- Dismantling the Affordable Care Act Would Harm Medicare and Medicare Beneficiaries: Spotlight on Medicare’s Financial Stability
- Provider Relief Funds: Care for Patients or Boosting Provider Revenues?
- Utah’s Crisis Standards of Care: Discriminatory Medical Rationing
- Infection Control Surveys At Nursing Facilities
- 2020 National Pro Bono Week
The Supreme Court will review the constitutionality of the Affordable Care Act (ACA) this term in California v. Texas, with oral argument scheduled for November 10, 2020. This ongoing litigation challenges the ACA’s individual mandate, but raises questions about the entire law’s survival, and could result in dismantling the entire ACA.
While the ACA’s changes to the individual insurance market and its expansion of Medicaid have been the focus of much media coverage, the law has affected every part of the health care system, including Medicare. The ACA is woven into Medicare, with over 165 provisions affecting the program. Many of these provisions help beneficiaries and strengthen Medicare’s financial well-being. Striking down the ACA would have disastrous ramifications for Medicare beneficiaries and the U.S. health care system as a whole. In a series of CMA Alerts leading up to the Supreme Court oral argument, the Center is highlighting some of the harm that undoing the ACA would bring to Medicare and Medicare beneficiaries.
The ACA strengthened the long-term financial stability of the Medicare program, improving the program’s sustainability. This was accomplished in part by reducing excessive payments to private Medicare Advantage plans, bringing those payments closer to the average spending for beneficiaries in traditional/original Medicare. Dismantling the ACA could thus eliminate those savings and increase Medicare spending by approximately $350 billion over the ten years of 2016- 2025. This would accelerate the insolvency of the Medicare Trust Fund.
Undoing the ACA would jeopardize these fiscal gains and harm Medicare’s long term financial stability. At the very least, it would cause fiscal and administrative chaos in the health care sector as an entire payment system would be thrown into uncertainty. The Center for Medicare Advocacy strongly opposes dismantling the ACA and the lawsuit that seeks to do so on unmerited grounds. The Center joined AARP and Justice in Aging in submitting an amicus brief in support of California and the other states defending the ACA against the lawsuit now at the Supreme Court. The brief highlights the ACA’s key protections for older adults and the devastating consequences that would ensue if the law is nullified.
Additional Resources:
- Kaiser Family Foundation, “Potential Impact of California v. Texas Decision on Key Provisions of the Affordable Care Act” (updated September 2020).
- Center on Budget and Policy Priorities, “ACA Repeal Lawsuit Would Cut Taxes for Top 0.1 Percent by an Average of $198,000, Weaken Medicare Trust Fund” (October 2020).
- Congressional Budget Office, “Budgetary and Economic Effects of Repealing the Affordable Care Act,” (June 2015), analysis in response to Congressional ACA repeal efforts: “CBO and JCT cannot anticipate with any certainty what choices federal agencies would make to implement such legislation to repeal the ACA. Medicare, for example, would be affected in several fairly complicated ways. In many cases, the program’s payment rates reflect base payment amounts that are increased or updated each year according to formulas specified in law. The ACA reduced those updates, and repealing the relevant provisions would clearly cancel the reductions that are currently scheduled to take place in future years. The complication that arises is that the base payment amounts to which the updates will apply are currently lower than they would have been had the ACA never been enacted. If the ACA was repealed, it is unclear whether those base amounts would be adjusted upward so that future payments would not be affected by past update reductions. In other cases, repealing the ACA would require payment mechanisms for Medicare to revert to those used under prior law, but the Department of Health and Human Services (HHS) would need to decide how to calculate those payments once the law was repealed. (Legislation to repeal the ACA could reduce the scope of such discretion, however, by specifying the manner of restoration or revival of the provisions of prior law.)”
- Kaiser Family Foundation, “A Primer on Medicare: Key Facts About the Medicare Program and the People it Covers,” (March 2015).
- GAO Report, “Continuous Insurance before Enrollment Associated with Better Health and Lower Program Spending,” (December 2013).
- Center statement concerning the fate of the ACA in light of Supreme Court nomination hearings (October 2020).
– top –
Provider Relief Funds: Care for Patients or Boosting Provider Revenues?
Despite nursing facilities’ reporting severe shortages of nursing staff and personal protective equipment,[1] the Department of Health and Human Services (HHS) has revised federal policy to allow health care providers, including nursing facilities, to apply Provider Relief Funds (PRF) to revenues lost during the pandemic “without limitation.”[2]
The Coronavirus Aid, Relief, and Economic Security (CARES) Act[3] created a fund for providers dealing with the coronavirus pandemic. As described by HHS, Provider Relief Funds, whicheventually totaled $175 billion, are required to be used
to prevent, prepare for, and respond to coronavirus, domestically or internationally, for necessary expenses to reimburse, through grants or other mechanisms, eligible health care providers for health care related expenses or lost revenue that are attributable to coronavirus.
HHS has issued multiple instructions and guidance documents setting out federal policy on how health care providers can spend PRF. Guidance issued September 19 prohibited providers “from using PRF payments to become more profitable than they were pre-pandemic.” The most recent guidance, issued October 22, explicitly reverses that September 19 policy.
Responding to concerns raised by “stakeholders and Members of Congress” that “PRF should allow a provider to apply PRF payments against all lost revenues without limitation,” HHS revised its policy and “amended its reporting instructions to provide for the full applicability PRF distributions to lost revenues.” In other words, instead of using Provider Relief Funds to hire desperately needed staff and to purchase essential personal protective equipment, providers are free to use the remaining $35 billion of PRF to compensate themselves for “lost revenues” that are attributable to the pandemic.
In the middle of an ever-worsening pandemic, it should go without saying that Congressionally-appropriated funds must be devoted to the care of patients and their caregivers, not to boosting providers’ bottom lines.
More than 84,000 residents and workers at nursing facilities have died of COVID-19, 38% of all deaths in the United States.[4] Sufficient staffing and personal protective equipment are key to preventing or slowing the spread of COVID-19 in nursing facilities. The billions of public dollars available through the CARES Act must go to protecting public health and the public good.
___________________
[1] Brian E. McGarry, David C. Grabowski, and Michael L. Barnett, “Severe Staffing And Personal Protective Equipment Shortages Faced By Nursing Homes During The COVID-19 Pandemic,” Health Affairs (Aug. 20, 2020), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.01269; Peter Cox, “Minn. Nursing homes in rural areas see staff shortages worsen with COVID-19,” MPRNews (Oct. 26, 2020), https://www.mprnews.org/story/2020/10/26/minn-nursing-homes-in-rural-areas-see-staff-shortages-worsen-with-covid19; Shahla Farzan, “Pandemic Worsens Staff Shortages At St. Louis Nursing Homes, Putting Residents and Workers At Risk,” St. Louis Public Radio (Oct. 9, 2020), https://news.stlpublicradio.org/2020-10-09/pandemic-worsens-staff-shortages-at-st-louis-nursing-homes-putting-residents-and-workers-at-risk.
[2] HHS, “Reporting Requirements Policy Update” (Oct. 22, 2020), https://www.hhs.gov/sites/default/files/reporting-requirements-policy-update.pdf.
[3] https://www.congress.gov/116/plaws/publ136/PLAW-116publ136.pdf.
[4] “About 38% of U.S. Coronavirus Deaths Are Linked to Nursing Homes,” The New York Times (Oct. 20, 2020), https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html.
– top –
Utah’s Crisis Standards of Care: Discriminatory Medical Rationing
What seemed unimaginable in the United States a few months ago may begin soon in Utah: rationing of access to critical life-saving medical care. This dire situation comes due to surging COVID-19 cases coupled with limited medical supplies and staff at hospitals in the state. As if it were not devastating enough that some deathly ill patients may be denied life-saving treatment, the Center for Medicare Advocacy has found that Utah’s criteria for making these determinations illegally discriminate against older adults in violation of the Age Discrimination Act of 1975 (Age Act) and Section 1557 of the Affordable Care Act.
According to news reports, hospital administrators in Utah have alerted the Governor that if virus cases continue to climb, hospitals will not be able to treat all patients – they will need to activate rationing criteria, which they expect to do within the next week or two.
Under Utah’s “criteria,” or Crisis Standards of Care, a medical provider who assesses two patients to be in the same health status can use age as a tie-breaker to determine which one of them receives access to lifesaving care when there is only enough to treat one patient. If the standards are approved by the Governor, then in a scenario where the patients’ conditions are considered “equal” after certain health factors are taken into account, the provider can use age as a tiebreaker to deny care to the older patient.
Since the pandemic began, the Center for Medicare Advocacy has been involved in a coalition effort, along with disability rights advocates and advocates representing older adults, to ensure that decisions to ration treatment are made without discrimination based on disability or age.
In September, the Center joined colleagues at Justice in Aging and the American Society on Aging in opposing HHS Office of Civil Rights endorsement of Utah’s standards as discriminatory against older adults in violation of the Age Act and Section 1557. To fairly allocate scarce medical resources, such as ventilators, guidelines should look to an individualized assessment of short-term mortality risk from the acute COVID-19 infection, not long term mortality. It is shameful to deny treatment to older adults, based solely on their age, embracing a value system in which an older person has less societal worth.
As stated in our joint letter:
One major goal of a CSC [Crisis Standards of Care] is to ensure decisions surrounding scarce resource allocation are made based on an individualized, clinical assessment of the patient and without discrimination.. . .The tiebreaker provision will work to prevent an older patient from receiving care in favor of a younger patient with a similar … individualized assessment. In that instance, the biased age-based tiebreaker would give preference to the younger person outside of any individualized factors. To avoid bias, tiebreaker provisions in crisis standards should not be based on generalized assumptions that an older individual must have worse mortality outcomes. . . .The tiebreaker language in the Utah CSC inexplicably denies critical care to the very people these [COVID-19 mitigation] efforts were meant to protect – those most at risk of dying from COVID-19 complications.
Resources:
- New York Times, “In hot spots around the country, hospitals are reaching their limits.” https://www.nytimes.com/2020/10/25/world/in-hot-spots-around-the-country-hospitals-are-reaching-their-limits.html
- Salt Lake tribune, “Utah’s hospitals prepare to ration care as a record number of coronavirus patients flood their ICUs” https://www.sltrib.com/news/2020/10/25/with-coronavirus-cases/
- Letter to Office for Civil Rights: https://justiceinaging.org/wp-content/uploads/2020/10/Utah-CSC-Ltr-to-OCR-2020-09-02.pdf?eType=EmailBlastContent&eId=cdfa7cc7-1b95-4e08-aa9b-eb3b463bf054
- Center for Medicare Advocacy Update: Medical Rationing: https://medicareadvocacy.org/advocacy-update-medical-rationing/
– top –
Infection Control Surveys At Nursing Facilities
More than two months ago, on August 14, 2020, the Centers for Medicare & Medicaid Services (CMS) reported that it had cited more than 180 “immediate jeopardy” level deficiencies for infection prevention and control at nursing facilities, triple the rate from 2019, and that it had imposed civil money penalties exceeding $10 million for the deficiencies.[1] CMS acknowledged in a call with nursing home residents’ advocates on August 19 that the data reported on August 14 were available only in an internal CMS database, not on its two publicly-reported databases.
The Center for Medicare Advocacy (Center) analyzed data on CMS’s Quality, Certification and Oversight Reports (QCOR) database, which CMS updates weekly, and reported on August 20, 2020 that QCOR data showed far fewer immediate jeopardy deficiencies in infection control than CMS reported.[2]
Now, two months later, the Center has analyzed QCOR data and again found inaccuracies in the database and far fewer than 180 immediate jeopardy infection control deficiencies.
| Why do infection control deficiencies matter? Failure to address infection control deficiencies effectively and permanently can result in residents’ deaths. Andbe Home, a Kansas nursing facility, was cited with a no-harm infection control deficiency at its standard survey on December 18, 2018. The facility was cited with an immediate jeopardy deficiency in infection control on May 20, 2020 (as shown on both QCOR and CMS’s September 30, 2020 data release). Although the facility claimed to have promptly corrected the deficiencies, as of October 21, 2020, all 62 residents at the facility and many staff were infected with coronavirus and 10 residents had died.[1] QCOR does not reflect that the facility received a fine for its infection control deficiency (as of October 22). |
On October 9, the Center searched QCOR for infection prevention and control deficiencies (F-880), at the immediate jeopardy level that had been cited since January 2020. QCOR identified 384 deficiencies as meeting these criteria. Analyzing a 20% sample of the data (59 of the 294 facilities),[3] the Center found:
- 11 of the 59 facilities did not have any survey in calendar year (CY) 2020
- 23 of the 59 nursing facilities had a survey in CY 2020, but they were not cited with an infection control deficiency
- Only 29 infection control deficiencies were cited in CY 2020
- Only 25 nursing facilities cited 29 infection control deficiencies in CY 2020
Eighteen of the 29 infection prevention and control deficiencies (62%) identified in QCOR were cited at the immediate jeopardy level. The immediate jeopardy deficiencies were cited in 18 facilities, several of which were also cited with a non-immediate jeopardy deficiency in infection control.
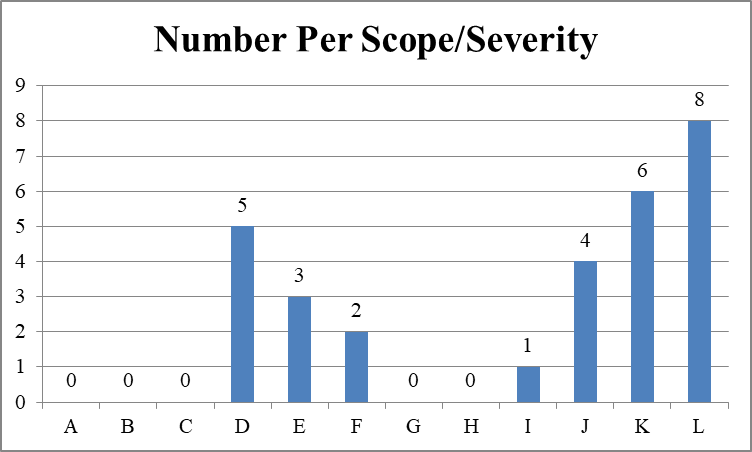
Expanding the 20% sample (18 times five) still means that only 90 facilities were likely cited with an immediate jeopardy deficiency in infection prevention and control since January 2020.
The Center looked at the sample of 25 nursing facilities with infection control deficiencies on Nursing Home Compare. One facility did not appear on Nursing Home Compare at all and another facility is a Special Focus Facility and, therefore, does not have star ratings.
Health ratings of 23 nursing facilities cited with infection control deficiencies
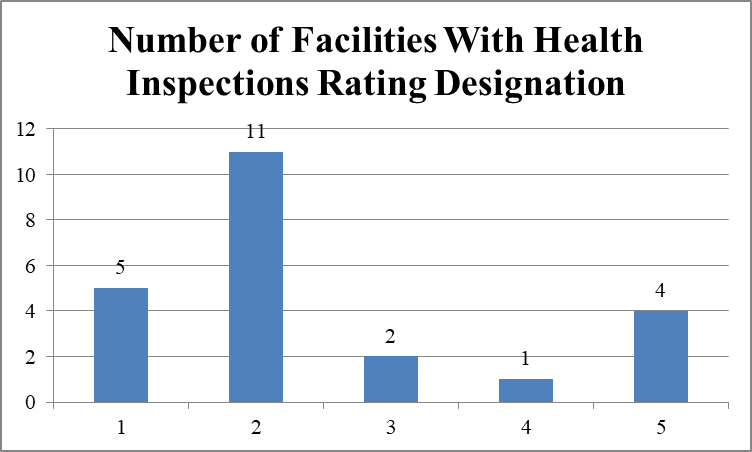
Facilities identified in QCOR as having immediate jeopardy deficiencies in infection control had poor records for quality of care. Sixteen of 23 facilities (69.6%) have one or two stars in health inspections; five of 23 facilities (21.7%) have four or five stars.
Staffing ratings of 23 nursing facilities cited with infection control deficiencies
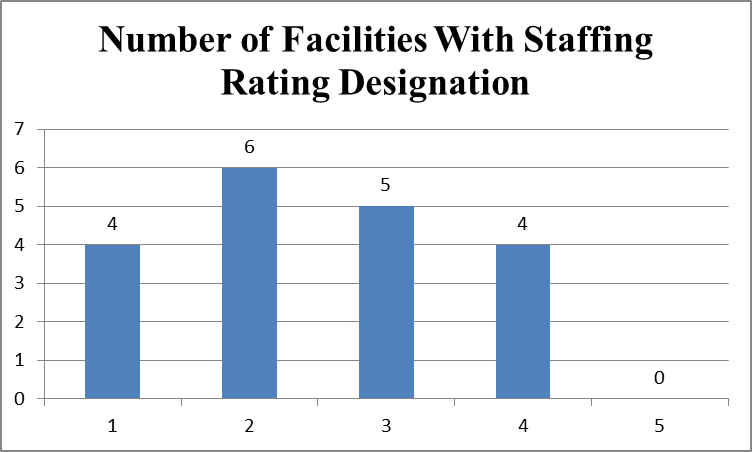
Facilities identified in QCOR as having immediate jeopardy deficiencies in infection control also had poor staffing levels. Ten of 23 facilities (43.5%) have one or two stars in staffing; four of 23 facilities (17.4%) have four stars in staffing; four facilities do not have staffing ratings. No facility has five stars in staffing.
Quality measure ratings of 23 nursing facilities cited with infection control deficiencies
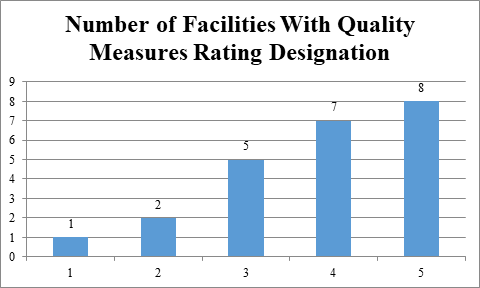
Facilities identified in QCOR as having immediate jeopardy deficiencies in infection control nevertheless self-report resident assessment data that makes them look good in the quality measure domain. Fifteen of 23 facilities (65.2%) have four or five stars in quality measures. These data document, again, that facilities’ largely self-reported quality measure data are inconsistent with the health inspection and staffing measures and make facilities look much better than they should.
Overall ratings of 23 nursing facilities cited with infection control deficiencies
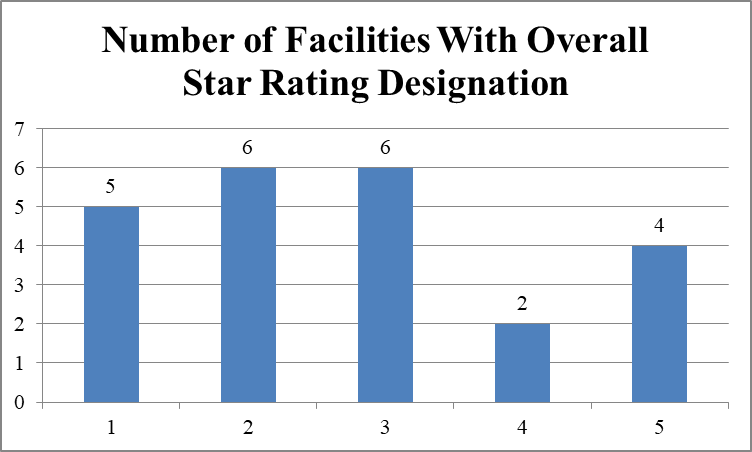
Eleven of 23 facilities (47.8%) have one or two stars in quality measures; six of 23 facilities (26.1%) have four or five stars in quality measures.
Penalty History
Eight of the 24 facilities (33.3%) had civil money penalties imposed in the prior three years, according to Nursing Home Compare; the fines averaged $56,692.13 and totaled $453,537. The Special Focus Facility was fined $166,183. Sixteen of the 25 facilities (66.7%) had no fines in the prior three years.
A total of six denials of payment for new admissions (DPNA) had been imposed at the 24 facilities in the prior three years. The Special Focus Facility had three DPNAs; one facility had two DPNAs; and one facility had one DPNA.
QCOR and CMPs
QCOR also separately identifies civil money penalties (CMPs) that are imposed for infection prevention and control deficiencies. Comparing the QCOR deficiency data with the QCOR CMP data, the Center found that 14 of the 25 facilities (56%) with infection control deficiencies had CMPs. Thirteen facilities had per day CMPs imposed, totaling $1,348.397.75; one facility had two per instance CMPs, totaling $21,768.50. Nursing Home Compare does not report CMPs for facilities that are appealing the deficiencies and CMPs.
- Of the 14 facilities with immediate jeopardy deficiencies in infection control, 11 had CMPs imposed and three did not.
- Of the seven facilities with only non-jeopardy deficiencies in infection control, three had CMPs imposed and four did not.
QCOR and CMS’s Fifth Cumulative Date Release of Focused Infection Control Surveys
On September 30, CMS made available on Nursing Home Compare its fifth cumulative release of focused infection control surveys, covering the period January-August 2020.[4] The Center compared the 75 facilities reported on Nursing Home Compare as having been cited with infection control deficiencies with the 25 facilities reported in the QCOR sample and found only 11 facilities listed in both databases.
Discussion/Conclusion
QCOR is inaccurate in its reporting of infection prevention and control deficiencies. While QCOR indicates that 384 immediate jeopardy infection control deficiencies had been cited since January 2020, the Center for Medicare Advocacy’s review of a 20% sample of the 384 deficiencies (i.e., 59 deficiencies) found that only 25 of 59 facilities were actually cited with an infection control deficiency. Expanding the 20% sample means that 125 facilities have been cited with an infection control deficiency. But only 18 of the 25 facilities were cited with an immediate jeopardy deficiency in infection control. Expanding that 20% sample means that 90 facilities have been cited with an immediate jeopardy infection control deficiency since January 2020, half the 180 facilities cited by CMS in August.
Enforcement of these deficiencies appears limited. QCOR data also show that only 11 of the 18 facilities (61%) cited with immediate jeopardy infection control deficiencies had CMPs imposed. It is possible that more CMPs have been imposed. Since QCOR reports only CMPs that are “final,” any CMPs that facilities have appealed are not listed.
Also troubling is the limited overlap between CMS’s two public databases, QCOR and Nursing Home Compare. Of the 18 facilities in the Center’s sample with immediate jeopardy deficiencies in infection control identified in QCOR, only ten facilities are reported in Nursing Home Compare.
Infection control deficiencies are rarely cited and, even if cited, they are not cited as immediate jeopardy and are not enforced. Proper enforcement could prevent unnecessary deaths.
___________________
[1] CMS, “Trump Administration Has Issued More Than $15 Million in Fines to Nursing Homes During COVID-19 Pandemic” (Press Release, Aug. 14, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-has-issued-more-15-million-fines-nursing-homes-during-covid-19-pandemic.
[2] CMA, “Responding to CMS Announcement on Nursing Home Enforcement – Infection Control Deficiencies in Nursing Facilities: QCOR Data” (CMA Alert, Aug. 20, 2020).
[3] The Center analyzed ## 1, 6, 11, and so on.
[4] CMA, “Special Report: CMS Releases Fifth Cumulative List of Focused Infection Control Surveys” (CMA Alert, Oct. 8, 2020), https://medicareadvocacy.org/special-report-cms-releases-fifth-cumulative-list-of-focused-infection-control-surveys/.
– top –
This week we honor and celebrate the Center for Medicare Advocacy’s pro bono partners, who support our mission of advancing access to Medicare and quality health care. Law firms that contribute their time, expertise, and resources expand the Center’s capacity to litigate on behalf of beneficiaries.
Today we highlight Wilson Sonsini Goodrich & Rosati, which has provided extraordinary assistance for several years on Alexander v. Azar, a nationwide class action. The case seeks appeal rights for Medicare beneficiaries who are placed on “observation status” at hospitals, a designation that can cost beneficiaries thousands of dollars. The Center’s partnership with Wilson Sonsini led to a successful trial last summer. The court made an important finding that Medicare coverage is protected by the U.S. Constitution and that the Medicare agency is violating the due process rights of many older adults and people with disabilities who are placed in “observation.” As the litigation continues on appeal, we remain grateful to Wilson Sonsini and the Alexander team for their ongoing assistance and unparalleled commitment to pro bono service.
– top –
