thinking the regulation does not apply to that class, but it does.
Physicians:
again the MD doesn't want us to tell them what to order
Doctors will do whatever the nurse that called them asked for.
D) [Do you observe providers] Failing to determine appropriate gradual dose reductions
Surveyors report that pharmacists are generally doing a good job, but that physician resistance prevents GDR from actually occurring. Several Surveyors report that GDR is not done at all.
Physician resistance is a common theme:
physicians don't want to reduce medications, write resident is stable or write "clinically contraindicated" with no further information.
Not gradually decrease, but abruptly discontinuing or halving a dose. This sets the resident up for failure.
Some of the physician's just state "no GDR at this time" with no rational or no documented failed attempts. No documentation on behaviors which are occuring.
They are identifying them, but the physician will document clinical contraindication.
doctors do not always want to fully document rationale for refusing GDR other than benefits outweigh the risks
Sometimes they will just say that it is not apprpriate due to the lenght of time someone has been on one
I have observed some psychiatrist just refuse the recommendation rather than provide the rationale for refusing the recommendation.
Still see a fair amount of poor response to pharmacy recommendations for GDRs.
Some facilities not reducing medications as indicated or documented reason why contraindicated
Usually they have their Pharm consultant making these recommendations. They don't always address them tho.
MD says no GDR-no explanation an d thst fine
because the physician always checks no when pharmacist makes recommendation
physicians will still decline
this is physican resistence. Pharmacist are doing there job for the most part
md just writes will decompensate
E) [Do you observe provders] Failing to adjust staffing levels, when necessary
Several Surveyors report that facilities will implement one-on-one staffing, when needed, but most used the question to reiterate the inadequate staffing levels that they see.
sometimes the facility will provide one to one staffing with a resident who is at risk for harm but have not noticed any staff adjustemnts based on antipsychotic drug use
More will assign 1:1 in unsafe circumstance.
I rarely see this occur unless a resident needs a 1:1
Yes especially when they knowingly admitted residents to a faciltiy with problem behaviors that require more staff supervision and care and only adjust when cited or a negative resident outcome occures.
How are we to determine adequate staffing when we are not privy to the staffing before the adjustment was or was not made
Surveyors report insufficient staffing
it is all about #s
no difference in staffing levels even for specific dementia care
They never seem to have enough aides.
No staffing levels are adjusted, facilities function on the limited available staff at hand and most of the time barely meet the minimum requirements
On the contrary, finding staff to do the job in rural areas is a problem. Some facilities work short-handed or make ADON's or DON's fill the shift, which causes burnout and vacancies.
Not seeing adjustment of staffing levels
yes weekends are the worst
As long as they are meeting minimum staffing they feel they have met thier obligation
yes, I think many homes are unable due to budget constraints to increase staffing when needed.
staffing is an issue in most facilities no matter what
Nursing facilities may increase staffing levels while the survey team is present. DONs have commented on this but the administration or facility corporate policy for staffing is very limited.
most facilities still have inadequate staffing
At times in facility's that are short staffed routinely.
the corporate tells us how many we can have is the normal response, they also determine the number by LVNS, CMA and CNA combined. THe number of CNA's needs to be determined alone as they are usually the ones who do the most work . This would eliminate having (for example) 3 LVNS and 2 CNA's for 70 residents maybe
can always use more staff
Usually if this is seen, it's when a resident is really acting out…don't always one:one them…staff just has to manage…although I believe more facilties are looking at this.
Staffing stys the same. but there is an increase in psych residents
Rely on direct care staff who already have responsibility for transfers and cares requiring two staff to monitor residents who are exhibiting behaviors
staffing is big concern in our homes even for care. leads to increased staff turnover
They are usually short staffed anyway.
facilities are always looking to keep costs down which is done by lowering staff numbers
Adminstrators at corporate levels don't work in dementia with behaviorial issue units. They are clueless for the most part
Most places are "overstaffed". Mandate staffing levels.
I think it is the one thing they are always most hesitant to do, And it is the one thing that is most effective.
staffing protocols seem to reamain consistent, industry wide
Do not want to increase their cost
F) [Do you observe provders] Reducing antipsychotic medications when they are truly necessary and appropriate
Some surveyors observe this practice; others do not.
yes, and then some residents have a relapse
I have witnessed a reduction in medication resulting in adverse behavior that caused harm to another resident – someone who needed the antipsychotic meds and was reduced according to CMS guidelines and they acted out. BUT! I have seen where medications were increased and perhaps were the cause of a fall that injured the resident. It goes both ways.
Fear of a citation if not done, whether meds are approprite or not.
Antipsychotic medications should be reduced in residents that are bedbound and severly cognitively impaired because these medications may not be truly necessaary or appropriate.
Sometimes, accordingb to staff
Physicians will disagree with a pharmacist and not give an explanation as to why, just that the resident will have a psychotic episode if medication is decreased.
still seeing a problem with this in some facilities
Yes, it happens. Restoring the dosage often does not get the same effect as before you decreased the dose.
occ. see this just to do a GDR and has caused distress on the resident
facilities reduce medications because they are afraid of getting tagged.
G) [Do you observe providers] Creating a new, but false, diagnosis of psychosis
Some Surveyors ask how they can question the physician; others suggest that false diagnosing is difficult to prove.
False diagnosis:
Pharmacists are giving the doctors a list to check off a diagnosis so it will meet the regulation."Pick one any one."
sometimes happens during the urvey to try to make the deficiency "go away"
Yes, "Dementia with psychotic features"!!!!!!
If you cite them for not having an appropriate diagnoses, they will have the diagnoses before you leave the facility, even without seeing psychiatry.
Sometimes I question this diagnosis in an elderly person who never had this diagnosis before and am unclear what psychosis the facility is seeing in the resident.
This is a consistent issue, physician adds diagnosis to justify the medication, mostly the meds are for staff convience.
Have seen multiple requests from pharmacist for dignosis for the medications given and after 3 or 4 requests doctors given a generic diagnosis that may or may not be relevant to the resident.
Have seen requests by pharmacists to MD asking for diagnosis for a medication and then seeing a diagnosis which has not ever been mentioned in resident's diagnosis history
They call the MD and say state's here we need a diagnosis of psychosis and over the phone he/she gives it. Just like cathethers and urinary retention all ove the phone with no assessment
Physicians will add a diagnosis of psychosis to justify some medications.
when MD want to use aP they add DX psychosis for pts with agitation
I see the diagnosis dementia with psychosis alot, but it is unclear what the psychosis refers to. Alot of times it is coined as delusions, when the resident has dementia and should be expected to have some cognitive issues and persistent thoughts/issues
Sometimes, diagnosis written after med ordered and given
Questioning a physician:
A surveyor reviewing the facility's clinical record of a resident over one to four days in no way can provide that person's true history. It is not possible to question a physician who has treated this resident for years.
How do I know if it's a false diagnosis? Only a doctor can diagnose. If the physician says it's a diagnosis then it is.
How are we to make such a determination? It is ouside our scope of practice
Feel as long as there is a supporting diagnoses, this is appropriate to give the med and control the behavior
Difficult to prove:
yes, but difficult to prove, since we cannot diagnose
Not that I can prove.
Not sure I would know if it was false.
difficult to prove, but sometimes appears to be so
I can't prove it but have been Highly suspicious this has happened or will happed
I can't prove this but I'm sure it happens at times.
I would need guidance on how I could prove a diagnosis written by a doctor to be false.
he facility will usually dig thru old records to find documentation of psychosis or get a new drs order
Since we don't diagnose, we need to question at times and look for reasons
been citing exactly this lately Got to have the symptoms to make a diagnosis
Psychiatrist notes will include the diagnosis so it matches
Very hard to prove
This happens frequently even with PAs
Creative writers.
no one seems to understand what this is. Use it for everything. Am citing this if no doc.
sometimes, mental health providers will depend on staff interviews and not direct observations of residentt 'behaviors, for permanent diagnoses that are not accurate. Staff does not always attempt other interventions before reporting this to physicians or psychiatrists'
This leads to additional investigation to determine who and when was the dx made and what was the evidence to come to that dx. Just more questions for the surveyor to ask.
Question 47: Have you cited more F329 and related deficiencies since the Initiative began?
More than two-third of Surveyors (241 of 345 Surveyors who responded to Question 47, 69.86%) have not written more deficiencies since the Initiative began; 30.14% (104 Surveyors) have.

Question 48: Is the scope/severity at which you are citing these deficiencies lower, the same, or higher?

Question 49: What has primarily caused you to make the changes noted in questions #47 and #48, above?
As their primary reason for changes, most Surveyors describe the CMS initiative, the new focus on antipsychotic drug use, surveyor training, or greater awareness of the problem.
New Focus (Yes to Question 47, same to Question 48)
increased reviews of antipsychotic (Yes same)
More focus is on F329 (Yes same)
Increased awareness of CMS requirements. (Yes same)
More attention, and the fact that we automatically pick at up least 4 residents with psychoactive medications on each sample now. (Yes same)
Looking more closely at the tag and the justification for the usage of the medication. (Yes same)
Closer investigation of residents' drug regimen (Yes higher)
paying more attention to the details (No higher)
greater focus and recent training (Yes higher)
Looking at this protocol a lot closer now. (Yes higher)
improved support from CMS for citing and most facilities are on board and understanding of deficient practice identified. (Yes same)
Spending more time on the unnecessary medication investigations. (Yes same)
Ensuring more residents on psychoactive medications are included in the phase one sample (No same)
Better understanding of how CMS wants the tag cited. (No higher)
Has become more of a focal point. (Yes same)
The mandate to focus attention on this concern. (Yes same)
Learning more about unnecessary drugs at this time. (No same)
The regulation initative (Yes same)
more aware of process, have developed a strategy to fully examine this area (Yes same)
awareness (Yes same)
We are looking at medications closer. (Yes same)
looking more closely since reviewing training. (No same)
Increased awareness and guidance. (Yes same)
being trained on the initiative and citing other tags along with F329 that we previously had not been citing (Yes same)
more guidance (Yes same)
More clarity. (Yes same)
More aware of F329 due to intiative (Yes same)
More information by CMS regarding Antipsychotic medications (No same)
Changed priortity to look closely at drugs, dose, indication, and more staff interviews. (Yes same)
It has been targeted as an initiative and we have had more focus and training on the tag. (Yes same)
Awareness of the negative outcome to residents. (Yes same)
new expectations (Yes same)
More information from CMS (Yes same)
More of a focus required by the SOM. (Yes same)
Better understanding and awareness of the issue. (Yes same)
As you learn your evaluation of a situation is enhanced (Yes higher)
More aware and more defining of what the facilities are to do in the tag. (Yes same)
A significant number of Surveyors report that facilities are themselves giving more attention to reducing antipsychotic drug use in their residents. Consequently, Surveyors have not increased deficiency citations for misuse of the drugs.
I believe the facilityies are educated and really trying to reduce the use on antpsychotics (No same)
heightened surveyor awareness, increased provider (NF/SNF) awareness making for fewer arguements when we do cite (Y same)
Facilities are more aware of CMS guidelines as it concerns psychoactive medications. (No lower)
the facility is making an effort to monitor residents on anti-psychotic drugs (No lower)
There appears to be a reduction in the use of antipsychotics in the facilities i have surveyed (No same)
facilities are following the initiative and it is working (No lower)
Some Surveyors report that they or their state cited antipsychotic drug deficiencies in the past and were ahead of CMS’s Initiative.
Again, my region has been ahead of CMS in this one thing. (No same)
Antipschotic / psychoactive medications has always been a focus for me. I think it is a very important category to look at during each survey. The resident can be very negatively affective by unnecessary medications. (No same)
Have cited this tag for a long time. I have extensive long term care experience as well as both regular psychiatric and geri psyche experience. I don't understand why some of these 90 year old people with dementia need antipsychotic medication. There are too many other medications that can be tried. Also CMS needs to acknowledge that there are antipsychotic meds that are used for other purposes and the MDS process does not allow for the rationale for the use of a medication (if that is where the numbers come from) (Yes same)
this has always been a concern. (No same)
I believe we were always looking at this area since it can have such a significant impact on the resident. Can't say I see much difference in what we do or how we cite….facilities are making efforts, but they still have a long way to go, especially as it relates to behavior documentation and follow-up after the use of PRN meds for behaviors. (No same)
My survey teams have not changed. They have always cited F329 for psy and other classifications of medications (No same)
Some surveyors explain why there have not been changes in antipsychotic drug use:
I don't see a lot of difference in what the facilities do. They have their consultant pharmacist look at the psychotropic medications and make recommendations and the physician responds. Sometimes they agree and sometimes they don't. If the physician does not agree I do not see what we can do. The facilities and physicians sometimes feel they will cause more harm to the resident by reducing certain medications when a resident has been stabalized on them. (No same)
the facility just do not seem to share the concept that there are more interventions then just increasing antipsychotic medications for relief….benefitting staff vs resident. (Yes same)
Team members and enforcement members say that monitoring is only a paper tag and we don't do paper tags. (No same)
Nursing staff are often unaware of the initiative. (No same)
Not wanting to overwhelm the facilities. (Yes same)
We are not qualified to diagnose and treat residents. I still believe the MDs are the ones who hold the key to psych med reduction. (No same)
One Surveyor describes how the antipsychotic drug deficiency she cited was dropped:
Last time I got to cite F329 was July 2012, have tried once since then and tag got dropped. (No same)
Two Surveyors who believe the Initiative will be ineffectual describe the F-tag as not strong enough and the guidelines as “too subjective.”
Toby S. Edelman
Dean Lerner
June 27, 2013
[1] The Affordable Care Act requires all facilities to implement Quality Assurance and Performance Improvement (QAPI) and, as part of QAPI, to develop and implement specific Performance Improvement Projects (PIPs). CMS has not published regulations, but has given informal guidance to facilities on QAPI. CMS, “Rollout of Quality Assurance and Performance Improvement (QAPI) Materials for Nursing Homes, S&C: 1-37-NH (June 7, 2013), http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-37.pdf.
