- Responding to CMS Announcement on Nursing Home Enforcement – Infection Control Deficiencies in Nursing Facilities: QCOR Data
- Advocates Support Nursing Home Residents’ Ability to Enforce Their Rights in Court
- Nursing Homes Nationwide Report Shortages of Nursing Staff
- Elder Justice Newsletter – Vol 2, Issue 12 Now Available
- Toolkit to Educate Candidates about Medicare Oral Health
On August 14, 2020, the Centers for Medicare & Medicaid Services (CMS) announced that it has cited many infection control deficiencies in nursing facilities at the immediate jeopardy level and that it has imposed civil money penalties as a result. According to CMS’s press release, the agency “imposed more than $15 million in civil money penalties (CMPs) across more than 3,400 nursing homes during the public health emergency for noncompliance with infection control requirements and failure to report coronavirus disease 2019 (COVID-19) data.”[1]
CMS said that infection control surveys during the current coronavirus pandemic yielded “more than 180 immediate jeopardy level findings for infection control, which is triple the rate of such deficiencies found in 2019.”[2] In an August 19, 2020 call with nursing home residents’ advocates, CMS said that the data reported on August 14 are, at present, available only in an internal CMS database; they have not yet been reported on publicly-reported databases.
The Center for Medicare Advocacy (the Center) has been analyzing and reporting publicly-available data about infection prevention and control surveys and deficiencies from two CMS databases: the targeted infection control surveys linked through Nursing Home Compare, which is updated on the last Wednesday of each month, and Quality, Certification and Oversight Reports (QCOR) which is updated weekly. These databases report far fewer immediate jeopardy infection control deficiencies than appear in CMS’s internal database.
- One in 5,724 surveys – From initial June 4, 2020 CMS data release[3]
- Four in 9,899 surveys – From June 24, 2020, CMS data release (cumulative)[4]
- 23 in 16,987 surveys – From July 29, 2020, CMS data release (cumulative)[5]
- 27 (from March 2020-July 24, 2020) – From July 24, 2020, evaluation of QCOR data[6]
QCOR Data: Deficiencies
On August 17, 2020, the Center looked at QCOR and searched for infection prevention and control deficiencies (F-880), at the immediate jeopardy level, that were cited since January 2020. (QCOR reports data by calendar year or fiscal year). QCOR identified 176 deficiencies as meeting these criteria. However, when analyzing the data, the Center found:
- Only 153 nursing facilities were cited
- 28 of the 153 nursing facilities did not have any survey in 2020
- 44 of the 90 nursing facilities had a survey in 2020, but they were not cited with an infection prevention and control deficiency
- Only 69 nursing facilities cited 81 infection prevention and control deficiencies in calendar year 2020
Fifty-five nursing facilities were cited with 59 infection prevention and control deficiencies since March 2020, according to QCOR. Fifty-two of the 59 deficiencies (88.1%) were cited at the immediate jeopardy level.
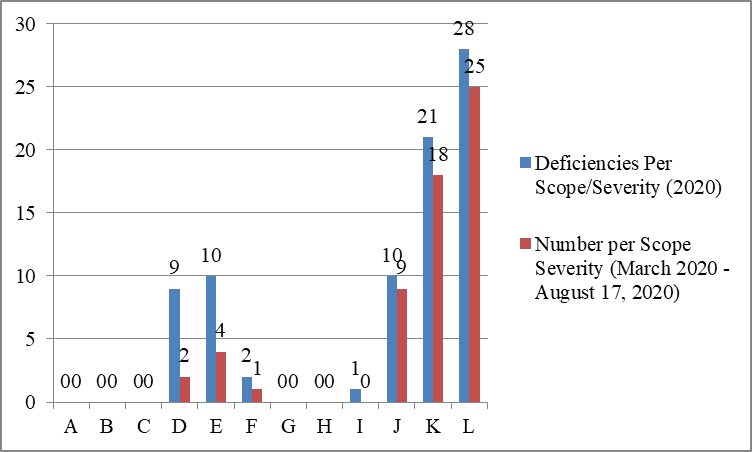
The bar graph below reflects the severity of the infection prevention and control deficiencies cited since March 2020. Twenty-five immediate jeopardy deficiencies were considered widespread, affecting many residents.
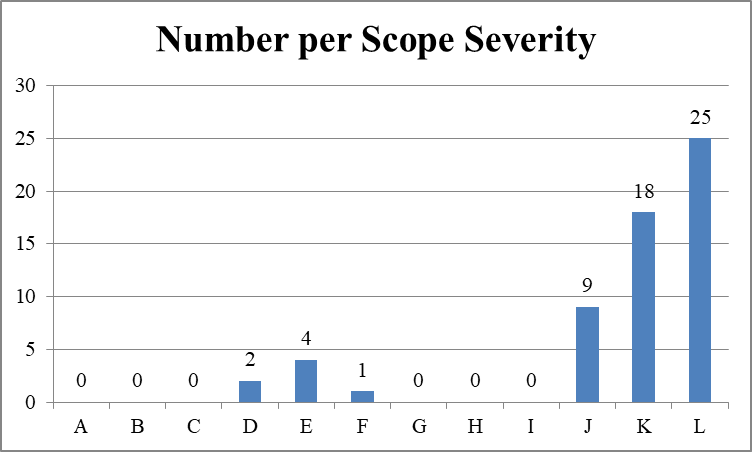
A larger portion of infection control deficiencies cited since March were cited as immediate jeopardy than deficiencies cited for the calendar year 2020, to date. Fifty-two of the 59 deficiencies (88.1%) cited since March were cited at the immediate jeopardy level. Fifty-nine of the 81 deficiencies (72.8%) cited for calendar year 2020, to date, were cited at the immediate jeopardy level.
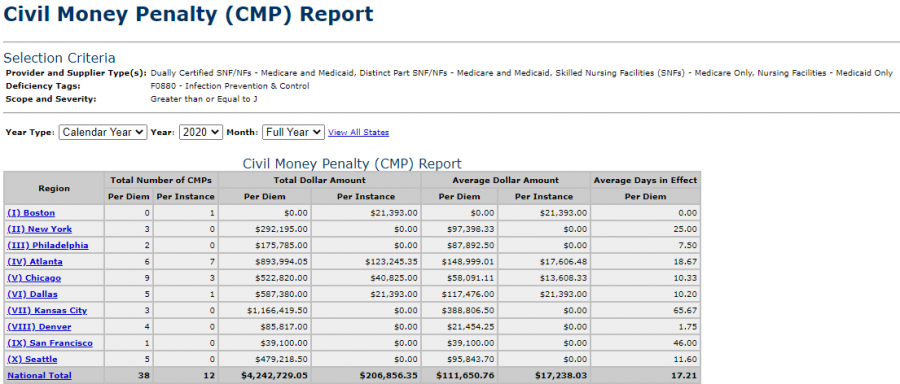
QCOR Data: Civil Money Penalties
QCOR also allows users to search for civil money penalties (CMPs) that are in effect. The Center’s August 19 search for CMPs imposed in calendar year 2020, to date, for immediate jeopardy infection control deficiencies found 50 CMPs – 38 per day CMPs totaling $4,242,729.05 (and averaging $111,650.76) and 12 per instance CMPs totaling $206,856.35 (and averaging $17,238.03), far fewer than the 180 CMPs reported by CMS on August 14.
Conclusion
QCOR data show only a small portion of the infection control immediate jeopardy deficiencies and Civil Monetary Penalties that CMS reported on August 14, 2020. The CMS data should be open and available to keep the public fully informed about these important matters.
__________________
[1] CMS, “Trump Administration Has Issued More Than $15 Million in Fines to Nursing Homes During COVID-19 Pandemic” (Press Release, Aug. 14, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-has-issued-more-15-million-fines-nursing-homes-during-covid-19-pandemic.
[2] CMS, “Trump Administration Has Issued More Than $15 Million in Fines to Nursing Homes During COVID-19 Pandemic” (Press Release, Aug. 14, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-has-issued-more-15-million-fines-nursing-homes-during-covid-19-pandemic.
[3] Center for Medicare Advocacy, “Special Report Infection Control Surveys at Nursing Facilities: CMS Data are Not Plausible” (Jun. 11, 2020), https://medicareadvocacy.org/wp-content/uploads/2020/06/Infection-Control-Surveys-Report.pdf.
[4] Center for Medicare Advocacy, “Special Report Infection Control Surveys at Nursing Facilities Reported Released by CMS in June 2020: Few Deficiencies, Most Called “No Harm;” Poor Ratings on Nursing Home Compare” (Jun. 24, 2020, https://medicareadvocacy.org/wp-content/uploads/2020/08/Special-Report-Infection-Control-Cumulative-6.24.20.pdf.
[5] Center for Medicare Advocacy, “Special Report Infection Control Surveys at Nursing Facilities Reported Released by CMS in July 2020: Few Deficiencies, Most Called ‘No Harm’” (Aug. 6, 2020), https://medicareadvocacy.org/wp-content/uploads/2020/08/Special-Report-Infection-Control-Cumulative-7.29.20.pdf.
[6] Center for Medicare Advocacy, “Special Report Infection Control Deficiencies In Nursing Facilities: QCOR Data” (Aug. 6, 2020), https://medicareadvocacy.org/wp-content/uploads/2020/08/Special-Report-SNF-Infections-QCOR-Data.pdf.
– top –
Advocates Support Nursing Home Residents’ Ability to Enforce Their Rights in Court
On August 7, 2020, the Center for Medicare Advocacy joined AARP, the National Consumer Voice for Quality Long-Term Care, and other advocates in an amicus brief submitted in Talevski v. Health and Hosp. Corp. of Marion Cnty. Corp., et al. The amicus brief supports a private right of enforcement for residents of state-run facilities under the Nursing Home Reform Act (NRHA). The NHRA mandates that nursing homes maintain minimum standards of care and it includes a “Residents’ Bill of Rights.” Those rights include freedom from abuse and neglect, freedom from illegal discharges, and freedom from chemical restraints administered for staff’s convenience. As explained in the advocates’ amicus brief, these legal rights “are a matter of life and death for nursing facility residents. Even today, residents still experience abuse, neglect, and dangerously poor care in many facilities.” The COVID-19 pandemic has only exacerbated the vulnerability of nursing home residents, as the virus has infected facilities and visitation restrictions have limited contact with the family members and advocates who usually play a key role in protecting residents.
The mere existence of rights in the law is not sufficient and regulatory oversight has proven to be inadequate. Residents must be able to go to court to hold nursing homes accountable. The Center’s joint amicus brief urges the Seventh Circuit to join the Third and Ninth Circuit Courts of Appeal in holding that residents can bring an action under Section 1983 of the Civil Rights Act against state-run facilities to enforce violations of the Nursing Home Reform Law.
– top –
Nursing Homes Nationwide Report Shortages of Nursing Staff
Last week, CMA released an Alert reporting on four recent studies that found a positive correlation between nurse staffing levels and improved nursing home performance in containing COVID-19 cases and deaths. Nursing homes in every state, along with Washington, DC, however, are informing CMS in parallel that they have a shortage of those valuable nurse resources.[1]
According to the latest release of CMS’s COVID-19 Nursing Home Data set, 15.7% of all nursing homes nationwide reported a nurse staff shortage.[2] The percentage of state-level nurse staff shortages ranged from 29.7% (Alabama) to 1% (California). Fourteen states reported that between 20.1%-29.7% of their nursing home facilities were suffering from nursing staff shortages, potentially negatively impacting their ability to contend with a still-growing pandemic.
Furthermore, 234 nursing homes across 40 states in the nation reported a staff shortage across all available categories (nursing, clinical, aides, and other). Of those states, Texas has the greatest number of nursing homes reporting across the board staff shortages (41 facilities), while Ohio came in second with 21 facilities. According to CMS, Texas falls within the highest bracket of total resident cases by state with over 13,300 cases.
______________
[1] Drawn from the CMS COVID-19 Nursing Home Data set (https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/) ending the week of August 2, 2020. 2,237 out of 14,256 nursing homes reported nurse staff shortages from July 27 – August 2, 2020.
[2] The COVID-19 Nursing Home Data set filtered to remove nursing homes surveys that did not pass the CMS quality assurance check
– top –
Elder Justice Newsletter – Vol 2, Issue 12 Now Available
Elder Justice: What “No Harm” Really Means for Residents is a newsletter published by the Center for Medicare Advocacy and the Long Term Care Community Coalition. The purpose of the newsletter is to provide residents, families, friends, and advocates information on what exactly a “no harm” deficiency is and what it means for nursing home residents. Our latest issue has real stories from nursing homes in New York, Illinois, and Kansas.
- Read the latest issue at: https://medicareadvocacy.org/wp-content/uploads/2020/08/Elder-Justice-Vol.-2-Issue-12.pdf
– top –
Toolkit to Educate Candidates about Medicare Oral Health
The Oral Health Progress and Equity Network (OPEN) has developed a new Medicare Dental Toolkit to help educate candidates about the importance of oral health for Medicare beneficiaries. Access the full toolkit here.
Please also join us on September 2nd for OPEN’s Virtual Day of Action with a Twitter Chat at 2pm ET – @OPENoralhealth.
- More information on OPEN: https://medicareadvocacy.org/new-oral-health-advocacy-collaborative-begins/
– top –
